
Am Fam Physician. 1999;60(6):1687-1696
Anterior hip pain is a common complaint with many possible causes. Apophyseal avulsion and slipped capital femoral epiphysis should not be overlooked in adolescents. Muscle and tendon strains are common in adults. Subsequent to accurate diagnosis, strains should improve with rest and directed conservative treatment. Osteoarthritis, which is diagnosed radiographically, generally occurs in middle-aged and older adults. Arthritis in younger adults should prompt consideration of an inflammatory cause. A possible femoral neck stress fracture should be evaluated urgently to prevent the potentially significant complications associated with displacement. Patients with osteitis pubis should be educated about the natural history of the condition and should undergo physical therapy to correct abnormal pelvic mechanics. “Sports hernias,” nerve entrapments and labral pathologic conditions should be considered in athletic adults with characteristic presentations and chronic symptoms. Surgical intervention may allow resumption of pain-free athletic activity.
Anterior hip pain is a common problem that is frequently difficult to diagnose and treat.1 Determining the exact cause of hip pain can be difficult for several reasons. The multiple structures in the hip have the potential to produce similar pain syndromes; in addition, pain in the hip region may come from deep structures that are not palpable. Pathologic conditions ranging from a benign muscle or tendon strain to a potentially catastrophic femoral neck stress fracture can have similar clinical presentations.
This article reviews many of the hip problems in adolescents and adults that present with anterior pain (Table 1). Conditions of the lumbar spine that radiate pain to the anterior hip are not discussed. A brief review of hip pain in adolescents is included.
| Condition | Presentation | Examination findings | Imaging and diagnostic studies | Basis of diagnosis | Treatment |
|---|---|---|---|---|---|
| Osteoarthritis | Groin pain on activity; gradual worsening of pain; limp | Pain and decreased range of motion on internal rotation and extension | Radiographs: joint space narrowing, sclerosis, osteophytes | Clinical findings, confirmed with radiographs | Initially, oral analgesics and exercise |
| Joint arthroplasty for end-stage disease | |||||
| Inflammatory arthritis | Pain in the morning; activity limitation; systemic involvement | Generalized joint involvement; enthesopathy; skin or bowel symptoms | Elevated erythrocyte sedimentation rate and C-reactive protein level Arthrocentesis: white blood cell count in joint fluid of mm3 Radiographs: erosions, osteopenia | Clinical and laboratory findings Significant improvement with NSAIDs | NSAIDs and exercise; with disease progression, antirheumatic drugs |
| Muscle and tendon strains | Acute mechanism; localized pain occurring immediately | Local swelling and tenderness, ecchymosis, weakness | MRI or ultrasonography | Clinical findings with imaging if needed | Rest, ice, compression, progressive rehabilitation |
| Address errors in training, technique and mechanics. | |||||
| Tendonitis | Overuse; delayed onset, pain localized and worsening with activity | Local swelling and tenderness, crepitus “snapping,” weakness | MRI or ultrasonography | Clinical findings with imaging if needed | Same as for strains |
| Femoral neck stress fracture | Impaired bone metabolism; overuse; worsening hip and thigh pain; progressive limitation of activity | Pain on internal rotation and with hopping; regional muscle guarding | Radiographs: often normal | Confirmed with imaging | Nonweight-bearing; urgent orthopedic referral for displaced fracture |
| Bone scans: highly sensitive | |||||
| MRI: better specificity than bone scans | |||||
| Sports hernia (occult hernia or tear of oblique aponeurosis) | Chronic groin pain (i.e., particularly common in soccer, rugby and ice hockey); pain worse with “cutting” and sprinting | Tenderness at superficial inguinal ring | Herniography may identify occult hernia. | Clinical findings | Herniorrhaphy |
| Repair of aponeurosis | |||||
| Obturator or ilioinguinal nerve entrapment | Same as for sports hernia but with adductor weakness or spasm | Adductor tenderness; decreased sensation | Electromyelography Obturator nerve block | Clinical findings and diagnostic tests | Surgical release of fascial entrapment of nerve |
| Osteitis pubis | Midline pubic pain with radiation to hip; pain worse with striding and pivoting | Direct tenderness; painful adduction; limited rotation and obliquity | Radiographs: widening of symphysis; sclerosis; cyst formation Bone scans “hot” over symphysis | Clinical and imaging findings | Seven to 10 months of rest, along with hip adductor and rotator stretching |
| Address sacroiliac function. | |||||
| Acetabular labral tears | Injury; chronic deep, sharp hip pain; intermittent “catch” or “giving way” of the hip | Tenderness on internal rotation and extension; click on Thomas test | Magnetic resonance arthrography | Clinical and imaging findings | Hip arthroscopy |
| Relief of pain with injection of local anesthetic |
Definitions
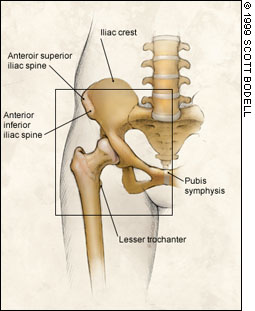
In this article, the term “anterior hip pain” is applied to symptoms extending medially to the pubic symphysis, laterally to the anterior superior iliac spine, superiorly to the lower abdomen and inferiorly to the proximal 5 to 10 cm of the anterior thigh (Figure 1). The term “groin” refers to the inferomedial aspect of the anterior hip.
Adolescents
Although adults and adolescents have many of the same hip problems, special consideration must be given to skeletal immaturity in young persons. Open physes are weaker than surrounding bone or tendon and are therefore susceptible to acute and chronic injuries.
APOPHYSEAL INJURY
In the adolescent, acute muscle contraction about the hip can result in avulsion of an apophysis (an ossification center at the attachment of tendon to bone). Whereas overuse is likely to result in tendonitis in an adult, it is more likely to cause apophysitis in the adolescent. Muscles with pelvic apophyseal attachments are illustrated in Figure 1 and listed in Table 2.
| Muscles | Apophyseal attachment |
|---|---|
| Internal and external obliques | Iliac crest |
| Sartorius | Anterior superior iliac spine |
| Rectus femoris | Anterior inferior iliac spine |
| Hamstrings* | Ischium |
| Iliopsoas | Lesser trochanter |
Symptoms of acute apophyseal injury include localized pain and swelling over the affected area, muscle weakness and limited range of motion. Radiographs should be obtained as part of the initial evaluation of suspected apophyseal injuries. Nondisplaced or minimally displaced fractures can be treated conservatively.2 However, if displacement is present, orthopedic referral is recommended because the degree of displacement warranting open reduction and external fixation remains unclear.3
Initial conservative treatment includes ice application, rest and relaxation of the involved tendon. Gradual pain-free range of motion is initiated as tolerated. Crutches may be used to assist with ambulation for up to three weeks as pain-free range of motion is achieved. Local treatment modalities, including application of ice, heat, electrical stimulation and ultrasound, may be useful. Gentle, progressive resistance training should follow.
Limited sports participation, as tolerated, is possible by four to eight weeks after the injury. A return to competitive activity can be considered after eight to 10 weeks if the radiographs demonstrate maturing callous, range of motion and strength are normal, and participation in the sport-specific activity causes no pain.4
EPIPHYSEAL INJURY
Adolescents are also at risk for epiphyseal injuries in response to acute or chronic trauma. Slipped capital femoral epiphysis is a developmental injury that must be considered in any adolescent who presents with hip pain. Symptoms are not always related to a specific event. Typically, overweight male adolescents who are in a period of rapid growth present with hip pain, medial knee pain or a limp. In most patients, pain occurs with passive internal rotation of the flexed hip.
In patients with slipped capital femoral epiphysis, anteroposterior (AP) and frog-leg lateral radiographs demonstrate physeal widening with or without medial displacement of the femoral head. Depending on the severity of the injury, there may appear to be superior migration of the femoral neck at the level of the physis.
When slipped capital femoral epiphysis is diagnosed, all weight should be taken off the affected hip, and the patient should be referred immediately to an orthopedist for surgical stabilization. The contralateral hip should also be evaluated, because bilateral injury is present in as many as 40 percent of patients.5
Adults
ARTHRITIS
Arthritis is a disease state characterized by joint inflammation. Osteoarthritis is the most common cause of anterior hip pain in patients over 50 years of age, whereas inflammatory arthritis can affect patients of any age.6
Osteoarthritis of the hip joint generally presents with fairly steady pain that becomes more severe as the disease advances. Progressively worsening pain with activity is common, and a painful, limping gait generally develops. Pain is worse initially with full internal rotation and extension of the hip, and hip range of motion is progressively lost.
Radiographically, osteoarthritis is identified by unequal cartilage loss (i.e., joint space narrowing) on one side relative to the other. Normal hips should have 4 mm of cartilage space with a difference of less than 1 mm from side to side.6
Treatment initially entails orally administered analgesics and activity modification (e.g., avoidance of high-impact activities) combined with an exercise prescription. Aerobic exercise, flexibility and resistance training, and joint range of motion exercises can decrease swelling and pain, thereby improving function in patients with osteoarthritis.7 Total joint arthroplasty is indicated when pain and activity limitation become unacceptable despite conservative treatment.
Pain is also a presenting complaint in many inflammatory arthritides, including seronegative spondyloarthropathies (ankylosing spondylitis, Reiter's syndrome, psoriatic arthropathy and enteropathic arthropathy), crystalline arthropathies (gout and pseudogout) and rheumatoid, viral and septic arthritis. Typically, the pain is worse in the morning and improves with activity, although activity limitation also occurs. A careful history should be obtained to pinpoint other joint involvement, enthesopathy (tendinous pain and inflammation at the site of muscle insertion), associated skin disease, systemic symptoms, eye problems, sexually transmitted diseases, inflammatory bowel disease and a family history of inflammatory disease. Many patients report that anti-inflammatory medication significantly alleviates their pain.
Radiographs may demonstrate diffuse joint involvement, symmetric narrowing of the joint space, osteopenia, erosions and a characteristic absence of osteophytes.8 Elevations of the white blood cell count, erythrocyte sedimentation rate and C-reactive protein level often accompany active inflammatory disease. When joint fluid is obtainable, the aspirate can be assessed for cell count and crystals. If infection is a concern, the aspirate can be cultured. Generally, a white blood cell count in joint fluid of 2,500 to 50,000 per mm3 is considered within the inflammatory range.
Treatment begins with anti-inflammatory drugs, activity modification and exercise training. If the disease progresses, anti-rheumatic drugs such as hydroxychloroquine (Plaquenil) or sulfasalazine (Azulfidine) can be highly effective and may help patients resume desired activity levels. Hydroxychloroquine is generally administered orally in a dosage of 3 mg per kg twice daily, and sulfasalazine is given orally in a dosage of 250 to 1,500 mg twice daily with meals. Patients treated with hydroxychloroquine must be monitored for maculopathy, and those treated with sulfasalazine must be monitored for leukopenia. Treatment with methotrexate (Rheumatrex), gold sodium thiomalate (Myochrysine) or azathioprine (Imuran) may also be considered. To effectively use these medications, physicians need to be familiar with their properties and side effects, as well as recommended monitoring.
STRAINS AND TENDONITIS
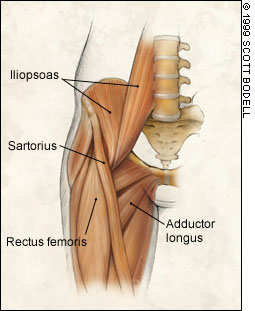
A strain is an acute injury to a muscle or tendon. In contrast, “tendonitis” is the term for acute inflammatory tendon changes secondary to overuse. In the anterior hip, the muscles most likely to be acutely or chronically injured are the rectus abdominis, iliopsoas, adductor longus and rectus femoris.1 Most often, the injuries occur at the muscle-tendon junction.
Acute injuries secondary to violent muscle contraction or stretch generally present abruptly with pain that increases with continued activity, swelling and ecchymosis. Chronic injuries (tendonitis) often present insidiously with increasing activity intolerance in a setting of relative overuse. The physical examination may reveal swelling or ecchymosis, along with local tenderness or crepitus (tendonitis) when more superficial structures are involved. Findings also include pain and loss of flexibility during passive stretch, and pain and weakness during muscle contraction against resistance.
In patients with iliopsoas tendonitis, which is also known as “internal snapping hip,” a “snap” or deep “clunk” may be heard over the tendon at the hip flexor crease as the hip moves from flexion to extension. The clunk is secondary to snapping of the iliopsoas tendon medially to laterally across the femoral head or, less frequently, the iliopectineal eminence. Inflammation of the iliopsoas bursae may play a role in tendonitis.
The diagnosis of strains depends on the characteristic clinical findings. The affected muscle or tendon can be identified based on the anatomic location of the pain (Figure 2) and the pattern of pain and weakness on manual muscle testing (Table 3). Tissue disruption in acute strains is graded as I (mild), II (moderate) or III (complete). If a bony avulsion is suspected, radiographs should be obtained. Magnetic resonance imaging (MRI) and diagnostic ultrasonography can demonstrate muscle and tendon injury, but these examinations are not indicated when the clinical presentation is diagnostic.
| Muscle | Pain with resistance |
|---|---|
| Rectus abdominis | Trunk flexion |
| Rectus femoris | Knee extension and hip flexion |
| Iliopsoas | Hip flexion and, sometimes, internal rotation |
| Adductor longus | Hip adduction |
For acute strains, treatment initially consists of rest, application of ice, compression and avoidance of painful activity. Crutches are helpful if ambulation causes significant pain. Gentle pain-free stretching and the use of ice, heat and other treatment measures should follow. Strengthening exercises, general endurance training and sports-specific activity should precede a full return to sports participation. Surgical treatment is generally not recommended, even for complete tears. Muscle tissue is not amenable to surgical repair, and most injuries occur at the muscle-tendon junction.
Tendonitis requires similar conservative treatment, although the initial period of disability is generally not as great. Rehabilitation should also include scrutiny of the training program that led to the problem, correcting poor technique that may be causing tissue overload and addressing regional biomechanical dysfunction.9
STRESS FRACTURE
Stress fractures result from chronic repetitive forces. They occur when the absorption of bone exceeds metabolic repair during the bone remodeling process in response to repetitive mechanical loads. This metabolic imbalance can occur secondary to increased mechanical loads from high levels of training or secondary to interference with the bone's remodeling capacity by various insults, including drugs that affect bone metabolism (e.g., glucocorticoids), nutritional deficiencies (e.g., calcium, vitamin D) or a hypoestrogenic state (e.g., after menopause, athletic amenorrhea). Stress fractures of the pubic ramus, femoral neck or proximal femur can cause anterior hip pain. Athletes at highest risk for these fractures include distance runners, jumpers, ballet and aerobic dancers, and triathletes.10,11
Femoral stress fractures, particularly those of the femoral neck, are worrisome because of the possibility of progression to displacement and osteonecrosis of the femoral head. Athletes with these injuries generally complain of proximal anterior thigh pain or anterior hip pain that initially occurs late in activity, eventually limits activity and finally occurs with any weight-bearing or at rest. Early findings on the physical examination include painful, possibly limited internal rotation of the hip and pain when the patient hops on the affected leg.11 With more severe stress fractures, limping and night pain may be present. If a femoral neck injury is suspected, all weight should be removed from the hip, and further imaging studies should be obtained as soon as possible.
Radiographs, including an AP view and a cross-table lateral or frog-leg view, may demonstrate a fracture line or, more likely, a region of lucency or increased sclerosis (a later finding) over the stress injury. Radiographic changes typically lag behind the onset of symptoms.
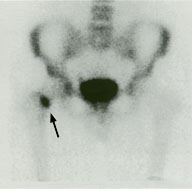
Bone scanning has been the study of choice for stress fractures but is being replaced by MRI in a number of centers. Compared with bone scanning, MRI has a similar sensitivity but an improved specificity for stress fractures.12 MRI is less invasive than bone scanning and can provide additional diagnostic information about the surrounding soft tissue. However, MRI is generally more expensive than bone scanning and requires technicians and physicians who are experienced with musculoskeletal protocols and MRI interpretation.
Treatment depends on the extent and location of a femoral neck stress fracture. Because of the potential for significant complications, referral to an orthopedist or sports medicine physician is generally advised. Urgent open reduction–internal fixation is recommended for fractures with displacement. The treatment of nondisplaced fractures depends on the side of the femoral neck on which the fracture is located.
If MRI scans indicate that inferior or medial neck fractures (which are compressed with weight-bearing) involve less than 50 percent of the femoral neck, initial conservative treatment is possible. With this approach, all weight is kept off the affected hip until the patient is completely free of pain. Activity is then resumed gradually as tolerated.
Percutaneous fixation is recommended when a fracture line involves more than 50 percent of the femoral neck or the fracture involves the superior or lateral side of the femoral neck.13 Because superior neck fractures are under tension with weight-bearing, they should be treated aggressively in most patients. Some authorities, however, recommend conservative treatment for superior nondisplaced stress fractures.14 Those who favor a more aggressive approach do so because of the morbidity associated with the prolonged bed rest (three weeks) and partial weight-bearing (up to 14 weeks) recommended for nonoperative treatment.
Illustrative Case
A 35-year-old male endurance runner presented with proximal anterior thigh pain on activity and during the night. These symptoms had been present for three weeks and had forced the patient to stop training. Radiographs demonstrated possible cortical disruption of the superior cortex but were not diagnostic. The bone scan was interpreted as highly suspicious for a femoral neck stress fracture (Figure 3). MRI scanning confirmed the diagnosis and clearly demonstrated involvement of the entire femoral neck (Figure 4). Because of the extent of the stress fracture, three percutaneous screws were placed (Figure 5).


SPORTS HERNIA AND NERVE ENTRAPMENT
It is widely accepted that femoral and inguinal hernias can cause anterior hip pain. However, increased attention is being given to nonpalpable hernias, often referred to as “sports hernias.” These injuries are thought to be responsible for chronic groin pain in athletes, particularly soccer, rugby and ice-hockey players. Suspected causes include weakness along the posterior aspect of the abdominal wall with occult direct or indirect hernia,15,16 injury or avulsion of the internal oblique muscle or fascia,17 tearing of the external oblique muscle and aponeurosis with ilioinguinal nerve entrapment,18 and fascial obturator nerve entrapment.19
Patients with nonpalpable (occult) hernias generally have a history of chronic activity-related groin pain. In patients with nerve entrapment, pain or numbness in the appropriate nerve distribution has been reported.18 Inguinal examination may demonstrate pain at the superficial ring. Imaging, with the possible exception of herniography (Figure 6) or ultrasonography to identify occult hernias, has not proved useful.20 If the diagnosis is not confirmed by herniography, it is made at surgery, which is eventually undertaken in patients with typical presentations who fail to improve despite generally long courses of conservative management.

Identified occult hernias are treated with herniorrhaphy. In one series, 90 percent of patients were able to return to full activity following this procedure.15 Surgical repair of the torn external oblique muscle with ablation of the ilioinguinal nerve18 and surgical release of the obturator nerve19 have also been successful in patients with painful nerve entrapment. At this time, sports hernias are not universally accepted as a cause of chronic groin pain.21 Nonetheless, based on current literature, sports hernias and nerve entrapments should be considered in the differential diagnosis of unremitting activity-related groin pain, especially in athletes who participate in high-risk sports.
OSTEITIS PUBIS
Osteitis pubis is a syndrome characterized by pain and bony erosion of the symphysis pubis. Historically, this condition has been considered an infectious complication of pelvic infection and instrumentation or a complication of excessive pubic symphysis mobility during pregnancy. More recent reviews in athletes have identified a predominance of patients with a mechanical etiology and a smaller number of patients with an obstetric or inflammatory etiology.22 The syndrome occurs most often in soccer, rugby, tennis and ice-hockey players, with males affected more often than females.
Patients with osteitis pubis generally present with pain over the pubic area that radiates laterally across the anterior hip. The pain is usually aggravated by striding, kicking or pivoting. Examination findings suggesting the diagnosis include tenderness over the symphysis and proximal adductors, pain with adduction against resistance, and restricted hip rotation with pelvic obliquity and sacroiliac dysfunction.23
In the well-developed syndrome, radiographs may demonstrate symphysis widening, cystic changes and sclerotic changes (a later finding). “Flamingo” views (i.e., AP radiographs of the pelvis with the patient standing on one leg) may reveal instability of the pubic symphysis. Bone scanning, which is more sensitive than radiography, often demonstrates increased uptake over the symphysis and pubic ramus.
One review of 59 patients with osteitis pubis suggested that the average time to recovery is seven months in women and slightly less than 10 months in men.22 In this study, the degree of radiographic changes and the intensity of isotope uptake on bone scans did not predict symptom duration. Yet patients with increased early-phase uptake appeared to have a shorter duration of symptoms.
At this time, no good scientific evidence indicates that surgical intervention or injecting the symphysis with corticosteroids improves outcomes in patients with osteitis pubis. Recommended treatment includes rest from the aggravating activity as well as hip adductor and rotator stretching exercises. If pelvic obliquity and sacroiliac dysfunction are present, treatment should also include stretching, strengthening and mobilization techniques to correct the muscular imbalance and maximize functional pelvic stability.
ACETABULAR LABRAL TEARS
Like the shoulder, the hip has a fibrocartilaginous labrum, and tears of this structure can be responsible for chronic anterior hip pain (Figure 7). Symptoms may or may not follow a traumatic event. Patients with this injury generally have activity-related sharp groin and anterior thigh pain that often becomes worse with extension. They also have episodes of deep clicking and a feeling that the hip is “giving way.”24 The diagnosis of acetabular labral tear is generally considered in patients who have typical symptoms for more than six months despite receiving conservative treatment.
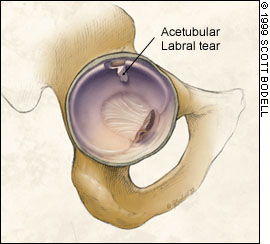
Clicking palpated on Thomas flexion-to-extension testing frequently correlates with the finding of labral tears at arthroscopy.24 For the Thomas test, the contralateral hip is flexed, and the symptomatic hip is moved from full flexion to full extension. Fluoroscopically guided intra-articular injection of a local anesthetic is also useful in diagnosing an acetabular labral tear.25 If the symptoms abate following the injection, an intra-articular etiology is much more likely.
Hip arthroscopy is currently the gold standard for the diagnosis of acetabular labral tears, as well as the preferred method of treatment. The procedure is technically difficult and requires specialized equipment but, when performed by an experienced surgeon, produces good results.29