
A more recent article on temporomandibular disorders is available.
Am Fam Physician. 2015;91(6):378-386
Related letter: Temporomandibular Disorder: An Underdiagnosed Cause of Headache, Sinus Pain, and Ear Pain
Patient information: See related handout on temporomandibular disorders, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Temporomandibular disorders (TMD) are a heterogeneous group of musculoskeletal and neuromuscular conditions involving the temporomandibular joint complex, and surrounding musculature and osseous components. TMD affects up to 15% of adults, with a peak incidence at 20 to 40 years of age. TMD is classified as intra-articular or extra-articular. Common symptoms include jaw pain or dysfunction, earache, headache, and facial pain. The etiology of TMD is multifactorial and includes biologic, environmental, social, emotional, and cognitive triggers. Diagnosis is most often based on history and physical examination. Diagnostic imaging may be beneficial when malocclusion or intra-articular abnormalities are suspected. Most patients improve with a combination of noninvasive therapies, including patient education, self-care, cognitive behavior therapy, pharmacotherapy, physical therapy, and occlusal devices. Nonsteroidal anti-inflammatory drugs and muscle relaxants are recommended initially, and benzodiazepines or antidepressants may be added for chronic cases. Referral to an oral and maxillofacial surgeon is indicated for refractory cases.
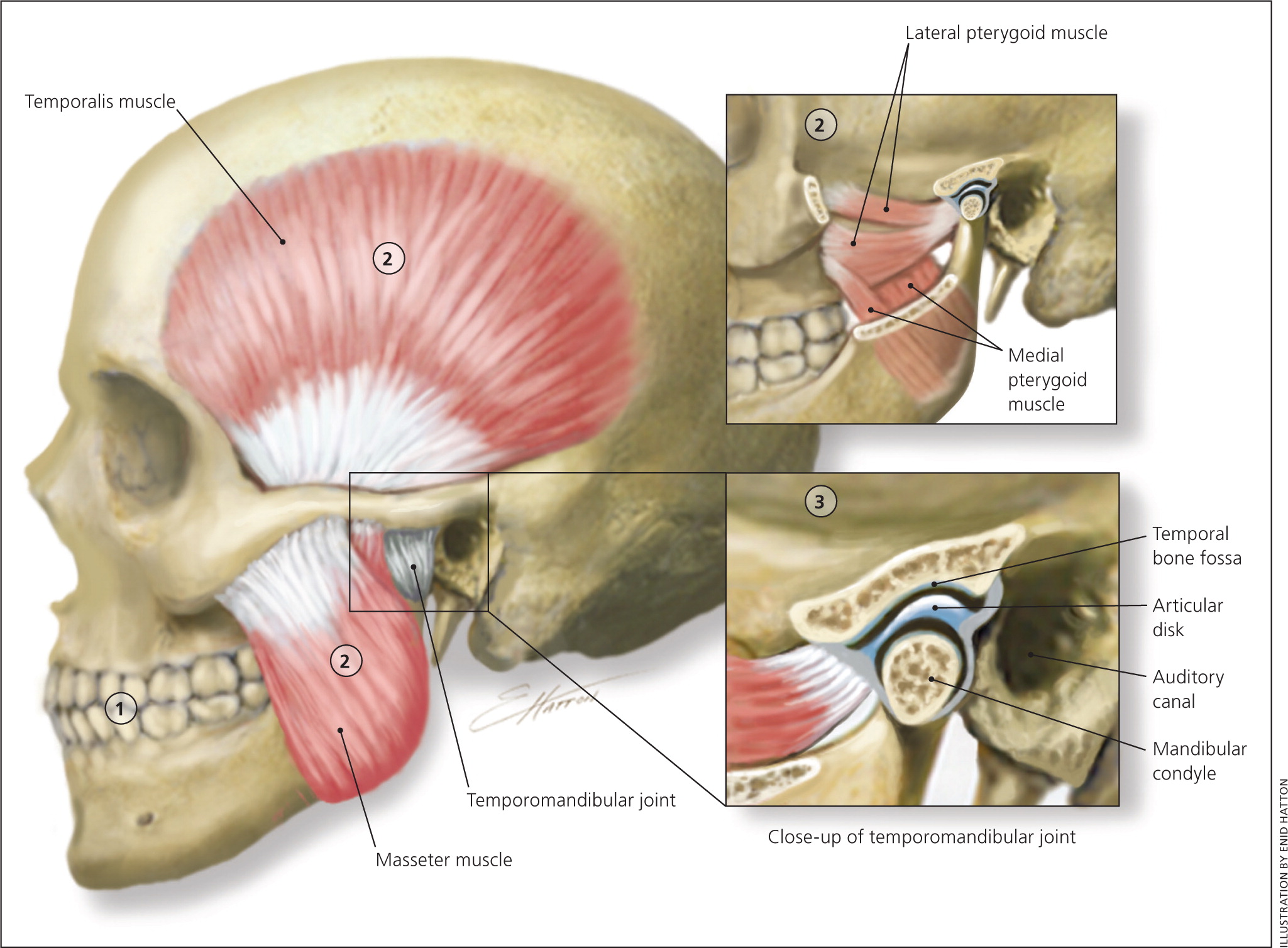
The temporomandibular joint (TMJ) is formed by the mandibular condyle inserting into the mandibular fossa of the temporal bone. Muscles of mastication are primarily responsible for movement of this joint (Figure 1). Temporomandibular disorders (TMD) are characterized by craniofacial pain involving the joint, masticatory muscles, or muscle innervations of the head and neck.1 TMD is a major cause of nondental pain in the orofacial region. Population-based studies show that TMD affects 10% to 15% of adults, but only 5% seek treatment.2,3 The incidence of TMD peaks from 20 to 40 years of age; it is twice as common in women than in men and carries a significant financial burden from loss of work.4 Symptoms can range from mild discomfort to debilitating pain, including limitations of jaw function.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Nonsteroidal anti-inflammatory drugs should be recommended for initial pharmacotherapy of TMD. The addition of a muscle relaxant is recommended if there is clinical evidence of muscle spasm. | C | 37, 44, 47, 51 |
| Cognitive behavior therapy and biofeedback improve short- and long-term pain management for patients with TMD. | B | 10, 36 |
| Occlusal adjustments of the teeth (i.e., grinding the enamel) should not be recommended for the management or prevention of TMD. | B | 61 |
| Referral to an oral and maxillofacial surgeon should be recommended for patients in whom conservative therapy is ineffective and in those with functional jaw limitations or unexplained persistent pain. | C | 10, 14, 62 |
The spectrum for TMD is reflected in its classification (eTable A). The most common syndromes are myofascial pain disorder, disk derangement disorders, osteoarthritis, and autoimmune disorders. The discussion of acute dislocations, trauma, and neoplasia is beyond the scope of this article.
| Articular disorders (intra-articular) | |
| Congenital or developmental disorders | |
| Condylar hyperplasia | |
| First and second branchial arch disorders | |
| Idiopathic condylar resorption | |
| Degenerative joint disorders | |
| Inflammatory: capsulitis, synovitis, polyarthritides (rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Reiter syndrome, gout) | |
| Noninflammatory: osteoarthritis | |
| Disk derangement disorders | |
| Displacement with reduction | |
| Displacement without reduction (closed lock) | |
| Perforation | |
| Infection | |
| Neoplasia | |
| Temporomandibular hypermobility | |
| Dislocation | |
| Joint laxity | |
| Subluxation | |
| Temporomandibular hypomobility | |
| Ankylosis: true ankylosis (bony or fibrous) or pseudoankylosis | |
| Postradiation fibrosis | |
| Trismus | |
| Trauma | |
| Contusion | |
| Fracture | |
| Intracapsular hemorrhage | |
| Masticatory muscle disorders (extra-articular) | |
| Local myalgia | |
| Myofascial pain disorder | |
| Myofibrotic contracture | |
| Myositis | |
| Myospasm | |
| Neoplasia | |
Etiology
The etiology of TMD is multifactorial and includes biologic, environmental, social, emotional, and cognitive triggers. Factors consistently associated with TMD include other pain conditions (e.g., chronic headaches), fibromyalgia, autoimmune disorders, sleep apnea, and psychiatric illness.1,3 A prospective cohort study with more than 6,000 participants showed a twofold increase in TMD in persons with depression (rate ratio = 2.1; 95% confidence interval, 1.5 to 3; P < .001) and a 1.8-fold increase in myofascial pain in persons with anxiety (rate ratio = 1.8; 95% confidence interval, 1.2 to 2.6; P < .001).5 Smoking is associated with an increased risk of TMD in females younger than 30 years.6
Classification
TMD is categorized as intra-articular (within the joint) or extra-articular (involving the surrounding musculature).7 Musculoskeletal conditions are the most common cause of TMD, accounting for at least 50% of cases.8,9 Articular disk displacement involving the condyle–disk relationship is the most common intra-articular cause of TMD.10
In 2013, the International Research Diagnostic Criteria for Temporomandibular Dysfunction Consortium Network published an updated classification structure for TMD (eTable A).
Differential Diagnosis
Clinicians should be vigilant in diagnosing TMD in patients who present with pain in the TMJ area. Conditions that sometimes mimic TMD include dental caries or abscess, oral lesions (e.g., herpes zoster, herpes simplex, oral ulcerations, lichen planus), conditions resulting from muscle overuse (e.g., clenching, bruxism, excessive chewing, spasm), trauma or dislocation, maxillary sinusitis, salivary gland disorders, trigeminal neuralgia, postherpetic neuralgia, glossopharyngeal neuralgia, giant cell arteritis, primary headache syndrome, and pain associated with cancer.11,12 The differential diagnosis and associated clinical findings are presented in Table 1.11,12 TMD symptoms can also manifest in autoimmune diseases, such as systemic lupus erythematosus, Sjögren syndrome, and rheumatoid arthritis.11
| Condition | Location | Pain characteristics | Aggravating factors | Typical findings | Diagnostic studies | Management | |
|---|---|---|---|---|---|---|---|
| Dental conditions | |||||||
| Caries | Affected tooth | Intermittent to continuous dull pain | Hot or cold stimuli | Visible decay | Radiography | Extraction, filling | |
| Cracked tooth | Affected tooth | Intermittent dull or sharp pain | Biting, eating | Often difficult to visualize crack | Radiography | Possible extraction | |
| Dry socket | Affected tooth | Continuous, deep, sharp pain | Hot or cold stimuli | Loss of clot, exposed bone | None | Antibiotics, irrigation | |
| Giant cell arteritis | Temporal region | Sudden onset of continuous dull pain | Visual disturbance, loss of vision | Scalp tenderness, absence of temporal artery pulse | Erythrocyte sedimentation rate, temporal artery biopsy | Corticosteroids | |
| Migraine headache | Temporal region, behind the eye, cutaneous allodynia | Acute throbbing, occasionally with aura | Activity, nausea, phonophobia, photophobia | Often normal, aversion during ophthalmoscopic examination, normal cranial nerve findings | None | Antiemetics, ergot alkaloids, nonsteroidal anti-inflammatory drugs, triptans | |
| Neuropathic conditions | |||||||
| Glossopharyngeal neuralgia | Most often ear, occasionally neck or tongue | Paroxysmal attacks of electrical or sharp pain | Coughing, swallowing, touching the ear | Pain with light touch | Magnetic resonance imaging | Anticonvulsants, surgery | |
| Postherpetic neuralgia | Site of dermatomal nerve and its distribution | Continuous, burning, sharp pain | Eating, light touch | Hyperalgesia | None | Anticonvulsants, tricyclic antidepressants | |
| Trigeminal neuralgia | Unilateral trigeminal nerve | Paroxysmal attacks of sharp pain | Cold or hot stimuli, eating, light touch, washing | Pain with light touch | Magnetic resonance imaging | Anticonvulsants, surgery | |
| Salivary stone | Submandibular or parotid region | Intermittent dull pain | Eating | Tenderness at gland, palpable stone, no salivary flow | Computed tomography, sialography | Often conservative; antibiotics, stone removal | |
| Sinusitis | Maxillary sinus, intraoral upper quadrant | Continuous dull ache | Headache, nasal discharge, recent upper respiratory infection | Tenderness over maxillary sinus or upper posterior teeth | Radiography, computed tomography | Antibiotics | |
Evaluation
DIAGNOSIS
The diagnosis of TMD is based largely on history and physical examination findings. The symptoms of TMD are often associated with jaw movement (e.g., opening and closing the mouth, chewing) and pain in the preauricular, masseter, or temple region. Another source of orofacial pain should be suspected if pain is not affected by jaw movement. Adventitious sounds of the jaw (e.g., clicking, popping, grating, crepitus) may occur with TMD, but also occur in up to 50% of asymptomatic patients.1 A large retrospective study (n = 4,528) conducted by a single examiner over 25 years noted that the most common presenting signs and symptoms were facial pain (96%), ear discomfort (82%), headache (79%), and jaw discomfort or dysfunction (75%).13 Other symptoms may include dizziness or neck, eye, arm, or back pain. Chronic TMD is defined by pain of more than three months' duration.
Physical examination findings that support the diagnosis of TMD may include—but are not limited to—abnormal mandibular movement, decreased range of motion, tenderness of masticatory muscles, pain with dynamic loading, signs of bruxism, and neck or shoulder muscle tenderness. Clinicians should assess for malocclusion (e.g., acquired edentulism, hemifacial asymmetries, restorative occlusal rehabilitation), which can contribute to the manifestation of TMD. Cranial nerve abnormalities should not be attributed to TMD.14 A clicking, crepitus, or locking of the TMJ may accompany joint dysfunction. A single click during opening of the mouth may be associated with an anterior disk displacement. A second click during closure of the mouth results in recapture of the displaced disk; this condition is referred to as disk displacement with reduction. When disk displacement progresses and the patient is unable to fully open the mouth (i.e., the disk is blocking translation of the condyle), this condition is referred to as closed lock. Crepitus is related to articular surface disruption, which often occurs in patients with osteoarthritis.11
Reproducible tenderness to palpation of the TMJ is suggestive of intra-articular derangement. Tenderness of the masseter, temporalis, and surrounding neck muscles may distinguish myalgia, myofascial trigger points, or referred pain syndrome. Deviation of the mandible toward the affected side during mouth opening may indicate anterior articular disk displacement.15
IMAGING
Imaging can assist in the diagnosis of TMD when history and physical examination findings are equivocal.16 Although infrequently used, multiple imaging modalities are available to obtain additional information about suspected TMD etiologies17,18 (eTable B). The initial study should be plain radiography (transcranial and transmaxillary views) or panoramic radiography. Acute fractures, dislocations, and severe degenerative articular disease are often visible in these studies. Computed tomography is superior to plain radiography for evaluation of subtle bony morphology. Magnetic resonance imaging is the optimal modality for comprehensive joint evaluation in patients with signs and symptoms of TMD. Although there is a 78% to 95% correlation between magnetic resonance imaging findings and joint morphology in symptomatic patients,15,19–21 false-positive findings occur in 20% to 34% of asymptomatic patients.22 Magnetic resonance imaging is typically reserved for patients with persistent symptoms, those in whom conservative therapy has been ineffective, or in those with suspected internal joint derangement. Ultrasonography is a noninvasive, dynamic, low-cost technique to diagnose internal derangement of the TMJ when magnetic resonance imaging is not readily available.23
| Condition | Transcranial or transmaxillary radiography* | Panoramic radiography | Computed tomography | Magnetic resonance imaging |
|---|---|---|---|---|
| Arthritides | + | + | ++ | +++ |
| Bony pathology | 0 | 0 | +++ | + |
| Disk position | 0 | 0 | + | +++ |
| Fractures or | + | ++ | +++ | ++ |
| dislocations | ||||
| Inflammatory | 0 | 0 | + | +++ |
| conditions | ||||
| Neoplasia | + | + | +++ | +++ |
DIAGNOSTIC INJECTIONS
Injections of local anesthetic at trigger points involving the muscles of mastication can be a diagnostic adjunct to distinguish the source of jaw pain. This procedure should be performed only by physicians and dentists with experience in anesthetizing the auriculotemporal nerve region. When performed correctly, complication rates are low. Persistent pain after appropriate nerve blockade should alert the clinician to reevaluate TMD symptoms and consider an alternative diagnosis.24
Treatment
Only 5% to 10% of patients require treatment for TMD, and 40% of patients have spontaneous resolution of symptoms.25 In a long-term follow-up study, 50% to 90% of patients had pain relief after conservative therapy.26 A multidisciplinary approach is successful for the management of TMD. Initial treatment goals should focus on resolving pain and dysfunction. More than 1,500 persons in an online TMD registry reported that they had received anti-inflammatory agents (73%), nonprescription pain relievers (56%), antidepressants (50%), opioids (48%), anxiolytics (41%), and muscle relaxants (40%).27 Surgical interventions were reserved for patients whose symptoms did not improve after a trial of conservative therapy. Figure 2 presents an abbreviated treatment algorithm for the nonsurgical management of TMD.
NONPHARMACOLOGIC MANAGEMENT
Supportive patient education is the recommended initial treatment for TMD.28,29 Adjunctive measures include jaw rest, soft diet, moist warm compresses, and passive stretching exercises. TMJ immobilization has shown no benefit and may worsen symptoms as a result of muscle contractures, muscle fatigue, and reduced synovial fluid production.30
Physical Therapy. There is evidence—albeit weak—that supports the use of physical therapy for improving symptoms associated with TMD.31 Techniques may be active or passive (e.g., scissor opening with fingers, use of medical devices) with the goal of improving muscle strength, coordination, relaxation, and range of motion.31 Specialized physical therapy options such as ultrasound, iontophoresis, electrotherapy, or low-level laser therapy have been used in the management of TMD, despite the lack of evidence to support their use.32 Treatment of underlying comorbid conditions results in greater likelihood of success in the management of TMD.
Acupuncture. Acupuncture is used increasingly in the treatment of myofascial TMD. Sessions typically last 15 to 30 minutes, and the mean number of sessions is six to eight.33 Two systematic reviews suggested that acupuncture is a reasonable adjunctive treatment for short-term analgesia in patients with painful TMD symptoms.34,35
Biofeedback. A Cochrane review supports the use of cognitive behavior therapy and biofeedback in both short- and long-term pain management for patients with symptomatic TMD when compared with usual management.36 Patients should be counseled on behavior modifications such as stress reduction, sleep hygiene, elimination of parafunctional habits (e.g., teeth grinding, pencil or ice chewing, teeth clenching), and avoidance of extreme mandibular movement (e.g., excessive opening during yawning, tooth brushing, and flossing).
PHARMACOLOGIC MANAGEMENT
Pharmacologic treatments for TMD are largely based on expert opinion. Several classes of medication are used to treat the underlying pain associated with TMD.
A Cochrane review evaluating nonsteroidal anti-inflammatory drugs (NSAIDs; including salicylates and cyclooxygenase inhibitors), benzodiazepines, anti-epileptic agents, and muscle relaxants initially included 2,285 studies, 11 of which were included in the qualitative synthesis.37 The authors found insufficient evidence to support or refute the effectiveness of any drug for the treatment of TMD.
Results of an evidence-based literature review of various pharmacologic options are shown in Table 2.38–50 NSAIDs are first-line agents typically used for 10 to 14 days for initial treatment of acute pain.44,47,51 Patients with suspected early disk displacement, synovitis, and arthritis benefit from early treatment with NSAIDs. Despite the multiple choices of NSAIDs available, only naproxen (Naprosyn) has proven benefit in reduction of pain.47 Muscle relaxants can be prescribed with NSAIDs if there is evidence of a muscular component to TMD.46 Tricyclic antidepressants—most commonly amitriptyline, desipramine (Norpramin), doxepin, and nortriptyline (Pamelor)—are used for the management of chronic TMD pain. Benzodiazepines are also used, but are generally limited to two to four weeks in the initial phase of treatment.40,44 Longer-acting agents with anticonvulsant properties (i.e., diazepam [Valium], clonazepam [Klonopin], gabapentin [Neurontin]) may provide more benefit than shorter-acting agents. Opioids are not recommended and, if prescribed, should be used for a short period in the setting of severe pain for patients in whom nonopiate therapies have been ineffective. Even with these parameters, opioids should be used cautiously because of the potential for dependence.51
| Medication | Dosage | Evidence | Study | |
|---|---|---|---|---|
| Anticonvulsant: gabapentin (Neurontin) | 300 mg per day, increased by 300 mg incrementally | Statistically significant reduction in pain | Double-blind, placebo-controlled RCT (n = 44)38 | |
| Benzodiazepines | ||||
| Clonazepam (Klonopin) | 0.25 mg every night, increased by 0.25 mg each week to a maximum of 1 mg per day | Conflicting data showing benefit for reduction in pain | Double-blind, placebo-controlled RCT (n = 20)39 | |
| Diazepam (Valium) | 2.5 mg four times per day for one week, then 5 mg four times per day for three weeks | Statistically significant reduction in pain | Double-blind RCT (n = 39)40 | |
| Triazolam (Halcion) | 0.125 mg every night | Improved sleep function, but no statistically significant reduction in symptoms | Double-blind RCT, two-period crossover study (n = 20)41 | |
| Corticosteroids | ||||
| Intra-articular injection (e.g., triamcinolone, methylprednisolone) | Injection of 0.5 mL local anesthetic and 5 to 20 mg steroid using 23- to 27-gauge 0.5- to 1-inch needle | Limited evidence of improved joint function and reduction in pain; should be reserved for severe cases because of reports of articular cartilage destruction | Systematic review of seven double-blind RCTs and two single-blind RCTs42,43 | |
| Systemic | Short course (five to seven days), with or without tapering | Limited evidence; should be reserved for patients with severe joint inflammation associated with autoimmune syndromes | None44 | |
| Hyaluronate (avian) | Single-dose vial, with second injection in two weeks | Inconclusive evidence | Systematic review of seven RCTs45 | |
| Muscle relaxant: cyclobenzaprine (Flexeril) | 10 mg every night | More effective than clonazepam and placebo for reduction in pain | Double-blind, placebo-controlled RCT (n = 39)46 | |
| Nonsteroidal anti-inflammatory drugs | ||||
| Celecoxib (Celebrex) | 100 mg two times per day | No statistically significant reduction in pain | Double-blind, placebo-controlled RCT (n = 68)47 | |
| Diclofenac | 50 mg three times per day | No statistically significant reduction in pain | Double-blind, placebo-controlled RCT (n = 32)48 | |
| Ibuprofen | 600 mg four times per day | No statistically significant reduction in pain; combination of ibuprofen and diazepam was more effective than placebo | Double-blind, placebo-controlled RCT (n = 39)40 | |
| Naproxen (Naprosyn) | 500 mg two times per day | Statistically significant reduction in pain | Double-blind RCT (n = 68)47 | |
| Piroxicam (Feldene) | 20 mg per day | No statistically significant reduction in pain | Double-blind, placebo-controlled RCT (n = 41)49 | |
| Tricyclic antidepressant: amitriptyline | 25 mg per day | Statistically significant reduction in pain | Double-blind RCT (n = 12)46,50 | |
Medications that have limited or no effectiveness for the treatment of TMD include tramadol (Ultram), topical medications (e.g., capsaicin [Zostrix], lidocaine, diclofenac52), and newer antidepressants (e.g., selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, monoamine oxidase inhibitors).37
There has been a limited number of studies investigating the effectiveness of onabotulinumtoxinA (Botox) in the management of TMD.53 Early small randomized controlled trials have shown promising results for the improvement of painful myofascial symptoms.54–56 However, a recent Cochrane review (four studies, N = 233) found inconclusive evidence to support use of onabotulinumtoxinA for myofascial pain.57 Only one of the four studies demonstrated benefit with this modality.
OCCLUSAL SPLINTS AND ADJUSTMENTS
The use of occlusal splints is thought to alleviate or prevent degenerative forces placed on the TMJ, articular disk, and dentition.58 These devices may benefit a select population of patients with severe bruxism and nocturnal clenching. Systematic reviews have shown conflicting results on the preferred occlusal device for relieving TMD symptoms.59,60 Dental consultation should be obtained to determine the optimal occlusal device. Occlusal adjustments (i.e., grinding enamel surfaces to improve dentition) have no benefit in the management or prevention of TMD.61
Referral
Referral to an oral and maxillofacial surgeon is recommended if the patient has a history of trauma or fracture to the TMJ complex, severe pain and dysfunction from internal derangement that does not respond to conservative measures, or pain with no identifiable source that persists for more than three to six months.10,14,62 Surgery is rarely required for treatment of TMD and is usually reserved for correction of anatomic or articular abnormalities.1 Surgical options include arthrocentesis, arthroscopy, diskectomy, condylotomy, and total joint replacement.
Data Sources: An OvidSP search was completed using the key terms temporomandibular joint disorders, temporomandibular disorders, headache, diagnosis, acupuncture, treatment, occlusal splints, occlusal adjustment, pharmacotherapy, randomized controlled trials, meta-analysis, botulinum toxin, differential diagnosis, biofeedback, cognitive behavior therapy, physical therapy, and classification. Additional literature searches included the Cochrane library, UpToDate, Essential Evidence Plus, International Association for Dental Research, and the TMJ Association, Ltd. (http://www.tmj.org). Search dates: December 22, 2013; April 8, 2014; and November 6, 2014.
The authors thank Katrease Gauer for her assistance with the manuscript.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Medical Department of the U.S. Army or the U.S. Army Service at large.
