
Am Fam Physician. 2010;82(9):1075-1082
Patient information: See related handout on cold sores, written by the authors of this article.
Author disclosure: Nothing to disclose.
Nongenital herpes simplex virus type 1 is a common infection usually transmitted during childhood via nonsexual contact. Most of these infections involve the oral mucosa or lips (herpes labialis). The diagnosis of an infection with herpes simplex virus type 1 is usually made by the appearance of the lesions (grouped vesicles or ulcers on an erythematous base) and patient history. However, if uncertain, the diagnosis of herpes labialis can be made by viral culture, polymerase chain reaction, serology, direct fluorescent antibody testing, or Tzanck test. Other nonoral herpes simplex virus type 1 infections include herpetic keratitis, herpetic whitlow, herpes gladiatorum, and herpetic sycosis of the beard area. The differential diagnosis of nongenital herpes simplex virus infection includes aphthous ulcers, acute paronychia, varicellazoster virus infection, herpangina, herpes gestationis (pemphigoid gestationis), pemphigus vulgaris, and Behçet syndrome. Oral acyclovir suspension is an effective treatment for children with primary herpetic gingivostomatitis. Oral acyclovir, valacyclovir, and famciclovir are effective in treating acute recurrence of herpes labialis (cold sores). Recurrences of herpes labialis may be diminished with daily oral acyclovir or valacyclovir. Topical acyclovir, penciclovir, and docosanol are optional treatments for recurrent herpes labialis, but they are less effective than oral treatment.
Nongenital herpes simplex virus type 1 (HSV-1) is a common infection that most often involves the oral mucosa or lips (herpes labialis). The primary oral infection may range from asymptomatic to very painful, leading to poor oral intake and dehydration. Recurrent infections cause cold sores that can affect appearance and quality of life. Although HSV-2 also can affect the oral mucosa, this is much less common and does not tend to become recurrent.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Oral acyclovir suspension (Zovirax) is an effective treatment for children with primary herpetic gingivostomatitis. | B | 12 |
| Oral acyclovir, valacyclovir (Valtrex), and famciclovir (Famvir) are effective for the treatment of acute recurrences of herpes labialis. | A | 13–15 |
| Recurrences of herpes labialis are suppressed with daily oral acyclovir or valacyclovir. | A | 13, 19, 20 |
| Topical acyclovir, penciclovir (Denavir), and docosanol (Abreva) are optional treatments for recurrent herpes labialis. | A | 16–18 |
Epidemiology
HSV-1 is initially transmitted in childhood via nonsexual contact, but it may be acquired in young adulthood through sexual contact. In the United States, the seroprevalence of HSV-1 decreased from 62.0 percent between 1988 and 1994 to 57.7 percent between 1999 and 2004.1 In a cross-sectional survey of U.S. college students, the prevalence of HSV-1 antibodies was 37.2 percent in freshmen and 46.1 percent in fourth-year students.2 A history of cold sores was reported in 25.6 percent of freshmen and 28 percent of fourth-year students. Significant predictors of HSV-1 antibodies in this population were female sex, sexual intercourse before 15 years of age, greater total years of sexual activity, history of a partner with oral sores, and personal history of a non-HSV sexually transmitted disease.2 Approximately 90 percent of recurrent HSV-1 infections cause the orofacial lesions known as herpes labialis3 (Figure 1).

Pathophysiology
HSV invades and replicates in neurons, as well as in epidermal and dermal cells. The virus travels from the skin during contact to the sensory dorsal root ganglion, where latency is established. Oral HSV-1 infections reactivate from the trigeminal sensory ganglia, affecting the facial, oral, labial, oropharyngeal, and ocular mucosa.
Primary infection appears two to 20 days after contact with an infected person. The virus can be transmitted by kissing or sharing utensils or towels. Transmission involves mucous membranes and open or abraded skin. During one study of herpes labialis, the median duration of HSV-1 shedding was 60 hours when measured by polymerase chain reaction (PCR) and 48 hours when measured by culture.4
Peak viral DNA load occurred at 48 hours, with no virus detected beyond 96 hours of onset of symptoms.4 Recurrent infections may be precipitated by various stimuli, such as stress, fever, sun exposure, extremes in temperature, ultraviolet radiation, immunosuppression, or trauma. The virus remains dormant for a variable amount of time. Oral HSV-1 usually recurs one to six times per year.5 The duration of symptoms is shorter and the symptoms are less severe during a recurrence.
The likelihood of reactivation of HSV infection differs between HSV-1 and HSV-2, and between the sacral and trigeminal anatomic sites. In one study, the mean monthly frequencies of recurrence were 0.33 genital HSV-2 infections, 0.12 orolabial HSV-1 infections, 0.020 genital HSV-1 infections, and 0.001 oral HSV-2 infections.6 This shows that recurrences are more likely when HSV-1 is oral and HSV-2 is genital.
Clinical Presentation
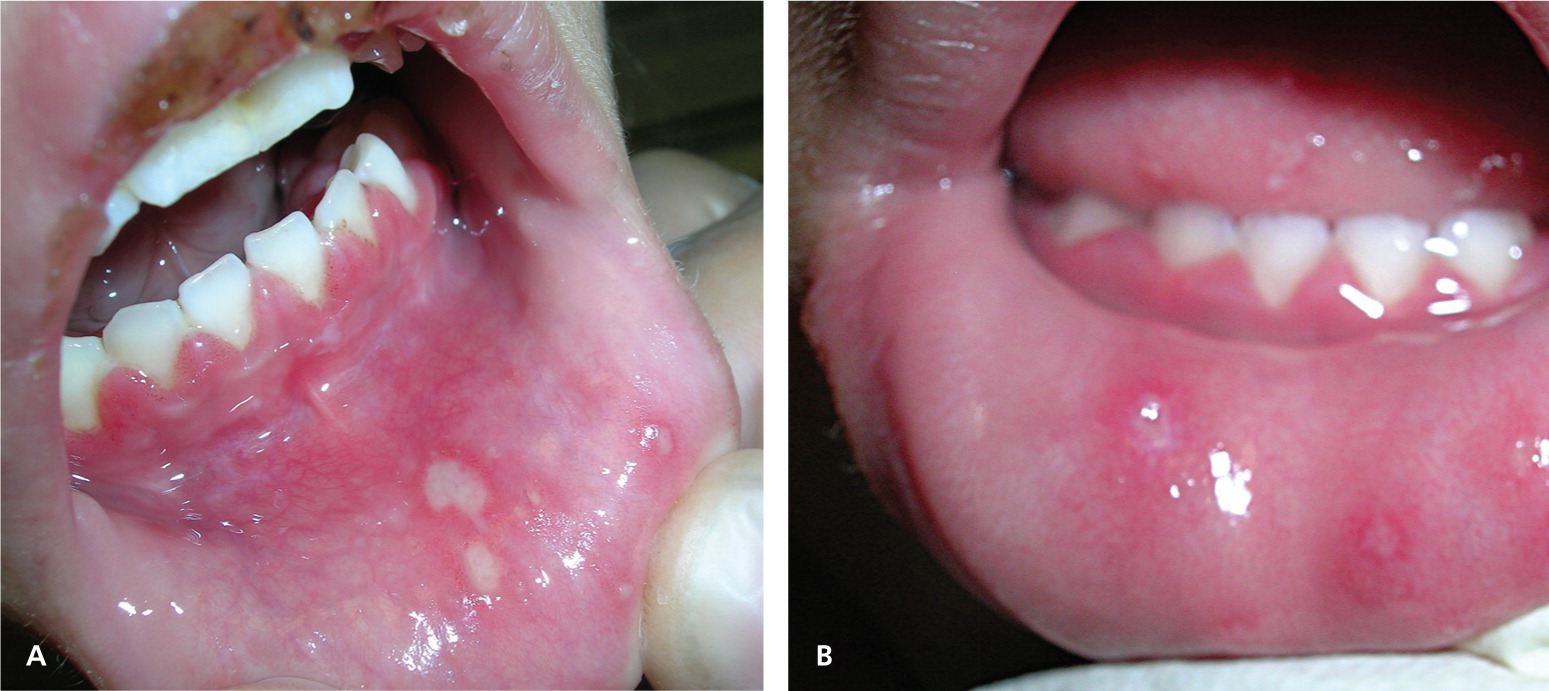
In primary oral HSV-1, symptoms may include a prodrome of fever, followed by mouth lesions with submandibular and cervical lymphadenopathy. The mouth lesions (herpetic gingivostomatitis) consist of painful vesicles on a red, swollen base that occur on the lips, gingiva, oral palate, or tongue. The lesions ulcerate (Figure 2) and the pain can be severe. Refusal to eat or drink may be a clue to the presence of oral HSV. The lesions usually heal within 10 to 14 days.5
In recurrent herpes labialis, symptoms of tingling, pain, paresthesias, itching, and burning precede the lesions in 60 percent of persons.5 The lesions then appear as clusters of vesicles on the lip or vermilion border (Figure 1). The vesicles may have an erythematous base. The lesions subsequently ulcerate and form a crust (Figure 3). Healing begins within three to four days, and reepithelization may take seven to eight days.5 However, many persons who are exposed to HSV-1 demonstrate asymptomatic seroconversion.

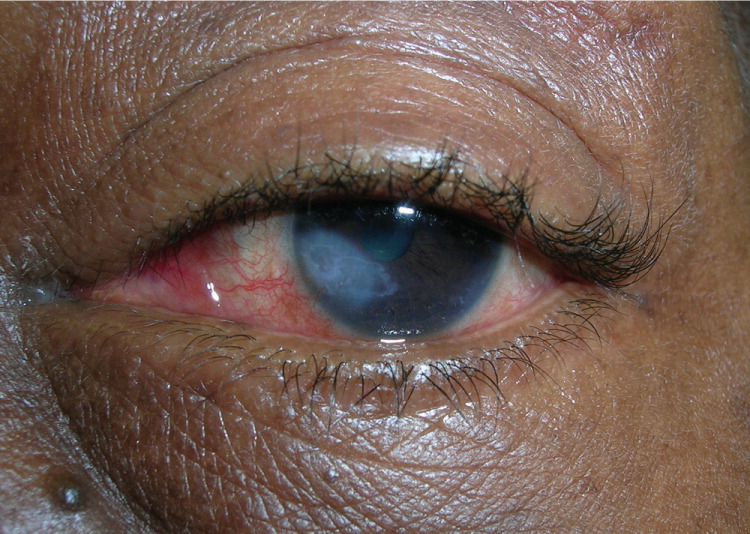
Herpetic keratitis is an HSV infection of the eye. Common symptoms are eye pain, light sensitivity, and discharge with gritty sensation in the eye. Fluorescein stain with a ultraviolet light may show a classic dendritic ulcer on the cornea (Figure 47). Without prompt treatment, scarring of the cornea may occur (Figure 5).

Herpetic whitlow is a vesicular lesion found on the hands or digits (Figures 68 and 7). It occurs in children who suck their thumbs or medical and dental workers exposed to HSV-1 while not wearing gloves. Herpes gladiatorum is often seen in athletes who wrestle, which may put them in close physical contact with an infected person. Vesicular eruptions are often seen on the torso, but can occur in any location where skin-to-skin contact has occurred. Herpetic sycosis is a follicular infection with HSV that causes vesiculopapular lesions in the beard area. It is often caused by autoinoculation from shaving.


HSV infection is one of the most common causes of erythema multiforme (Figure 8), which some patients have with a recurrent HSV infection. The differential diagnosis of HSV-1 infection is presented in Table 1. Herpes gestationis may present like an HSV infection, but it is an autoimmune disease similar to bullous pemphigoid (Figure 9).
| Condition | Identifying features | Diagnosis | Treatment |
|---|---|---|---|
| Acute paronychia | Localized bacterial abscess in a nail fold; has white pus rather than the clear fluid often seen in herpetic whitlow (Figure 68), although the fluid in herpetic whitlow also can become white (Figure 7) | Clinical appearance; can be confirmed with a Gram stain or bacterial culture | Incision and drainage |
| Aphthous ulcers | Similar to the ulcers in the mouth that occur in primary herpetic gingivostomatitis; these ulcers are painful, but the patient is afebrile and not otherwise ill | Clinical appearance; herpes simplex virus culture will be negative | Self-limited, usually no treatment necessary; topical steroids, if needed |
| The cause remains unknown, but these are not viral | |||
| Behçet syndrome | Produces ulcerative disease around the mouth and genitals | Clinical constellation of recurrent oral and genital aphthous-type ulcers; refer to ophthalmologist to look for characteristic eye findings | Tetracycline and topical steroids; may need prednisone and immunosuppressive agents |
| Herpangina | Oral infection with small ulcers caused by Coxsackie virus; ulcers characteristically seen on the soft palate | Clinical presentation | Treat symptoms only |
| Seen in children ages three to 10 years | |||
| Herpes gestationis (pemphigoid gestationis) | Rare blistering eruption that occurs during the second or third trimester of pregnancy; bullae may be seen around the umbilicus, but can occur anywhere on the body (Figure 9) | Skin biopsy to confirm clinical suspicion | Prednisone |
| Herpes zoster (shingles) | Painful clusters of blisters on a red base in a dermatomal distribution | Presence of dermatomal distribution and painful prodrome; direct fluorescent antibody testing of skin scraping can be done | If diagnosed early, may treat with oral acyclovir (Zovirax), valacyclovir (Valtrex), or famciclovir (Famvir) |
| Pemphigus vulgaris | Rare bullous disease that can present with oral ulcers, cutaneous bullae, and erosions | Skin biopsy to confirm clinical suspicion | Oral prednisone and refer to dermatologist immediately |
| Varicella | Caused by a virus in the herpes family; widespread vesiculopustular lesions more concentrated on the face, scalp, and trunk | Its widespread distribution helps to differentiate it from herpes simplex virus; direct fluorescent antibody testing of skin scraping can be done | If diagnosed early, may treat with oral acyclovir |


Diagnosis
The diagnosis of HSV-1 infection is usually made by the appearance of the lesions and the patient's history. However, if the pattern of the lesions is not specific to HSV, its diagnosis can be made by viral culture, PCR, serology, direct fluorescent antibody testing, or Tzanck test. Viral culture should be obtained from vesicles when possible. The vesicle should be unroofed with a scalpel or sterile needle, and a swab should be used to soak up the fluid and to scrape the base. The swab should be sent in special viral transport media directly to the laboratory (or placed on ice if transport will be delayed). Vesicles contain the highest titers of virus within the first 24 to 48 hours of their appearance (89 percent positive).9 In general, viral culture for all types of HSV has a sensitivity of approximately 50 percent.6 Viral isolates usually grow in tissue culture by five days.
PCR is a more sensitive method in the laboratory diagnosis of HSV infection.4 It is useful for the detection of asymptomatic viral shedding. Direct fluorescent antibody testing may be performed from air-dried specimens, and can detect 80 percent of true HSV-positive cases compared with culture results.10 Immunoglobulin G antibodies that are type-specific to HSV develop the first several weeks after infection and persist indefinitely. A Tzanck test is difficult to perform correctly without specific training in its use, but it may be done in the office setting by scraping the floor of the herpetic vesicle, staining the specimen, and looking for multinucleated giant cells. Its results do not specify the type of HSV infection, but if done correctly, its sensitivity is 40 to 77 percent for acute herpetic gingivostomatitis.11
Management
EPISODIC ORAL TREATMENT FOR PRIMARY HERPETIC GINGIVOSTOMATITIS
Oral acyclovir suspension (Zovirax; 15 mg per kg five times per day for seven days) can be used to treat herpetic gingivostomatitis in young children. In one randomized controlled trial (RCT), children receiving acyclovir had oral lesions for a shorter time than children receiving placebo (median of four versus 10 days). The treatment group also had earlier resolution of the following signs and symptoms: fever (one versus three days); eating difficulties (four versus seven days); and drinking difficulties (three versus six days).12 Viral shedding was significantly shorter in the group treated with acyclovir (one versus five days).12 Children should be treated symptomatically with oral analgesics and cold, soothing foods such as ice pops and ice cream. Various concoctions of topical anesthetics and other medications have been used to numb the painful ulcers so that children can be kept well hydrated.
EPISODIC ORAL TREATMENT FOR RECURRENT HERPES LABIALIS
In a Cochrane review on the treatment of herpes labialis in patients receiving cancer treatment, acyclovir was found to be effective with regard to viral shedding (median of 2.5 versus 17.0 days); time to first decrease in pain (median of three versus 16 days); complete resolution of pain (9.9 versus 13.6 days); and total healing (median of 13.9 versus 20.7 days).13 The brief period of viral replication in recurrent herpes labialis lesions suggests short therapeutic regimens should produce good results. In one RCT, 701 patients self-initiated therapy with famciclovir (Famvir; 1,500 mg once [single dose] or 750 mg twice per day for one day [single day]) or placebo within one hour of prodromal symptoms onset.14 Median healing times of primary (first to appear) vesicular lesions in the famciclovir single-dose, famciclovir single-day, and placebo groups were 4.4, 4.0, and 6.2 days, respectively.14 Famciclovir showed decreased healing times, with no significant difference between the divided- or single-dose famciclovir treatment groups.14
In one RCT of recurrent herpes labialis, treatment with oral valacyclovir (Valtrex) plus topical clobetasol (Temovate) was compared with placebo.15 The patients took oral valacyclovir (2 g twice for one day) and applied clobetasol 0.05% gel (twice per day for three days) at onset of symptoms. There were more aborted lesions in the valacyclovirclobetasol group compared with the placebo-placebo group (50 versus 15.8 percent). Combination therapy reduced the mean maximum lesion size (9.7 versus 54 mm) and the mean healing time (5.8 versus 9.3 days) of classic lesions.15
EPISODIC TOPICAL TREATMENT FOR RECURRENT HERPES LABIALIS
Topical treatment for herpes labialis is less effective than oral treatment. An RCT of treatment with topical penciclovir 1% cream (Denavir) showed healing was marginally faster in the penciclovir group compared with placebo (4.8 versus 5.5 days).16 The participants were adults in otherwise good health who had at least three episodes of herpes labialis per year. They applied penciclovir cream or placebo within one hour of the first sign or symptom of a recurrence, and then every two hours while awake for four days. Resolution of symptoms occurred more rapidly in the penciclovir group regardless of whether the medication was applied in the early or late stage. Penciclovir cream applied every two hours while awake reduced median duration of pain from 4.1 to 3.5 days, sped up the healing of classic lesions (e.g., vesicles, ulcers, crusts) from 5.5 to 4.8 days, and did not change median time of viral shedding (median of three versus three days).16
Docosanol cream (Abreva) is a saturated, 22-carbon, aliphatic alcohol with antiviral activity. It is available without prescription. One RCT of 743 patients with herpes labialis showed a faster healing time in patients treated with docosanol 10% cream compared with placebo cream (4.1 versus 4.8 days), as well as reduced duration of pain symptoms (2.2 versus 2.7 days).17 More than 90 percent of patients in both groups healed completely within 10 days.17 Treatment with docosanol cream, when applied five times per day and within 12 hours of episode onset, is safe and somewhat effective.
An RCT of healthy adults with a history of frequent herpes labialis recurrences evaluated treatment with 5% acyclovir cream versus a vehicle control.18 Participants were told to self-initiate treatment five times per day for four days, beginning within one hour of the onset of a recurrent episode. In study 1, the mean duration of episodes was 4.3 days for patients treated with acyclovir cream and 4.8 days for those treated with the vehicle control.18 In study 2, the mean duration of episodes was 4.6 days for patients treated with acyclovir and 5.2 days for those treated with the vehicle control.18
ORAL TREATMENT TO PREVENT HERPES LABIALIS RECURRENCES
Oral acyclovir is effective in suppressing herpes labialis in immunocompetent adults with frequent recurrences. In one RCT, treatment with oral acyclovir (400 mg twice per day) resulted in a 53 percent reduction in the number of clinical recurrences and a 71 percent reduction in virus culture-positive recurrences compared with placebo.19 The median time to first clinically documented recurrence was 46 days for placebo courses and 118 days for acyclovir courses.19 The mean number of recurrences per four-month treatment period was 1.80 episodes per patient during placebo treatment and 0.85 episodes per patient during acyclovir treatment.19
Treatment with oral valacyclovir (500 mg per day) for 16 weeks was compared with placebo in the suppression of herpes labialis in patients with a history of four or more recurrent lesions in the previous year.20 Results showed 60 percent of persons in the valacyclovir group were recurrence-free throughout the study period compared with 38 percent in the placebo group. The mean time to first recurrence was longer with valacyclovir (13.1 weeks) compared with placebo (9.6 weeks).20
In a Cochrane review of herpes labialis prevention in patients receiving treatment for cancer, acyclovir was found to be effective in the prevention of HSV infections, as measured by oral lesions or viral isolates (relative risk = 0.16 and 0.17, respectively).13 There also was no evidence that valacyclovir is more effective than acyclovir. In another study, daily valacyclovir (500 mg per day) and acyclovir (400 mg twice per day) were equally effective in the prevention of recurrent HSV eye disease.21

| Drug | Dose or dosage | Cost of generic (brand)* | Evidence rating† | References |
|---|---|---|---|---|
| Episodic oral treatment for recurrences‡ | ||||
| Acyclovir (Zovirax) | 200 mg five times per day or 400 mg three times per day for five days | 200 mg: $23 ($154)§ 400 mg: $13 ($87) | A | 12, 13 |
| Famciclovir (Famvir) | 1,500 mg once for one day | $173 ($158) | B | 14 |
| Valacyclovir (Valtrex) | 2 g twice for one day | $56 ($74) | B | 15 |
| Episodic topical treatment for recurrences‡ | ||||
| Acyclovir cream | Apply five times per day for four days | 2-g tube: NA ($69) | B | 18 |
| Docosanol cream (Abreva) | Apply five times per day until healed | 2-g tube: NA ($15)∥ | B | 17 |
| Penciclovir cream (Denavir) | Apply every two hours while awake for four days | 1.5-g tube: NA ($54) | B | 16 |
| Treatment to prevent recurrences | ||||
| Acyclovir | 400 mg twice per day (ongoing) | 30-day supply: $29 ($345) | A | 13, 19 |
| Valacyclovir | 500 mg once per day (ongoing) | 30-day supply: $186 ($234) | B | 20 |
