
Am Fam Physician. 2019;100(3):158-164
Patient information: See related handout on ingrown toenail management, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Ingrown toenails account for approximately 20% of foot problems in primary care. The great toe is most often affected. Ingrown toenails occur most commonly in young men, and nail care habits and footwear are most often contributory factors. No consensus has been reached for the best treatment approach, but ingrown nails may be nonsurgically or surgically treated. Nonsurgical treatments are typically used for mild to moderate ingrown nails, whereas surgical approaches are used in moderate and severe cases. Simple nonsurgical palliative measures include correcting inappropriate footwear, managing hyperhidrosis and onychomycosis, soaking the affected toe followed by applying a mid- to high-potency topical steroid, and placing wisps of cotton or dental floss under the ingrown lateral nail edge. Application of a gutter splint to the ingrown nail edge to separate it from the lateral fold provides immediate pain relief. A cotton nail cast made from cotton and cyanoacrylate adhesive, taping the lateral nail fold, or orthonyxia may also alleviate mild to moderate ingrown toenail. Surgical approaches seek to remove the interaction between the nail plate and the nail fold to eliminate local trauma and inflammatory reaction. These approaches are superior to nonsurgical ones for preventing recurrence. The most common surgical approach is partial avulsion of the lateral edge of the nail plate. Matrixectomy further prevents recurrence and can be performed through surgical, chemical, or electrosurgical means.
Ingrown nail, also known as onychocryptosis or unguis incarnatus, represents approximately 20% of foot problems presenting to family physicians.1 It occurs when the periungual skin of the lateral nail fold is traumatized by its adjacent nail plate, resulting in an inflammatory foreign body reaction.2,3 This often results in a painful, draining, foul-smelling lesion and hypertrophy of the involved nail fold.4,5
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Surgical approaches are recommended for moderate to severe ingrown toenails to prevent recurrence.2 | B | Cochrane review of 24 studies of varying methodologic quality |
| Equally effective treatments for ingrown toenails are partial nail avulsion followed by phenolization or direct surgical excision of the nail matrix.5 | B | Single-center randomized controlled trial with 58 participants |
| Oral antibiotics are not recommended for ingrown toenail unless there is cellulitis.1 | B | Single-center randomized controlled trial with 54 participants |
| Partial nail avulsion with phenolization is more effective at preventing symptomatic recurrence than surgical excision without phenolization.2 | B | Cochrane review |
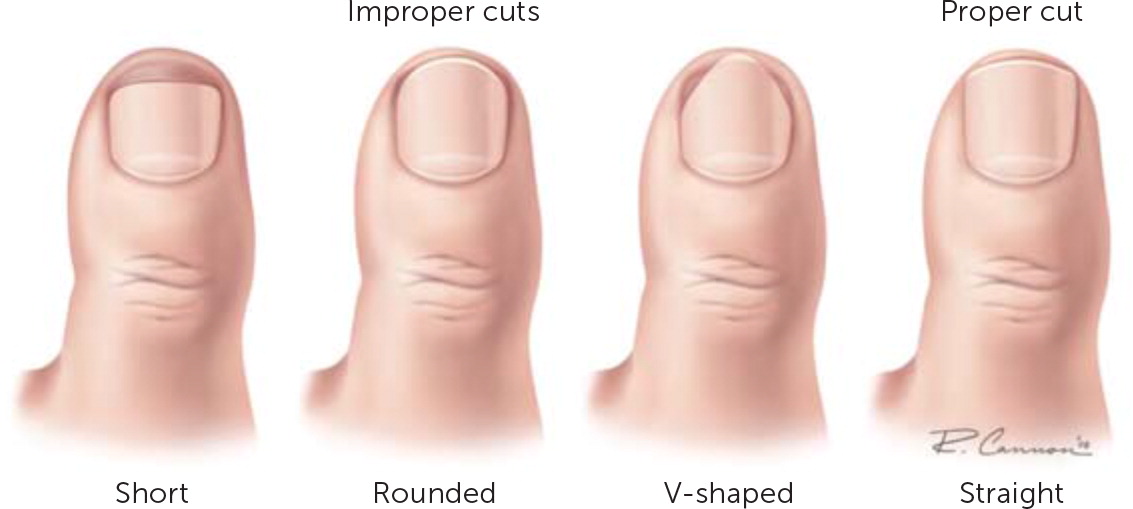
Ingrown toenail most commonly affects the great toe and is more common in young men.2,6,7 Risk factors include anatomic and physiologic mechanisms and grooming techniques, including excessive or improper trimming of the lateral nail plate. Repetitive toe trauma (e.g., running, kicking), inadvertent nail injury, wearing constricting footwear, and the reduced ability to care for one's nails are also risk factors3,4 (Figure 18).
Treatment
The natural history of untreated ingrown toenails is supported by few data, and no consensus on the best treatment technique is available.2 However, ingrown toenails are usually treated because they typically persist or progress if not properly addressed, which results in a progressively more painful digit that affects a person's functional ability. Clinical classification based on severity may help guide therapy. Most severe cases of ingrown toenail exhibit chronic granulation formation and nail-fold hypertrophy.9
Treatment indications include pain, secondary infection, onychogryphosis, and chronic or recurrent paronychia. Potential contraindications to surgical treatment include an allergy to local anesthetics or another chemical used in the procedure, peripheral vascular disease, uncooperative patient, or a known bleeding diathesis. Relative contraindications to chemical matrixectomy include uncontrolled diabetes mellitus and peripheral vascular disease.10 Phenol exposure is contraindicated in pregnancy.
Nonsurgical treatments are typically used when the ingrown nail is at a mild or moderate stage (grades I or II, respectively); surgical treatments are preferred in moderate or severe cases (grades II or III, respectively).2,7 Neither oral nor topical antibiotics before or after treatment improve outcomes.1,2 Postoperative use of antibiotics, manuka honey, povidone-iodine with paraffin, hydrogel with paraffin, or paraffin gauze does not improve infection rates, pain, or healing time.2
A 2012 Cochrane review found that surgical interventions are better than nonsurgical interventions at preventing recurrence.2 In the review, four of the 12 studies demonstrated that the addition of chemical nail matrix ablation to surgical intervention resulted in a significant reduction in recurrence.2 One study compared partial nail avulsion with matrix excision to the same intervention with phenol ablation in 117 participants and found that the use of phenol was significantly more effective in preventing recurrence.2 With the lack of availability of direct comparative evidence, the choice of intervention is influenced by patient preference, supply availability, and physician expertise.
NONSURGICAL THERAPY
Nonsurgical interventions are appropriate in patients with mild to moderate ingrown toenail (grade I or II) who do not have significant pain, substantial erythema, or purulent discharge. The goal of nonsurgical therapy is to relieve symptoms, prevent progression, promote resolution, and prevent recurrence. Conservative therapy provides a cost-effective, often patient-applied approach that may obviate the need for a minor surgical procedure. Treatment is continued until the normal nail grows past the edge of the lateral fold, which typically occurs in two to 12 weeks.
Simple measures include wearing appropriate footwear with an open toe or wide toe box and managing underlying factors such as hyperhidrosis and onychomycosis. Patients may soak the affected toe and foot for 10 to 20 minutes in warm, soapy water followed by application of a mid- to high-potency steroid cream or ointment to the affected area several times daily for two to 14 days.11 Another option is placing wisps of cotton or dental floss under the ingrown lateral nail edge.11 Both methods are effective for mild to moderate cases.12 A newer treatment approach involves using tape to pull the nail fold away from the nail plate. Tape is placed along the top of the affected lateral nail fold, wrapped around the underside, and then across the toe proximal to the fold.13
Physicians may apply a gutter splint to the ingrown nail edge by slitting vinyl intravenous tubing and cutting it to fit with one end cut diagonally for smooth insertion14 (Figure 28). After a digital block or local anesthesia infiltration, the splint is placed over the side of the ingrowing plate and affixed with tape, cyanoacrylate adhesive, suture, or wound closure strips.15 Patients frequently get pain relief after application of a gutter splint.

Another nonsurgical, physician-applied method involves creating a cotton nail cast using forceps to introduce a small piece of cotton in a U shape between the nail plate and the affected nail fold. The cast is secured and hardened with cyanoacrylate adhesive. Anesthesia is not necessary. A trial of this approach showed pain resolution in less than 24 hours in 50% of the patients and before 72 hours in 100% of the patients without other treatments.16 The cotton cast may be removed after two months, at resolution, or may be allowed to fall out spontaneously.
Orthonyxia involves placing a small metal brace on the nail after the involved part of the nail is excised. The metal brace has an omega shape in the center and U-shaped hooks on both sides. After the hooks are placed around both edges of the nail, tension is applied to the brace, and then it is attached to the nail plate with an adhesive.2
SURGICAL THERAPY
The goal of surgical intervention is to remove the interaction between the nail plate and the nail fold to eliminate local trauma and foreign body reaction2 (Figure 317). Surgical techniques involve removing the pressure of the nail plate on the nail fold by excising all or part of the nail plate or by excising all or part of the nail fold.2

Surgical procedures for ingrown nails include the following: partial nail avulsion (Ross procedure) with or without partial matrixectomy; wedge excision, wedge segmental excision, or wedge resection with nail matrix destruction (Winograd procedure); total nail avulsion with or without excision of any granuloma with or without total (chemical or surgical) excision of the matrix (Zadik procedure); rotational flap technique of the nail fold; or radical nail-fold excision (Vandenbos procedure). Surgical procedures are supported by minimal comparative data. In the Cochrane review, one study showed no significant difference in recurrence with nail-edge excision and total avulsion of the nail.2 Less recurrence after 12 months with wedge resection (risk ratio = 0.19; 95% CI, 0.05 to 0.80) and radical excision of the nail fold (risk ratio = 0.17; 95% CI, 0.04 to 0.72) than with the rotational flap technique was also noted.2 Prevention of recurrence between wedge resection and radical excision of the nail fold showed no significant difference after 12 months.2
The most common procedure for treating locally ingrown toenails is partial avulsion of the lateral edge of the nail plate sometimes followed by lateral horn matrixectomy by phenolization or surgical excision of the lateral horn of the nail matrix, both of which are equally effective5 (Table 118–23 and Figure 423). When possible, partial nail-plate avulsion is preferred to complete avulsion because it minimizes trauma to the adjacent tissues.24,25

|

Most of the lateral fold redness associated with onychocryptosis results from the foreign body reaction. After the ingrown portion of the nail is removed and matrixectomy is performed, any localized inflammation and/or infection should resolve without the need for antibiotic therapy with similar healing times.1,26,27 Thus, oral or topical antibiotic treatment is not recommended unless clear, widespread cellulitis is present.1,2
NAIL MATRIXECTOMY
Matrixectomy can be performed surgically, chemically, electrosurgically, or with radiofrequency ablation; all are effective options when treating ingrown toenails (Table 22,23,28–30). Unilateral matrixectomy is effective and appropriate in most cases, but contralateral ingrown toenail may develop over time.31 Bilateral partial matrixectomy maintains the functional and cosmetic role of the nail plate (although narrowing it) and may be considered in patients with severe ingrown nail or recurrences.32

Electrosurgical
|
Phenol
|
Sodium hydroxide
|
Lateral nail matrixectomy is required to permanently eliminate the lateral nail-forming tissue and to narrow the width of the nail plate to better fit the lateral nail fold. The agents used for chemical cauterization of the lateral horns of the nail matrix are phenol and sodium hydroxide, which produce success rates of more than 95%.33,34 Phenol chemical ablation is relatively easy to perform, causes minimal bleeding, allows the patient to return to normal activities after a few days, is not significantly disfiguring, and has less than 5% recurrence rate35,36 (Figure 4D23). Because of phenol's antiseptic and hemostatic effects, it is particularly useful in patients with diabetes and those using anticoagulants.28 Segmental phenolization may produce less postprocedure pain and has better postoperative outcomes than sharp excision.37,38 Studies of phenol matrixectomy show recurrence rates of 1.1% to 4.3% over six to 33 months of follow-up.28
A Cochrane systematic review found that partial nail avulsion combined with phenolization is more effective at preventing symptomatic recurrence than surgical excision without phenolization (one in 25 patients with recurrence vs. eight in 21 without phenol).2 Trials evaluating different treatment methodologies have not adequately assessed patient satisfaction because most follow-up times occurred in less than six months.
Phenolization does not increase the risk of infection more than matrix excision.39 Excessive phenolization affecting adjacent tissues may cause serous oozing for up to five to six weeks after the procedure. The use of 20% ferric chloride–soaked sterile cotton application for 20 to 30 seconds to the exposed nail bed has been found to reduce nail-bed oozing, but it carries a small risk of inducing local thrombosis.9
A prospective study of partial nail avulsion and chemical matrixectomy using 80% trichloroacetic acid involving 197 ingrown toenails demonstrated a 94% success rate with 4% non-ingrown spicule reformation and 2% recurrence rate.7 This agent caused less reported pain in one study than has been reported with phenol or sodium hydroxide, but direct comparison studies are lacking.7 Additional evidence of safety and relative effectiveness are still needed.
Electrosurgical ablation of the nail bed is a highly successful alternative that produces less discharge (Figure 523). Special high-frequency unit matrixectomy electrodes coated with a nonconductive coating on one side can be used to avoid injury to the overlying normal tissue of the proximal nail fold (i.e., cuticle) while ablating the nail bed.8 Laser matrixectomy is another option, but it has high equipment and upkeep costs.8

The granulation tissue produced by the foreign-body reaction can produce lateral wall hypertrophy. Because this tissue is abnormal, some physicians advocate removal at the time of nail surgery. Removal can be accomplished with scalpel excision or with electrosurgical excision or ablation. Tissue removal can produce a scooped-out defect in the lateral tissue at the time of the procedure. This defect fills in over several weeks as the remaining normal lateral tissue grows to the newly formed lateral nail edge.
POSTPROCEDURE INSTRUCTIONS
The toe should be rested and preferably elevated during the first 12 to 24 hours. Pain should be minor when matrixectomy is performed because it ablates the nail-bed nerve endings. Nonsteroidal anti-inflammatory drugs or acetaminophen may be used for discomfort. The dressing should be changed in 24 to 48 hours, and normal ambulation may be fully resumed.24 A sterile exudate from the nail bed should be expected for two to three weeks.29
An incomplete matrixectomy can result in a recurrence. If infection of the lateral nail fold is suspected, an oral antibiotic that treats common skin flora (e.g., cephalexin [Keflex], 500 mg orally four times daily for five to seven days) should be prescribed.10 Overaggressive electrocautery or radiofrequency ablation to the nail matrix may damage the adjacent and underlying fascia or periosteum. If the toe is healing poorly several weeks after the procedure, debridement, oral antibiotics, and radiographic evaluation may be warranted.11 Granulation tissue and the recess sometimes created by the removal of the nail will gradually resolve to a more normal appearance. Rarely, permanent loss of nail plate, nail-plate dystrophy, or pyogenic granuloma may occur.
This article updates previous articles on this topic by Heidelbaugh and Lee,8 and Zuber.40
Data Sources: A PubMed search was completed in Clinical Queries using the key terms ingrown nail, onychocryptosis, and unguis incarnatus. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. We also searched the Agency for Healthcare Research and Quality evidence reports, Clinical Evidence, the Cochrane database, Essential Evidence Plus, and the National Guideline Clearinghouse database. Search date: March 25, 2019. Secondary searches were done for matrixectomy and digital blocks on March 25, 2019.
