Food Intolerance vs Food Allergy: US Burden and Role of IgE
Food allergies can cause severe immune reactions, including anaphylaxis. Each year, it is estimated that food allergy reactions result in 30,000 emergency room visits, 2,000 hospitalizations, and 150 deaths in the US.1
Adverse reactions to food can be broken down into two distinct categories: food allergies and food intolerances.2 The majority of food reactions come from food intolerances, such as lactose intolerance, gluten intolerance, and sensitivity to some pharmacological substances like caffeine. These reactions can manifest as a GI problem like abdominal pain or diarrhea.2,3
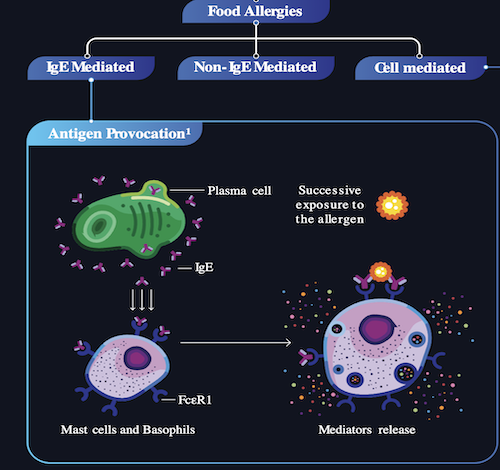
Food allergies, however, are distinct from food intolerances. Unlike food intolerances, IgE-mediated food allergies can be life-threatening.3 Food allergy is a pathological reaction of the immune system that can be mediated by IgE, non-IgE, or mixed immune reactions.
IgE-mediated food allergy is predominant.2,4 It occurs when the body develops antibodies to a food, which then triggers the release of histamine and other proinflammatory mediators from mast cells. Reactions are typically rapid, occurring within minutes or hours, and symptoms may include itching, swelling, hives, trouble breathing, and anaphylaxis.3
Food Allergy Burden Is Often Exacerbated by Social Determinants of Health
Persons of non-Hispanic Black descent are more likely to be diagnosed with a food allergy than are non-Hispanic Whites and Asians. In addition, data suggest that patients of lower socioeconomic status tend to experience suboptimal treatment.4 Patients from lower-income families spend 2.5 times more on emergency department visits and hospitalizations, and 21% of these families are food insecure.5
Download IgE Mediated Food Allergy Infographic to learn more.
All information shared by Genentech Medical is intended to foster scientific exchange with US healthcare professionals and should not be interpreted as a recommendation for use.
REFERENCES
- Food Allergy and Anaphylaxis Connection Team. https://www.foodallergyawareness.org/food-allergy-and-anaphylaxis/anaphylaxis/anaphylaxis/ Accessed July 15, 2024.
- Boyce JA et al. J Allergy Clin Immunol. 2010;126(6 suppl):S1-S58.
- American Academy of Allergy, Asthma & Immunology. https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/food-intolerance. Accessed July 15, 2024.
- Warren C et al. Ann Allergy Asthma Immunol. 2022:129(4):407-416. https://pubmed.ncbi.nlm.nih.gov/35914663/ Accessed July 15, 2024.
- Tepler E et al. Ann Allergy Asthma Immunol. 2022;129(4):417-423. https://pubmed.ncbi.nlm.nih.gov/35476967/ Accessed July 15, 2024.
Disclaimer:
The posting of information and content on this page should not be considered an AAFP endorsement or recommendation of the partner or sponsor organization’s products, services, policies or procedures. The information and opinions expressed are those of partners and paid sponsors and do not necessarily reflect the views of the AAFP. The AAFP is not responsible for the content of third-party websites linked from this page. Any links on this page to third-party websites where goods and services are advertised are not endorsements or recommendations by the AAFP of the third-party sites, goods or services.