
Am Fam Physician. 2003;68(11):2167-2176
A more recent article on acute hand infections is available.
Hand infections can result in significant morbidity if not appropriately diagnosed and treated. Host factors, location, and circumstances of the infection are important guides to initial treatment strategies. Many hand infections improve with early splinting, elevation, appropriate antibiotics and, if an abscess is present, incision and drainage. Tetanus prophylaxis is indicated in patients who have at-risk infections. Paronychia, an infection of the epidermis bordering the nail, commonly is precipitated by localized trauma. Treatment consists of incision and drainage, warm-water soaks and, sometimes, oral antibiotics. Afelon is an abscess of the distal pulp of the fingertip. An early felon may be amenable to elevation, oral antibiotics, and warm water or saline soaks. Amore advanced felon requires incision and drainage. Herpetic whitlow is a painful infection caused by the herpes simplex virus. Early treatment with oral antiviral agents may hasten healing. Pyogenic flexor tenosynovitis and clenched-fist injuries are more serious infections that often require surgical intervention. Pyogenic flexor tenosynovitis is an acute synovial space infection involving a flexor tendon sheath. Treatment consists of parenteral antibiotics and sheath irrigation. A clenched-fist injury usually is the result of an altercation and often involves injury to the extensor tendon, joint capsule, and bone. Wound exploration, copious irrigation, and appropriate antibiotics can prevent undesired outcomes.
The hand can easily be injured during everyday activities. Any trauma to the hand, particularly a penetrating trauma, may introduce damaging pathogens. The hand's compartmentalized anatomy may contribute to the development of an infection. If an infection is not appropriately diagnosed and treated, significant morbidity can result.
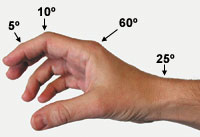
Some general wound-care principles apply to all hand infections.1,2 Most hand infections can be treated with an initial period of rest, immobilization, and elevation. Splint immobilization and elevation can protect the affected area, minimize edema, and decrease pain. If a single digit is infected, a finger splint supporting the interphalangeal joints in extension is usually adequate. If the palm, the metacarpophalangeal (MCP) joint, or larger portions of the hand are infected, splinting in a position of function (Figure 1) can help protect against flexion contractures and hasten rehabilitation.
Open wounds should be gently, but copiously, irrigated to remove debris and purulent material. When an abscess has formed or pus is present, incision and drainage are necessary. Devitalized and contaminated tissue serves as a potent culture medium and should be promptly debrided. Minor infections may resolve with these measures alone.
More severe infections require oral or parenteral antibiotics and, possibly, surgical intervention. Moist heat may be used to increase local circulation and may enhance antibiotic delivery to the tissue. Photographs and diagrams of the hand may be helpful in assessing the success of therapy. All tetanus-prone wounds (e.g., soil, animal, oral, fecal exposure) require tetanus prophylaxis.
| Host factor | Considerations |
|---|---|
| Diabetes mellitus | Higher incidence of mixed and pure gram-negative organisms (approaching 30 to 40 percent) requiring use of broader spectrum antibiotics. Susceptible to more severe infections and more likely to require surgical intervention. Patients on renal dialysis pose the highest risk.8 |
| Immunocompromised state (patients on immunosuppressive therapy and patients with HIV infection or AIDS) | More susceptible to opportunistic infections. |
| Pyogenic flexor tenosynovitis as well as cutaneous abscesses are known potential sequelae of disseminated Neisseria gonorrhoeae and are more common in patients who are immunocompromised.1,3,5 | |
| Candidal flexor tenosynovitis infection has been reported in patients who are immunocompromised.7 | |
| Intravenous drug use | Mixed aerobic and anaerobic hand infections are common and usually caused by oral pathogens. Patients commonly present with subcutaneous abscesses and tendon sheath infections. They require the use of broader spectrum antibiotics.1–4 |
| Tropical fish aquarium exposure | The culprit organism is more likely to be Mycobacterium marinum. This organism is quite fastidious and often responsible for chronic, indolent hand infections.9 |
| Possible sexually transmitted disease exposure | Flexor tenosynovitis as well as cutaneous abscesses are known potential sequelae of disseminated N. gonorrhoeae infection.1,3,5,6,10 |
| Condition | Most common offending organisms | Recommended antimicrobial agents | Comments | |
|---|---|---|---|---|
| Paronychia | Usually Staphylococcus aureus or streptococci; pseudomonas, gram-negative bacilli, and anaerobes may be present, especially in patients with exposure to oral flora | First-generation cephalosporin or anti-staphylococcal penicillin; if anaerobes or Escherichia coli are suspected, oral clindamycin (Cleocin) or a beta-lactamase inhibitor such as amoxicillin-clavulanate potassium (Augmentin) | Incision and drainage should be performed if infection is well established. | |
| If infection is chronic, suspect Candida albicans. | ||||
| Early infections without cellulites may respond to conservative therapy. | ||||
| Felon | S. aureus, streptococci | First-generation cephalosporin or anti-staphylococcal penicillin | Incision and drainage should be performed if infection is well established. | |
| Oral antibiotic therapy usually is adequate. | ||||
| Herpetic whitlow | Herpes simplex virus types 1 and 2 | Supportive therapy | Antivirals may be prescribed if infection has been present for less than 48 hours. | |
| For recurrent herpetic whitlow, suppressive therapy with an antiviral agent may be helpful. | ||||
| Consider antibiotics if secondarily infected. | ||||
| Incision and drainage are contraindicated. | ||||
| Pyogenic flexor tenosynovitis | S. aureus, streptococci, anaerobes | Parenteral first-generation cephalosporin or antistaphylococcal penicillin and penicillin G or Parenteral beta-lactamase inhibitor such as ampicillin-sulbactam (Unasyn) Use ceftriaxone (Rocephin) or a fluoroquinolone if Neisseria gonorrhoeae is suspected. | Early surgical assessment is suggested. | |
| N. gonorrhoeae or C. albicans should be suspected in sexually active or immunocompromised patients. | ||||
| Incision and drainage with catheter irrigation of the sheath should be performed if no improvement within the first 12 to 24 hours of conservative therapy. | ||||
| Human bite, clenched-fist injury | S. aureus, streptococci, Eikenella corrodens, gram-negative bacilli, anaerobes | Parenteral first-generation cephalosporin or antistaphylococcal penicillin and penicillin G or Beta-lactamase inhibitor such as ampicillin-sulbactam or amoxicillin-clavulanate potassium or Second-generation cephalosporin such as cefoxitin (Mefoxin) | Prophylactic oral antibiotics should be used if outpatient therapy is chosen. | |
| Wounds should be explored, copiously irrigated, and surgically debrided. | ||||
| Hospitalization and parenteral antibiotics often are indicated. | ||||
Paronychia
Paronychia is an infection of the perionychium (also called eponychium), which is the epidermis bordering the nail. Paronychia results in swelling, erythema, and pain at the base of the fingernail (Figure 2). A review of acute and chronic paronychia was recently published in this journal.11 Acute paronychia is usually the result of localized trauma to the skin surrounding the nail plate. This infection is usually the result of dishwashing, a manicure, an ingrown nail, or a hangnail, and usually becomes evident two to five days posttrauma.12,13 Paronychia in children is usually the result of thumb sucking.

The responsible organisms in acute paronychia are usually Staphylococcus aureus and Streptococcus pyogenes; pseudomonas organisms are rarely responsible.3,4,11,12,14 Warm water soaks alone may be effective if an abscess has not formed. If spontaneous drainage does not occur or if an abscess is well established, incision and drainage are warranted. Surgical treatment techniques are well described in the medical literature.3,4,11,12 Direct damage and incision to the cuticle are not recommended. For severe infections, an antistaphylococcal penicillin or a first-generation cephalosporin should be given.3,12,14 Clindamycin (Cleocin) or amoxicillin-clavulanate potassium (Augmentin) may be considered if anaerobes and Escherichia coli are suspected organisms.4,11 A tetanus booster should be administered when appropriate. Chronic paronychia often is caused by a candidal infection that may respond to treatment with a topical antifungal/steroid agent.11,12
Felon
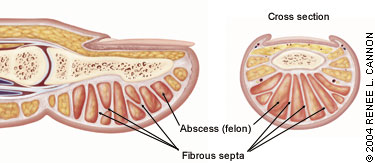
A felon is an abscess of the distal pulp or phalanx pad of the fingertip.1,2,12,14,15 The pulp of the fingertip is divided into small compartments by 15 to 20 fibrous septa that run from the periosteum to the skin (Figure 3). Abscess formation in these relatively noncompliant compartments causes significant pain, and the resultant swelling can lead to tissue necrosis. Because the septa attach to the periosteum of the distal phalanx, spread of infection to the underlying bone can result in osteomyelitis.16
A felon usually is caused by inoculation of bacteria into the fingertip through a penetrating trauma. The most commonly affected digits are the thumb and index finger.15 Common predisposing causes include splinters, bits of glass, abrasions, and minor puncture wounds. A felon also may arise when an untreated paronychia spreads into the pad of the fingertip. Felons have been reported following multiple finger-stick blood tests.12
Patients present with rapid onset of severe, throbbing pain, with associated redness and swelling of the fingertip (Figure 4). The pain caused by a felon is usually more intense than that caused by paronychia. The swelling will not extend proximal to the distal interphalangeal joint. Occasionally, the high pressure in the fingertip pad will cause a felon to spontaneously drain, resulting in a visible sinus.

If diagnosed in the early stages of cellulitis, a felon may be amenable to treatment with elevation, oral antibiotics, and warm water or saline soaks.4,12,15 Bone and soft tissue radiographs should be obtained to evaluate for osteomyelitis or a foreign body. Tetanus prophylaxis should be administered when necessary.
If fluctuance is present, incision and drainage are appropriate. The preferred techniques3,4,12,14,15 are a single volar longitudinal incision or a high lateral incision (Figure 5). Potential complications of a felon and felon drainage include an anesthetic fingertip, a neuroma, and an unstable finger pad. The family physician's comfort level and the availability of a surgeon may determine whether this procedure is performed in the family physician's office, or the patient is referred.
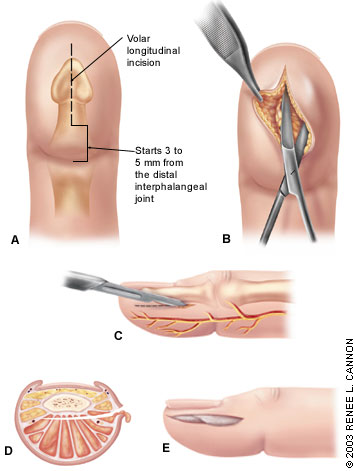
Postoperative care includes loose packing, splinting, and elevation of the hand for approximately 24 hours. Dry dressing changes with twice-daily saline soaks, range-of-motion activities and, eventually, scar massage may accelerate return to normal activity.12
Gram stain should guide initial antibiotic therapy. As with paronychia, the most common isolated organism is S. aureus. Empiric antibiotic coverage with a first-generation cephalosporin or antistaphylococcal penicillin usually is adequate treatment for an uncomplicated felon. The recommended length of treatment varies from five to 14 days and depends on the clinical response and severity of infection.3,12 Methicillin-resistant S. aureus has been reported in felons and other hand infections; clinical response, as well as bacterial cultures, should be followed closely.17,18
Herpetic Whitlow
Viral infections of the hand are rare, with the exception of the clinical entity known as herpetic whitlow. Herpetic whitlow results from autoinoculation of type 1 or type 2 herpes simplex virus into broken skin. The infection may occur as a complication of primary oral or genital herpes lesions. Health care workers exposed to oral secretions (e.g., dental hygienists, respiratory therapists) can be affected if they are not using universal precautions.
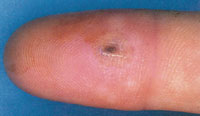
Signs and symptoms of herpetic whitlow include the abrupt onset of edema, erythema, and significant localized tenderness of the infected finger. Often, the pain is out of proportion to the physical findings. Fever, lymphadenitis, and epitrochlear and axillary lymphadenopathy may be present. Small, clear vesicles initially are present. These may eventually coalesce and, as the fluid becomes cloudier, mimic a pyogenic bacterial infection. If in a distal location, herpetic whitlow may mimic paronychia or felon (Figure 6). A history of localized trauma to the nail cuticle may be helpful in distinguishing herpetic whitlow from paronychia. A diagnosis of herpes simplex virus infection may be confirmed with a Tzanck test, viral culture, or DNA amplification technique.
Herpetic whitlow usually is self-limited and resolves in two to three weeks. Treatment within the first 48 hours of symptom onset with acyclovir (Zovirax), famciclovir (Famvir), or valacyclovir (Valtrex) may lessen the severity of infection, but randomized controlled trials have not been performed.19–21 Because viral shedding continues until the epidermal lesion is healed, contact with the lesion should be avoided by keeping the affected digit covered with a dry dressing. Incision and drainage of the lesion may cause viremia or bacterial infection.2–4 Patients should be advised that the infection recurs in 30 to 50 percent of cases, but the initial infection is typically the most severe. Treatment with antivirals may be beneficial for recurrent herpetic whitlow if initiated during the prodromal stage.19–23
Pyogenic Flexor Tenosynovitis
The flexor tendons of the hand are enclosed in distinct synovial sheaths. The flexor tendon sheaths of the index, middle, and ring fingers extend from the distal phalanges to the distal palmar crease, and generally do not communicate. The sheath encompassing the fifth finger extends from its distal phalanx to the mid-palm, where it expands across the palm to form the ulnar bursa. The thumb flexor sheath begins at the terminal phalanx and extends to the volar wrist crease, where it communicates with the radial bursa. Anatomic variations are frequent. For example, the radial bursa can communicate with the ulnar bursa at the wrist (an infection of this area is called a “horseshoe abscess”). The synovial sheaths, poorly vascularized and rich in synovial fluid, provide an optimal environment for bacterial growth. Once inoculated, infection can spread rapidly within the confines of the sheath.2 Infection of the flexor tendon sheath, known as pyogenic flexor tenosynovitis (Figures 7 and 8), warrants early surgical evaluation.2–4,14,24
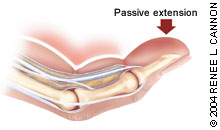

Patients with pyogenic flexor tenosynovitis present with the four cardinal signs as described by Kanavel: (1) uniform, symmetric digit swelling; (2) at rest, digit is held in partial flexion; (3) excessive tenderness along the entire course of the flexor tendon sheath; and (4) pain along the tendon sheath with passive digit extension.25 Pain with passive extension has been reported as the most clinically reproducible of these four signs.24,26
Patients typically recall some antecedent trauma or puncture wound. The trauma often is at a flexor crease; this is where the tendon sheath is most superficial. Hematogenous spread to the sheath (i.e., Neisseria gonorrhoeae) occurs rarely but should be suspected if there is no puncture wound or history of trauma.5,6
Early diagnosis and treatment of pyogenic flexor tenosynovitis is necessary to prevent tendon necrosis, adhesion formation, and spread of infection to the deep fascial spaces. Distinguishing a subcutaneous abscess from a tendon sheath infection can be challenging. A subcutaneous abscess should not have tenderness over the entire sheath, and passive mobility of the uninvolved segments should be painless.15 Elevated sheath pressures consistent with compartment syndrome pressures (i.e., higher than 30 mm Hg) have been documented in flexor tenosynovitis.27 Ultrasound examination may show an abnormal effusion or abscess in the tendon sheath.28
Infections in the early stage may respond to nonoperative treatment that includes splinting, elevation, and intravenous antibiotics. Rings should be removed from the affected finger and other fingers of the hand as soon as possible.
Causative agents for flexor tenosynovitis typically include Staphylococcus and Streptococcus species.1,2,24 Mixed infections should be suspected in patients who have diabetes or are immunocompromised.8,24 Disseminated gonorrhea5 and Candida albicans7 infection have been reported as causes of flexor tenosynovitis in immunocompromised patients.
Gram stain and wound culture growth should guide antibiotic therapy. Empiric therapy should include parenteral penicillin plus either an antistaphylococcal penicillin or a first-generation cephalosporin.1,3,4,24 Alternatively, a parenteral beta-lactamase inhibitor may be used as monotherapy. Tetanus prophylaxis should be administered if necessary.
If there is no improvement within 12 to 24 hours, surgical intervention is warranted. Early surgical treatment should be considered if the patient is immunocompromised or has diabetes.24 Surgical treatment involves proximal and distal tendon exposure, and careful insertion of a catheter or feeding tube into the tendon sheath with copious intraoperative irrigation.1,4,15,24,25 Postoperatively, the catheter may be left in place for 24 hours to allow for further low-flow irrigation. One retrospective study29 questioned the utility of postoperative irrigation and found no difference in outcome whether the catheter was left in or taken out. Parenteral antibiotic therapy should be continued for at least 48 hours. Comparable oral antibiotic therapy should then be instituted and continued for an additional five to 14 days on an outpatient basis. Physical and occupational therapy should be initiated to reduce long-term disability from scarring and contractures.
Human Bite and Clenched-Fist Injuries
Human bite injuries to the hand usually result from a direct bite or a “fight bite” (also known as a “clenched-fist” injury).30–32 Direct human bite injuries are often visually evident. A clenched-fist injury typically is characterized by a 3- to 5-mm laceration on the dorsum of the hand or overlying an MCP joint (Figure 9). Because of the innocent appearance of this injury, patients may not seek medical attention and commonly present with advanced infection.

A clenched-fist wound is the result of a fist striking an object, such as another person's face, with considerable force. A tooth may penetrate an extensor tendon and MCP joint capsule, sometimes fracturing a metacarpal or phalangeal bone. Because the injury occurs with the MCP joint in flexion, injuries to the extensor tendon and joint capsule can be overlooked easily during examination of the MCP joint in extension. In a study of 191 patients with clenched-fist injuries, 75 percent had an injury to tendon, bone, joint, or cartilage.33
Recognition of the potential severity of the injury is important in the management of a clenched-fist injury. Radiographs should be obtained to assess for fracture, foreign body, gas, or osteomyelitis. A thorough neurovascular and musculoskeletal examination should be performed. Extensor tendon function should be documented.
Puncture wounds should be extended proximally and distally while the physician is looking for extensor tendon disruption or injury. The wound should be explored, copiously irrigated, and surgically debrided. Material for Gram stain and aerobic/anaerobic cultures should be obtained from deep within all suppurative wounds before therapy is instituted. Gram stain results should guide initial antibiotic therapy. The wound should not be sutured but allowed to heal by secondary intention. The hand should be splinted in a position of function and elevated. Occupational rehabilitation can be considered once the infection has cleared.
Human bite infections are often more virulent than animal bite injuries and are polymicrobial in nature.30,31,34 Cultures grow an average of five different organisms, three of which are usually anaerobes.30 Isolated anaerobes are commonly beta-lactamase producers. S. aureus and streptococci also are commonly isolated. Eikenella corrodens, an anaerobic gram-negative rod, has been found in 10 to 29 percent of infections.30
Patients who present early with uncomplicated wounds (i.e., no joint capsule penetration or tendon injury, and the injury happened less than 24 hours earlier) should be given prophylactic antimicrobial therapy.
The use of early prophylactic antibiotics in uncomplicated wounds is supported by one small, randomized prospective clinical trial.35 [Evidence level B, lower quality randomized controlled trial] This trial compared mechanical wound care alone (N = 15) with wound care plus prophylactic oral cefaclor (Ceclor), N = 16, or intravenous cefazolin (Kefzol) plus penicillin G (N = 17). Patients with joint capsule penetration, tendon injury, and bites older than 24 hours were excluded from the study. All patients were hospitalized. The trial was terminated early because the infection rate in the group that received mechanical wound care alone was extraordinarily high (47 percent).
None of the patients treated with antibiotics developed a subsequent infection. The authors conclude that, in the treatment of uncomplicated clenched-fist injuries, mechanical wound care alone is insufficient, and oral and intravenous antibiotics are equally efficacious for prophylaxis. This trial was emphasized in a recent Cochrane systematic review on antibiotic prophylaxis for mammalian bites.36
Outpatient management for uncomplicated wounds (as described above) can be considered after the wound has been adequately cleaned and explored. In outpatient therapy, one of three treatment options should be used: (1) amoxicillin-clavulanate potassium; (2) penicillin (to cover E. corrodens) plus an antistaphylococcal penicillin (such as dicloxacillin); or (3) penicillin plus a first-generation cephalosporin. First-generation cephalosporins are not effective as monotherapy because some anaerobic bacteria and E. corrodens are resistant. In patients who are allergic to penicillin, clindamycin plus either a fluoroquinolone or trimethoprim-sulfamethoxazole (Bactrim, Septra) should provide adequate coverage. A tetanus booster should be administered if necessary.
Some clinicians believe that all clenched-fist injuries warrant hospital admission and surgical consultation.34 If treated on an outpatient basis, the patient should return at 24 hours for a wound check. Hospital admission with parenteral antibiotic administration should be considered for patients with any of the following: (1) diabetes or peripheral vascular disease; (2) immunocompromised state (secondary to disease or drugs); (3) wound older than 24 hours; (4) wound that involves injury to the extensor tendon, joint capsule, or bone; (5) questionable follow-up or compliance with antibiotic therapy; (6) systemic symptoms (e.g., fever, chills); or (7) cellulitis.30 If the patient is hospitalized, a broad-spectrum parenteral antibiotic (such as ampicillin-sulbactam [Unasyn] or ticarcillin-clavulanate potassium [Timentin]), or a second-generation cephalosporin such as cefoxitin (Mefoxin) should be administered.
Differential Diagnosis
Several noninfectious conditions, some of which can be difficult to distinguish, can mimic a hand infection.37,38 Crystalline deposition disease (e.g., gout, pseudogout), pyogenic granuloma, acute calcium deposition, acute nonspecific flexor tenosynovitis, brown recluse spider bites, rheumatoid arthritis, and foreign-body reactions can mimic an acute hand infection and should be considered in the differential diagnosis.