
Am Fam Physician. 2008;77(2):199-202
Patient information: See related handout on peritonsillar abscess, written by the author of this article.
Author disclosure: Nothing to disclose.
Peritonsillar abscess remains the most common deep infection of the head and neck. The condition occurs primarily in young adults, most often during November to December and April to May, coinciding with the highest incidence of streptococcal pharyngitis and exudative tonsillitis. A peritonsillar abscess is a polymicrobial infection, but Group A streptococcus is the predominate organism. Symptoms generally include fever, malaise, sore throat, dysphagia, and otalgia. Physical findings may include trismus and a muffled voice (also called “hot potato voice”). Drainage of the abscess, antibiotics, and supportive therapy for maintaining hydration and pain control are the foundation of treatment. Antibiotics effective against Group A streptococcus and oral anaerobes should be first-line therapy. Steroids may be helpful in reducing symptoms and speeding recovery. To avoid potential serious complications, prompt recognition and initiation of therapy is important. Family physicians with appropriate training and experience can diagnose and treat most patients with peritonsillar abscess.
Peritonsillar abscess is the most common deep infection of the head and neck in young adults, despite the widespread use of antibiotics for treating tonsillitis and pharyngitis. This infection can occur in all age groups, but the highest incidence is in adults 20 to 40 years of age.1,2 Peritonsillar abscess most commonly occurs during November to December and April to May, which coincides with the highest incidence rates of streptococcal pharyngitis and exudative tonsillitis.3,4 Peritonsillar abscesses are almost always first encountered by the family physician, and those with appropriate training and experience can diagnose and treat most patients. Prompt recognition and initiation of therapy is important to avoid potential serious complications.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Treatment for peritonsillar abscess should include drainage and antibiotic therapy. | C | 1, 3, 6, 12 |
| Initial empiric antibiotic therapy for peritonsillar abscess should include antimicrobials effective against Group A streptococcus and oral anaerobes. | C | 8, 13, 14 |
| Steroids may be useful in reducing symptoms and in speeding recovery in patients with peritonsillar abscess. | B | 17 |
Anatomy
The two palatine tonsils lie on the lateral walls of the oropharynx in the depression between the anterior tonsillar pillar (palatoglossal arch) and the posterior tonsillar pillar (palatopharyngeal arch). The tonsils form during the last months of gestation and grow irregularly, reaching their largest size at approximately six or seven years of age. The tonsils begin to gradually involute at puberty, and by older age little tonsillar tissue remains.5 When healthy, the tonsils do not project beyond the tonsillar pillars medially.2 Each tonsil has a number of crypts on its surface and is surrounded by a capsule that provides a pathway for blood vessels and nerves. Peritonsillar abscesses form in the area between the palatine tonsil and its capsule.1
Etiology
Peritonsillar abscess has traditionally been regarded as the end point of a continuum that begins as acute exudative tonsillitis, progresses to cellulitis, and eventually forms an abscess. A recent review implicates Weber's glands as playing a key role in the formation of peritonsillar abscesses.6,7 This group of 20 to 25 mucous salivary glands are located in the space just superior to the tonsil in the soft palate and are connected to the surface of the tonsil by a duct.7 The glands clear the tonsillar area of debris and assist with the digestion of food particles trapped in the tonsillar crypts. If Weber's glands become inflamed, local cellulitis can develop.
As the infection progresses, the duct to the surface of the tonsil becomes progressively more obstructed from surrounding inflammation. The resulting tissue necrosis and pus formation produce the classic signs and symptoms of peritonsillar abscess.8 These abscesses generally form in the area of the soft palate, just above the superior pole of the tonsil, in the location of Weber's glands.7 The occurrence of peritonsillar abscesses in patients who have undergone tonsillectomy further supports the theory that Weber's glands have a role in the pathogenesis. Other clinical variables include significant periodontal disease and smoking.6
Clinical Manifestations
Patients with peritonsillar abscess appear ill and present with fever, malaise, sore throat, dysphagia, or otalgia. The throat pain is markedly more severe on the affected side and is often referred to the ear on the same side. Physical examination usually reveals trismus, with the patient having difficulty opening his or her mouth because of pain from inflammation and spasm of masticator muscles.9 Swallowing is also highly painful, resulting in pooling of saliva or drooling.9 Patients often speak in a muffled voice (also called “hot potato voice”). Markedly tender cervical lymphadenitis may be palpated on the affected side. Inspection of the oropharynx reveals tense swelling and erythema of the anterior tonsillar pillar and the soft palate overlying the infected tonsil. The tonsil is generally displaced inferiorly and medially with contralateral deviation of the uvula (Figure 1). The most common symptoms and physical findings are summarized in Table 1. Potential complications of peritonsillar abscess are outlined in Table 2. Death can occur from airway obstruction, aspiration, or hemorrhage from erosion or septic necrosis into the carotid sheath.

| Symptoms |
| Fever |
| Malaise |
| Severe sore throat (worse on one side) |
| Dysphagia |
| Otalgia (ipsilateral) |
| Physical findings |
| Erythematous, swollen soft palate with uvula deviation to contralateral side and enlarged tonsil |
| Trismus |
| Drooling |
| Muffled voice (“hot potato voice”) |
| Rancid or fetor breath |
| Cervical lymphadenitis |
| Airway obstruction |
| Aspiration pneumonitis or lung abscess secondary to peritonsillar abscess rupture |
| Death secondary to hemorrhage from erosion or septic necrosis into carotid sheath |
| Extension of the infection into the tissues of the deep neck or posterior mediastinum |
| Poststreptococcal sequelae (e.g., glomerulonephritis, rheumatic fever) when infection is caused by Group A streptococcus |
Diagnosis
The diagnosis of peritonsillar abscess is often made on the basis of a thorough history and physical examination. Differential diagnosis includes infectious mononucleosis, lymphoma, peritonsillar cellulitis, and retromolar or retropharyngeal abscess. Patients often present with peritonsillar cellulitis with the potential to progress to abscess formation. In peritonsillar cellulitis, the area between the tonsil and its capsule is edematous and erythematous, but pus has not yet formed.1
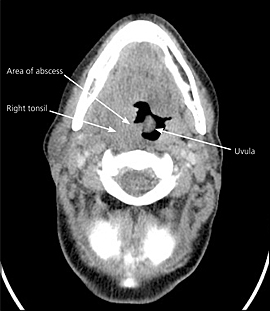
On occasions when the diagnosis of peritonsillar abscess is in question, the presence of pus on needle aspiration or radiologic testing may help confirm the diagnosis. Transcutaneous or intraoral ultrasonography also can be helpful in identifying an abscess and in distinguishing peritonsillar abscess from peritonsillar cellulitis.1,6 If spread of the infection beyond the peritonsillar space or complications involving the lateral neck space are suspected, computed tomography (CT) or magnetic resonance imaging (MRI) is indicated. CT can distinguish between peritonsillar cellulitis and peritonsillar abscess, as well as demonstrate the spread of the infection to any contiguous spaces in the deep neck region (Figure 2). MRI has the advantage of improved soft-tissue definition over CT without exposure to radiation. Additionally, MRI is superior to CT in detecting complications from deep neck infections such as internal jugular vein thrombosis or erosion of the abscess into the carotid sheath. Disadvantages of MRI include longer scanning times, higher cost, lack of availability, and the potential for claustrophobia.10
Treatment
Drainage of the abscess, antibiotics, and supportive therapy to maintain hydration and pain control are the foundation of treatment for peritonsillar abscess. Because peritonsillar cellulitis represents a transitional stage in the development of peritonsillar abscess, its treatment is similar to that of a peritonsillar abscess, excluding the need for surgical drainage.
The main procedures for the drainage of peritonsillar abscess are needle aspiration, incision and drainage, and immediate tonsillectomy. Drainage using any of these methods combined with antibiotic therapy will result in resolution of the peritonsillar abscess in more than 90 percent of cases.6 The acute surgical management of peritonsillar abscess has evolved over time from routine immediate tonsillectomy to increased use of incision and drainage or needle aspiration.11 Immediate abscess tonsillectomy has not been proven to be any more effective than needle aspiration or incision and drainage, and it is considered to be less cost-effective.12 Several studies comparing needle aspiration with incision and drainage have found no significant statistical differences in outcomes.11,12
Although it is not routinely performed for the treatment of peritonsillar abscess, immediate tonsillectomy should be considered for patients who have strong indications for tonsillectomy, including those who have symptoms of sleep apnea, a history of recurrent tonsillitis (four or more infections per year despite adequate medical therapy), or a recurrent or nonresolving peritonsillar abscess.6 Initial empiric antibiotic therapy should include antimicrobials effective against Group A streptococcus and oral anaerobes.13 The most common organisms associated with peritonsillar abscess are listed in Table 3.8,14 Although peritonsillar abscesses are polymicrobial infections, several studies have shown intravenous penicillin alone to be as clinically effective as broader-spectrum antibiotics, provided the abscess has been adequately drained.12,14 In these studies, inadequate clinical response following 24 hours of antibiotic therapy played a significant role in the decision to use broad-spectrum antibiotics. Several other studies have reported that more than 50 percent of culture results demonstrated the presence of betalactamase producing anaerobes, leading many physicians to use broader-spectrum antibiotics as first-line therapy.8,14,15 Table 4 shows suggested antimicrobial regimens.16
| Aerobic bacteria | Anaerobic bacteria |
|---|---|
| Group A streptococcus | Fusobacterium |
| Staphylococcus aureus | Peptostreptococcus |
| Haemophilus influenzae | Pigmented Prevotella |
| Intravenous therapy |
| Ampicillin/sulbactam (Unasyn) 3 g every six hours |
| Penicillin G 10 million units every six hours plus metronidazole (Flagyl) 500 mg every six hours |
| If allergic to penicillin, clindamycin (Cleocin) 900 mg every eight hours |
| Oral therapy |
| Amoxicillin/clavulanic acid (Augmentin) 875 mg twice daily |
| Penicillin VK 500 mg four times daily plus metronidazole 500 mg four times daily |
| Clindamycin 600 mg twice daily or 300 mg four times daily |
Although steroids have been used to treat edema and inflammation in other otolaryngologic diseases, their role in the treatment of peritonsillar abscess has not been extensively studied. A recent study reported that 32 patients who received a single high dose of steroids (methylprednisolone [DepoMedrol] 2 to 3 mg per kg up to 250 mg) intravenously plus antibiotics responded much more quickly to treatment than 28 patients who received antibiotics plus placebo.17 The use of steroids in the treatment of peritonsillar abscess appears to help speed recovery, but additional studies are needed before making a recommendation for their routine use.6,17
When the family physician is inexperienced in treating peritonsillar abscess or when complications or questions arise during treatment, an otolaryngologist should be consulted. Once the diagnosis has been established, drainage or aspiration of the abscess should be performed in a setting where possible airway complications can be managed.3 Peritonsillar aspiration is a technique well suited for the family physician who has had appropriate training. The patient should be observed for a few hours after aspiration to ensure he or she can tolerate oral antibiotics and pain medications. Outpatient follow-up should occur in 24 to 36 hours.18 Oral antibiotics are continued for 10 days.
Most patients with a peritonsillar abscess can be treated in an outpatient setting, but a small percentage (e.g., 14 percent in one study) may require hospitalization.12 Hospital stays usually do not exceed two days and are required for pain control and hydration.