
Am Fam Physician. 2016;93(9):783-784
Author disclosure: No relevant financial affiliations.
A 60-year-old woman presented with enlarging ulcers on her ankle and foot. Despite treatment, the ulcers worsened and became more painful, and she noted a new ulcer on her left shin. The problem started as a small ulcerated lesion on the lateral dorsal area of her foot that had developed two years earlier after she bumped into a dresser.
She had a history of diabetes mellitus, hypertension, hyperlipidemia, and myeloproliferative disease. At the time of presentation, her medications included enalapril (Vasotec), metoprolol, furosemide (Lasix), fenofibrate (Tricor), insulin aspart (Novolog), insulin detemir (Levemir), metformin, prednisone, dapsone, topical silver sulfadiazine (Silvadene), and clobetasol cream (Temovate). She was previously taking hydroxyurea and anagrelide (Agrylin) for her myeloproliferative disease. She was a nonsmoker.
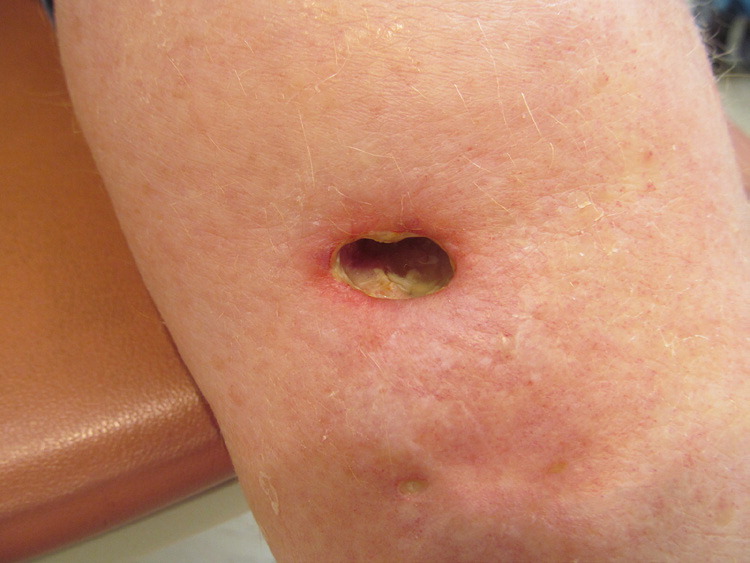
On examination, she was afebrile and had ulcers of varying size on her left lower leg over the lateral malleolus and foot (Figures 1 and 2). There were larger ulcerations exposing muscles and tendons, with sharp margins, an undermined and violaceous border, and granulation tissue over the ulcer beds. A smaller area of ulceration was noted in the left midpretibial area. A complete blood count revealed a white blood cell count of 17,200 per mm3 (17.2 × 109 per L). Her blood glucose level was 126 mg per dL (7.0 mmol per L). Findings from Doppler ultrasonography and wound cultures were unremarkable.

Question
Discussion
The answer is D: pyoderma gangrenosum. Pyoderma gangrenosum is an inflammatory, noninfectious, ulcerative skin disorder characterized by rapidly enlarging, painful lesions. Although the most common sites of involvement are the lower legs, buttocks, and abdomen, it may occur anywhere, including on mucosal surfaces.1,2 Multiple lesions are usually present.1 It is most common in adults 40 to 60 years of age.3 It is rare in children, but head and anogenital involvement is more common in children than in adults.1,2
There are four variants: ulcerative, pustular, bullous, and vegetative. These variants may occur simultaneously.1 Lesions begin as tender pustules or erythematous nodules that enlarge, undergo necrosis, and then ulcerate.2 A primary lesion is not always seen. Fully developed lesions are sharply marginated, undermined ulcers with violaceous borders.3 The condition may develop spontaneously or at the site of trauma. Postsurgical pyoderma gangrenosum may be misdiagnosed as wound dehiscence or infection.1 Because there are no diagnostic serologic or histologic features, pyoderma gangrenosum is diagnosed through exclusion.3 An underlying chronic disease is present in around 50% of patients.3 Inflammatory bowel disease is the most common association, but other conditions that have been reported include rheumatoid arthritis and myeloproliferative diseases.4
Factitial ulcers may be suspected in patients with a history of psychiatric disease. The patient may present with geometric, unusual shaped lesions. These ulcers generally heal quickly if there is no repeated trauma.5
Bacterial, deep fungal, parasitic, and atypical mycobacterial infections can lead to ulcers. A travel history is important in considering tropical and parasitic diseases such as amebiasis and leishmaniasis. Tissue culture may be required for diagnosis.5
| Condition | Location | Characteristics |
|---|---|---|
| Cutaneous malignancies | Anywhere on skin | May be a result of squamous cell carcinoma, basal cell carcinoma, or melanoma; nonhealing ulcers |
| Factitial ulcers | More common on the extremities | Geometric, unusual shaped lesions; associated with psychiatric disease |
| Infectious ulcers | Anywhere on skin | May be caused by bacterial, deep fungal, parasitic, or atypical mycobacterial infections; diagnosed with tissue culture |
| Pyoderma gangrenosum | Most common on the lower leg | Sharply marginated, undermined ulcers with violaceous borders; associated with several chronic diseases such as inflammatory bowel disease; may occur after minor trauma |
| Venous stasis ulcers | Typically on the medial aspects of the lower legs | Nonhealing ulcers; associated with chronic venous insufficiency; comprise up to 80% of leg ulcers |