
Am Fam Physician. 2007;75(3):361-367
Patient information: See related handout on amblyopia, written by the authors of this article.
Author disclosure: Nothing to disclose.
Amblyopia, a decrease in visual acuity, is a major public health problem with a prevalence of 1 to 4 percent in the United States. It is thought to develop early in life during the critical period of visual development. Early recognition of amblyogenic risk factors such as strabismus, refractive errors, and anatomic obstructions can facilitate early treatment and increase the chance for recovery of visual acuity. Multiple medical organizations endorse screening for visual abnormalities in children and young adults, yet only 20 percent of school-age children have routine vision screening examinations. Any child with a visual acuity in either eye of 20/40 or worse at age three to five years or 20/30 or worse at age six years or older, or a two-line difference in acuity between eyes, should be referred to an ophthalmologist for further evaluation and definitive therapy. Treatment is started at the time of diagnosis and depends on the etiology. Treatment options for children with strabismus include patching and atropine drops. Children with refractive errors should be prescribed corrective lenses. Corneal lesions, cataracts, and ptosis require surgery. The success of therapy is highly dependent on treatment compliance. Patients and their parents should be educated about the need for regular follow-up and the risk of permanent vision loss.
Amblyopia, often called “lazy eye,” is a decrease in visual acuity resulting from abnormal visual development in infancy and early childhood. The vision loss ranges from mild (worse than 20/25) to severe (legal blindness, 20/200 or worse). Although generally unilateral, amblyopia may affect both eyes. No apparent cause for the decreased vision can be detected on physical examination: the cornea, lens, retina, and optic disc are normal.
Amblyopia is a major public health problem with an estimated prevalence of 1 to 4 percent in the United States.1 It is the most common cause of monocular vision loss in children and young adults.2 Early recognition and prompt referral are crucial, especially during infancy and childhood, to prevent permanent loss of vision.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Screening for amblyopia should be performed early and regularly to prevent permanent loss of vision. | B | 5–14 |
| Patching and atropine (Atropisol) are effective treatments for amblyopia. | A | 16–22 |
| Educating patients and their parents is an integral component of amblyopia treatment. | B | 23 |
Etiology
Animal studies and clinical studies in infants and young children support the concept of a critical period during infancy and childhood for developing amblyopia.3,4 The developing brain is sensitive, and amblyopia may occur as early as the first weeks of life. The eyes and brain must work in conjunction for vision to develop correctly. If the visual pathways to the visual cortex are not properly stimulated, the visual cortex cannot mature appropriately. However, if amblyogenic risk factors are identified and treated early (i.e., during the critical period), the brain's plasticity is such that visual loss may be corrected.4
Several conditions may lead to amblyopia. Strabismus (i.e., ocular misalignment or heterotropia) causes the images on the retinas to be dissimilar; uncorrected refractive errors (i.e., anisometropia) or an impediment to the visual axis (e.g., cataracts) causes the images to be of unequal clarity. This displacement or distortion of the image prevents the development of fine visual perception in the occipital cortex and puts the child at risk for developing amblyopia.
Strabismus is by far the most common contributing factor. Amblyopia develops in the consistently deviating eye, which may turn inward (esotropia, or “cross-eye”), outward (exotropia), or vertically (hypertropia, as in congenital fourth nerve palsy; or hypotropia). In latent strabismus (heterophoria), deviations are detected only when one eye is occluded. Small, intermittent deviations are rarely associated with amblyopia. Children who can alternate fixation using one eye at a time usually do not develop amblyopia.
Refractive errors, the second most common contributing factor to the development of amblyopia, can be difficult to detect. Amblyopia resulting from refractive errors, is divided into two types: anisometropic and isometropic. Anisometropic amblyopia develops when the refractive errors in the two eyes are unequal. The difference in refraction, as well as the refractive error, causes the image to be out of focus on one retina, blunting the development of the visual pathway in the affected eye. Bilateral hyperopia (farsightedness) is the most common refractive error to cause amblyopia. Severe unilateral hyperopia, myopia (nearsightedness), and astigmatism also may cause profound vision loss. Isometropic amblyopia develops when the refractive errors in the two eyes are equal. Severe refractive errors in both eyes, even if symmetric, may cause bilateral isometropic amblyopia, especially if optical correction is delayed.
The least common amblyogenic condition, congenital or early-acquired media opacity, causes deprivation amblyopia. This often is the most severe and damaging type of amblyopia. Cataracts, corneal lesions, or ptosis block or distort the retinal image formation. Deprivation amblyopia can affect one or both eyes and may develop as early as two to four months of age. Occlusion amblyopia is a form of deprivation amblyopia caused by excessive therapeutic patching.
Screening
Studies have shown that early screening for amblyopia results in better outcomes.5,6 Countries that have instituted early vision screening programs have reduced rates of amblyopia.5,6 A systematic review found insufficient evidence to conclusively recommend screening in school-age children.7 However, multiple organizations (i.e., the American Academy of Family Physicians, the American Academy of Pediatrics [AAP], the American Academy of Ophthalmology, the American Association for Pediatric Ophthalmology and Strabismus, and the U.S. Preventive Services Task Force) endorse screening for visual abnormalities.8–10 Despite these recommendations, only about 20 percent of school-age children have routine vision screening examinations.11 A governmental task force concluded that there was a lack of data on the validity and effectiveness of the available screening programs.12 However, the panel determined that age-appropriate vision screening, as outlined by the AAP, should be a part of all well-child examinations.12
One method that may facilitate mass screening is the use of photoscreening. A camera or video system is used to photograph the eyes and red reflex, then the photographs are analyzed to detect amblyogenic risk factors such as strabismus, refractive errors, and media opacities.13 Photoscreeners have a reported sensitivity of 75 to 91 percent for the detection of amblyogenic risk factors14; however, they cannot detect amblyopia. Patients in whom risk factors are detected should be referred to an ophthalmologist for further evaluation. Photoscreening is not in widespread use for a variety of reasons, including inconsistent performance (especially in younger children) and high cost, but with further refinement it may prove to be a valuable screening tool in the future.13
Diagnosis
The diagnosis of amblyopia is made when there is evidence of reduced visual acuity that cannot be explained by physical abnormalities. Structural eye pathology, including optic nerve or macular lesions, media opacities, and abnormalities of the central visual pathways, should be excluded.
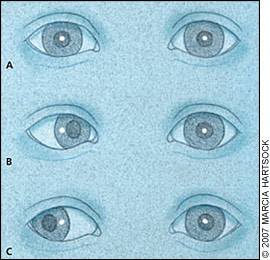
The evaluation begins with an ocular history based on the patient's age and parental observations. Parents are often the first to raise concerns about abnormalities such as difficulty seeing, an eye that drifts, or a head tilt. A vision assessment should be performed as part of the physical examination. The eyes and eyelids should be inspected for ptosis, corneal lesions, and cataracts. Extra-ocular movements and the red reflex should be examined carefully. Although the Snellen chart (Figure 1A) is the reference standard, the HOTV (Figure 1B), tumbling E, Lea (Figure 1C), and Allen (Figure 1D) charts can be used to test visual acuity in children as young as two or three years. A gross measure of visual acuity in young, preverbal children can be determined by their ability to visually follow an object placed before them.

If a visual acuity of 20/20 is not achieved on routine vision screening, then pinhole testing may be used to determine whether vision corrects to 20/20. Pinhole testing is useful in the primary care setting because it can help optimize vision. The child looks through a pinhole, using one eye at a time, while reading the age-appropriate vision chart. If a visual acuity of 20/20 is achieved, then a refractive error is present. If not, amblyopia must be considered. Any child with a visual acuity in either eye of 20/40 or worse at age three to five years or 20/30 or worse at six years or older, or a two-line difference in acuity between the two eyes, should be referred to an ophthalmologist for further evaluation (Table 1).9
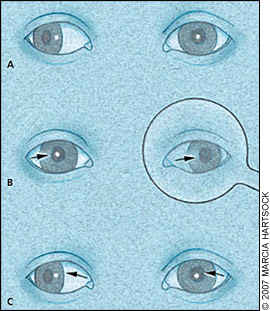
The corneal light reflex test may be performed at any age and can be particularly helpful in assessing ocular alignment in preverbal children (Figure 2). The test involves shining a light onto the child's eyes from a distance and observing the location of the light on the cornea with respect to the pupil. The location of the light reflection from both eyes (typically slightly nasal to the center of the pupil) should be symmetric. The presence of an esotropia after the age of two months (Figure 2B) or an exotropia after the age of six months (Figure 2C) suggests an abnormality, and further evaluation by an ophthalmologist is necessary.15
The cover-uncover test is used to detect the presence of strabismus, differentiating a tropia (i.e., deviation of an eye from the normal position when both eyes are open) from a phoria (i.e., latent deviation). The child fixates on an object at a specified distance—a near target or one about 10 feet (3 m) away. If one eye shows displacement of the corneal light reflex (Figure 3A), then the other eye is covered. In the presence of strabismus, the misaligned eye turns to fixate on the object indicating a tropia (Figure 3B), but when the good eye is uncovered, the weak eye drifts back to its original, strabismic position (Figure 3C). Just after the cover is placed over the eye, the physician should watch for movement in this eye. If the eye moves under the cover and there is movement in the opposite direction as the cover is removed (resulting from the interruption of binocularity), a phoria is present. The test must be repeated in the other eye. Irritability in a child while the good eye is covered suggests amblyopia, because the child receives no visual input from the weak eye and therefore cannot see.
If no movement is detected on the cover-uncover test, the alternate cover test should be performed. With the child focusing on a target, each eye is alternately covered. Any eye movement should prompt referral to an ophthalmologist.
A potential difficulty in the evaluation is the presence of pseudostrabismus—the appearance of strabismus despite normal alignment. The most common form is pseudoesotropia, which results from coverage of the nasal sclera by the wide, flat nasal bridge and epicanthus (i.e., epicanthal folds) common in infancy (Figure 4). Because no real deviation exists, the corneal light reflex and cover-uncover tests are normal.

Treatment
Treatment is individualized depending on the cause of amblyopia. Although treatment after age 10 years previously was thought to offer little benefit, results from a recent study suggest that treatment can improve visual acuity even in adolescence.16 Therefore, treatment should not be overlooked in children of this age group if amblyopia is suspected. The duration of therapy depends on the degree of vision loss and the rate at which the child regains vision. To maximize the image perceived by the retina, treatment must include attention to obstructing lesions (e.g., cataracts) and optical impediments to a good image (e.g., refractive errors). Then, the amblyopic eye must be forced to do the work of seeing. This is accomplished by limiting the stimulation of the other eye.
In children with strabismus, the most common technique used to stimulate the amblyopic eye is placement of an adhesive patch over the other eye for a period each day. Recommendations vary regarding the daily and total durations for which the patch should be worn. Additional treatment options include wearing opaque contact lenses, placement of cloth occluders over glasses, and adjustment of prescription glasses to blur vision in the good eye.
Another alternative is penalization therapy using atropine (Atropisol; one drop of 0.5 to 1% solution two to seven days per week) to dilate the pupil of the good eye.17 This paralyzes accommodation and blurs near vision, encouraging use of the amblyopic eye. Atropine may be especially useful in children who cannot comply with occlusive therapy.
Multiple studies have shown that both patching and atropine are effective therapies.17–22 Atropine is well tolerated and costeffective.20 Local skin irritation is the most common adverse reaction with patching.20 Atropine use is associated with a greater incidence of light sensitivity, eye irritation, flushing of the skin, and headache, although these side effects rarely necessitate discontinuation of therapy.20
While using a patch or atropine, the child should engage in active therapy such as writing or drawing. Such activities require the child to concentrate on fine visual detail using the amblyopic eye. Surgery for strabismus is usually reserved for correction of misalignments to achieve good binocular vision.
For children with significant refractive errors, appropriate corrective lenses should be prescribed to maximize visual acuity. Children with correctable lesions such as cataracts or ptosis should be referred for early surgical intervention.
The success of amblyopia therapy is highly dependent on compliance with appropriate treatment. Educating parents about the consequences of amblyopia is paramount. Written instructions reinforce the importance of therapy and have been shown to improve outcomes.23 Vision can be improved, often dramatically, in most patients. However, amblyopia may recur months or years after successful therapy. The risk of recurrence is 24 percent after one year.24 If amblyopia recurs, patching or penalization may be resumed until the amblyopic eye has a chance to regain its full visual capacity.
If vision cannot be improved, the patient's quality of life may be adversely affected because the loss of stereoscopic vision (which allows for depth perception) can put patients at risk for life-threatening injuries. Another risk associated with untreated amblyopia is that damage to the healthy eye may lead to bilateral vision loss.25
Ongoing surveillance for amblyopia should remain an integral part of well-child care. Patients and their parents should be educated about the need for continued follow-up, the possibility of recurrence, the risk of permanent vision loss, and the possibility of developing occlusion-related amblyopia in the good eye from excessive therapeutic patching.