National Conference Q&A: Look to the Future
July 15, 2024, David Mitchell — With the 50th anniversary approaching for the National Conference of Family Medicine Residents and Medical Students when it meets Aug. 1-3 in Kansas City, Mo., AAFP News gathered six past student and resident chairs whose leadership experiences span the event’s half-century.
So far this four-part series, family medicine leaders have shared their thoughts on the beginnings, evolution and growth of National Conference and the event’s vital role in helping students choose the specialty, find residency programs, connect with mentors and become future leaders of the specialty.
In this final installment, they offer their insights on the future of the specialty itself.
What are your hopes for the future of the specialty and what our future family physicians will accomplish in the next 50 years?
Daniel Lewis, M.D., FAAFP, resident chair 2006; current chair of the National Conference Planning Subcommittee: I look for continued growth and continued service to the country by family physicians. We obviously don’t have enough family physicians to fill the needs that are currently there nor the need that is forecasted to be there.
There’s a lot of angst about us being replaced by midlevel providers in primary care, or AI computers in primary care. It’s not a concern that I have.

Keck School of Medicine student Julia Wang (fourth from right) stands with students and residents from California during the 2019 National Conference of Family Medicine Residents and Medical Students in Kansas City, Mo. During that event, Wang was elected student chair of the 2020 National Conference.
There are 27 states that allow independent practice for NPs and five states for PAs, and family physicians are thriving in each and every one of them. Studies have shown that primary care and family medicine is the most difficult specialty to do via artificial intelligence because of the wide variety of things you have to know and the relationship-based aspect of it.
I want to see a future that’s thriving with increasing numbers of opportunities for medical students who choose family medicine. Seeing the folks like Julia who came behind me and seeing just how passionate they are makes me excited about what the future holds.
Beulette Hooks, M.D., FAAFP, student chair 1993, Resident chair 1996: What we do is take care of families. And that is always going to be needed. And we have to let the students and the residents behind us know that this is a good profession. This is something to look forward to doing, and it doesn’t have to be done one way. You can go in the military. You can work in a rural area. You can work in an urban area. You can work in a suburb. It’s not someplace where you have to say, “Well, I can only do this or that.” It is a wonderful profession, and if we get out the right message out, we will continue to have students who are interested in family medicine.
Marla Tobin, M.D., FAAFP, student chair 1980, resident chair 1982 and 1983: Family medicine should be and needs to be the anchor of our country’s health care system. When you look at the health care system right now, there’s never been a time that we needed more family doctors. It needs our specialty to make cost-effective, good decisions and try to get America back on track in terms of being a healthy country. There are so many communities that need family docs, and there are so many family docs who need to reestablish their foothold in the community, the hospitals, the government agencies, and the different kinds of hospital processes, elder care and pediatric care and wellness and everything else that we do — women’s health, especially — there’s just so much we need to do that we need to support each other to be strong and grow the field as much as we can to make it the anchor.
Douglas Henley, M.D., FAAFP, resident chair 1980: The future of the discipline has the potential to be very bright, and Danny alluded to this. I think a big part of that very well can be the proper integration of artificial intelligence into EHRs and practice, both in terms of reducing and eliminating a lot of administrative burden; and also, family physicians utilizing evidence-based content at the point of care and moving upstream with less need for many subspecialty referrals or consultations.
But there are things that can hold us back. It has taken me a long time to get over this, but I think we should not worry so much about the scope of practice challenges of nurse practitioners and PAs. They’re going to be around so why not effectively integrate them into your practice as I did for 20 years. I haven’t met a family physician yet in those states that have so-called independent practice for NPs and PAs who aren’t overwhelmed by their patient volume, so there are plenty of patients to go around and maintain an active healthy practice regardless of how many NPs or PAs may be around in a given region, much less in your practice. I like this perspective that FPs should embrace: “All members of the health care team are important, but they are not interchangeable.”
What I worry most about is the current consolidation and corporatization occurring in medicine that’s trying to make primary care a commodity. That’s just the wrong way for this country to go. And I worry that this consolidation and corporatization, including large health systems, is putting pressure on our discipline to narrow its scope – we should not allow this to happen when research data clearly shows that comprehensiveness in family medicine leads to better outcomes, lower costs, and less physician burnout.
Alan David, M.D., resident chair 1974-75: Go back historically a little bit. The people who were GPs when there were no training programs went out and practiced after a year of internship. More had a surgical personality. They wanted to go out there and do it and fix it, fix fractures, minor surgery. Some people learned to do major surgery, gallbladder and appendectomies in small towns.
When family medicine got going, the personality started to change to a little bit more of a behavioral, less of an interventional, but not completely, mentality. And yet family medicine physicians went into it with this comprehensive, I want to take care of patients, infants. I want to, for the most part, do obstetrics if I can. I want to take care of people at the hospital. I want to be their all-around family doctor.
As the world got more complicated, as information, not necessarily knowledge, but information exploded, it was harder to do that. People started to branch off with CAQs in geriatrics, sports medicine, things of that nature. People became employed by health systems. Health systems don’t want you to do much in the way of procedural medicine. So, what my concern is, and what my hope for this specialty is, we maintain a broad perspective. Is that necessarily for everybody? No, but how could we maintain that or develop it, not just around individuals, but around groups?
If you have a division of interest, a division of talent within a large group, or a medium-size group, can you provide the range of services? And yet everybody has an ongoing continuity practice of patients they take care of for all their basic problems. But how they divide their time different. Is that the best model? I don’t know. I think some large groups have accomplished that.
We’re not doing much pediatrics. We’re not doing much obstetrics, depending on where you are. And I would hope we don’t lose that. I want to be able to say that I go see my family doctor, and he or she is very capable and with a wide range of abilities, skills and interests. And that person’s patients not only are treated well, but they are treated comprehensively in a personal, longitudinal capacity.
I think one of the major efforts, not only family medicine, but other primary care specialties, need to do and continue to do is alter the landscape, whether it’s through national health care or a modified model to say, where do people start? They start with the primary care physician. My brother’s primary care physician in Chicago at Northwestern is retiring. They can’t find anybody who has a practice he can go to.
We’re producing a lot of people, but in the conditions of practice, the conditions of reimbursement and the conditions of respect, there’s work that needs to be done. I don’t have the answer. But if you talk to somebody in Canada, people there start with their family doc. That’s where we ought to begin.
Julia Wang, M.D., student chair 2020: I spent the last six months doing a reproductive health and advocacy fellowship here in Boston. The focus is figuring out how do we provide reproductive justice to all patients in the United States, and abortion care is such a hot topic at the moment.
Meet the Panel
Alan David, M.D.
Then: Resident chair from the University of Missouri Family Medicine Residency in 1974 and 1975
Now: Retired chair of the Department of Family Medicine and an associate dean at the Medical College of Wisconsin; Granville, Ohio
Other notable roles: Former president of STFM (1991); Also served on the boards of the Association of Departments of Family Medicine and the ABFM

Douglas Henley, M.D., FAAFP
Then: Resident chair from the University of North Carolina Family Medicine Residency in 1980
Now: President, Henley Health Care Consulting; Loch Lloyd, Mo.
Other notable roles: North Carolina AFP president (1987-1989); AAFP president (1995-96); AAFP Board chair (1994-95, 1996-97); AAFP executive vice president/CEO (2000-2020); chair of the Patient Centered Primary Care Collaborative (2015-17)

Marla Tobin, M.D., FAAFP
Then: Student chair from University of Missouri in 1980; resident chair from Duke University Family Medicine Residency in 1982 and 1983
Now: Retired Aetna Inc. regional senior medical director, who previously practiced full-scope family medicine in rural Missouri, Warrensburg, Mo.
Other notable roles: Inaugural convener of the National Conference of Women, Minority, and New Physicians (now the National Conference of Constituency Leaders) in 1990; Missouri AFP president (1993-94)

Beulette Hooks, M.D., FAAFP
Then: Student chair from the Mercer University School of Medicine in 1993; resident chair from Atrium Health Navicent /Mercer University School of Medicine Family Medicine Residency in 1996
Now: Medical director for the Family Medicine Clinic at Martin Army Community Hospital, Fort Moore, Ga.
Other notable roles: President of the Georgia AFP (2011-2012); convener of the National Conference of Special Constituencies (now the National Conference of Constituency Leaders) in 2006

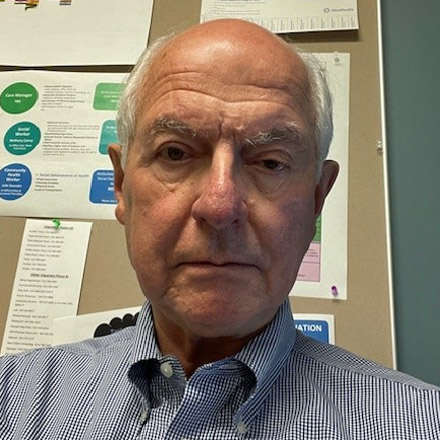
Daniel Lewis, M.D., FAAFP
Then: Resident chair from Self Regional Health Care Family Medicine Residency in 2006
Now: VP and CMO of Southern Market for Ballad Health/Wellmont Health Systems, Greeneville Tenn.
Other notable roles: Member of the Commission on Education and chair of the National Conference Planning Subcommittee; president of the Tennessee AFP (2020-21); resident member of the AAFP Board of Directors (2007-08)

Julia Wang, M.D.
Then: Student chair from Keck School of Medicine in 2020
Now: Reproductive Health and Advocacy Fellow, Tufts Cambridge Health Alliance; Family medicine attending, Cambridge Health Alliance Primary Care, Malden, Mass.
Other notable roles: Student delegate to the AAFP Congress of Delegates; student member of the AAFP Commission on Education
Family physicians also provide gender-affirming care, care for refugees, immigrants, the asylum seekers, the homeless population, folks really on the outskirts of our traditional medical health care system. My hopes are bringing in continually large groups of really activated and motivated students and residents who not only come from these populations, but also really passionate about changing the way that that our health care system views these patients, because if we don’t lift that bottom floor for everybody, then there’s no way for us to improve the health care system at all.
Finally, are there things you want people to know about National Conference that we haven’t covered?
Henley: The Family Medicine Experience and the Congress of Delegates are important to the Academy for a whole host of reasons. National Conference is important to the future of the discipline. I think it’s the most important meeting that the Academy puts on every year. I think it’s more important than FMX and COD.
Marla: It’s a lifeline.