
Am Fam Physician. 2020;101(9):567-568
Author disclosure: No relevant financial affiliations.
A 40-year-old man presented with a 10-day history of a worsening rash that began on his legs and advanced to his lower abdomen. The rash was red and nonpruritic. The patient also had muscle aches, mild abdominal discomfort, and a recent sore throat. His medical history included diabetes mellitus, hypertension, and cirrhosis due to non-alcoholic steatohepatitis. His long-term medications were insulin degludec (Tresiba), semaglutide, and lisinopril.
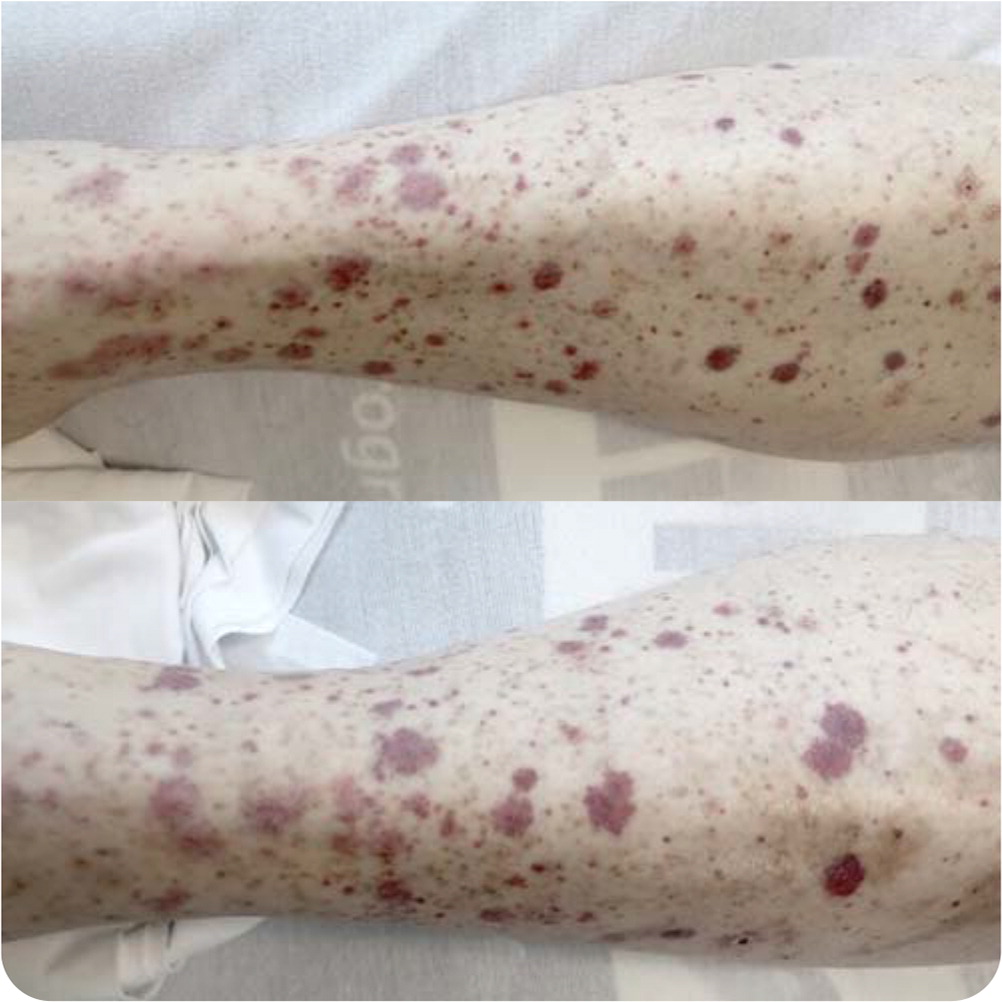
Physical examination revealed a nontender, symmetrical, petechial, and purpuric rash from the soles of the feet to the lower abdomen (Figures 1 and 2). His physical examination was otherwise unremarkable, including normal vital signs. His platelet count was low at 110 × 103 per μL (110 × 109 per L), but findings on a complete blood count and basic metabolic panel were otherwise normal. Urinalysis revealed 10 to 25 red blood cells per high-power field without protein. Recent laboratory tests were negative for hepatitis.

Question
Discussion
The answer is E: IgA vasculitis. IgA vasculitis, formerly known as Henoch-Schönlein purpura, is a systemic small-vessel vasculitis characterized by deposition of immune complexes containing IgA. Approximately 90% of cases occur in children four to seven years of age, but it rarely occurs in older age groups and can be more severe in adults.1 The purpuric rash, a hallmark of a small-vessel leukocytoclastic vasculitis, is commonly accompanied by arthralgias and abdominal pain. IgA vasculitis is often preceded by an infection, such as an upper respiratory tract infection. Kidney involvement is common, manifesting as hematuria or proteinuria.
Skin biopsy can confirm the diagnosis. Deposition of IgA in dermal vessels confirms the diagnosis and rules out other causes of leukocytoclastic vasculitis. IgA vasculitis often resolves in one to two months without treatment. Acetaminophen or nonsteroidal anti-inflammatory drugs can be used to relieve arthralgias or abdominal discomfort. Patients with more severe cases and significant kidney involvement should be referred to a nephrologist for consideration of steroid or immunosuppressive therapy.
ANCA-associated vasculitis involves necrotizing inflammation of small- to medium-sized vessels and includes granulomatosis with polyangiitis, eosinophilic granulomatosis with polyangiitis, and microscopic polyangiitis. Pulmonary manifestations and glomerulonephritis are common.2 ANCA testing is appropriate in all cases of lower extremity palpable purpura.
Cryoglobulinemia can cause vasculitis from blood vessel deposition of cryoglobulins.3 These proteins precipitate at temperatures below normal body temperature and can be associated with acral purpura, arthralgias, generalized weakness and fatigue, peripheral neuropathy, and glomerulonephritis. Hypocomplementemia is common with cryoglobulinemia, and there is a strong association between cryoglobulinemia and chronic hepatitis C infection.
Drug-induced leukocytoclastic vasculitis can cause petechiae and purpura indistinguishable from many other small-vessel vasculitides. It is characterized by immune complex deposition in small vessels. The rash usually develops within seven to 21 days of drug exposure. Medications that commonly cause leukocytoclastic vasculitis include beta-lactam antibiotics, sulfonamides, thiazides, allopurinol, and quinolones. Use of monoclonal antibody agents is an increasingly common cause.4 Discontinuation of the causative agent usually results in resolution of the cutaneous findings.
Immune thrombocytopenic purpura is an autoimmune condition with antibodies against several platelet surface antigens. Petechiae and purpura are common when the platelet count is severely low, whereas systemic symptoms, such as arthralgias or abdominal discomfort, are not present. Treatment with corticosteroids is generally not initiated until the platelet count is less than 30 × 103 per μL (30 × 109 per L).5
| Condition | Characteristics | Cause |
|---|---|---|
| ANCA-associated vasculitis | Pulmonary manifestations and glomerulonephritis are common | Necrotizing inflammation of small- to medium-sized vessels, with ANCA |
| Cryoglobulinemia vasculitis | Acral purpura, arthralgias, generalized weakness and fatigue, peripheral neuropathy, glomerulonephritis | Mixed cryoglobulinemia commonly due to chronic hepatitis C infection |
| Drug-induced leukocytoclastic vasculitis | Petechiae and purpura that develop within seven to 21 days of medication exposure | Immune complex deposition in small vessels |
| Immune thrombocytopenic purpura | Petechiae and purpura are common when platelet count is very low, without associated systemic symptoms | Autoimmune condition with antibodies against several platelet surface antigens |
| Immunoglobulin A vasculitis | Purpura accompanied by arthralgias, abdominal pain, hematuria, and proteinuria; often preceded by an upper respiratory tract infection | Deposition of immune complexes containing immunoglobulin A |
