
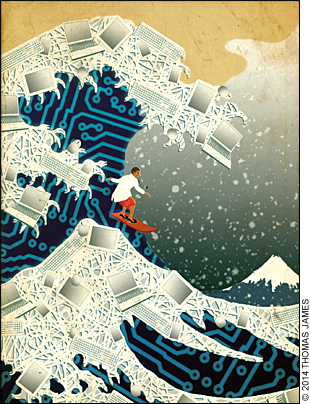
You need to prepare for the next round of electronic health record requirements to keep it from swamping your practice.
Fam Pract Manag. 2014;21(1):19-24
Author disclosures: no relevant financial affiliations disclosed.
For the past three years, many physicians and other eligible professionals have worked to comply with Stage 1 of the Centers for Medicare & Medicaid Services' (CMS's) electronic health records (EHR) meaningful use program. Beginning in 2014, those professionals who have completed two years of Stage 1 (or three years if they were an early demonstrator of meaningful use in 2011) must begin on Stage 2, which makes significant changes to the existing criteria and adds a few new rules.
This article details the major differences between Stage 1 and Stage 2 requirements of meaningful use. We will also touch on leveraging components of meaningful use to provide excellent care for your patients as well as developing a strategy for adjusting and adapting for future stages of meaningful use.
We have included some online resources that deal more in depth with other Stage 2 topics, such as provider registration and changes in technology certification (see “Additional meaningful use resources”).
ADDITIONAL MEANINGFUL USE RESOURCES
Registration
Medicare EHR Incentive Program: Registration User Guide for Eligible Professionals (Centers for Medicare & Medicaid Services)
Steps to Register for Meaningful Use (American Academy of Family Physicians [AAFP] Center for Health Information Technology)
Certified EHR Technology
Certified EHR Technology Products (AAFP Center for Health Information Technology)
Certified Health Information Technology Product List (Office of the National Coordinator for Health Information Technology)
Other
Meaningful Use and Your Practice (AAFP Center for Health Information Technology)
Structural changes in meaningful use
In Stage 2, the level of Medicare incentive payments declines steadily and, beginning in 2015, gives way to financial penalties of 1 percent for those who aren't meaningful users, increasing to 3 percent in 2017. (See “Meaningful use incentive/penalty timeline (Medicare)” and “Meaningful use incentive/penalty timeline (Medicaid)”.) We believe that meaningful use Stage 2 represents significantly more work for about half the money you would have achieved through Stage 1. For example, physicians who began meaningful use in 2012 are eligible for up to $30,000 in incentives in Stage 1 compared with up to $14,000 in Stage 2. And it's still not clear how much additional investment practices will have to make to upgrade their technology or change clinical and operational workflows.
There are five policy priorities that the Office of the National Coordinator for Health Information Technology and CMS are trying to accomplish through the meaningful use program – improving quality, safety, efficiency, and reducing health disparities; engaging patients and families in their health care; improving care coordination; improving population and public health; and ensuring adequate privacy and security protections for personal health information. These policies are broken out into the objectives that meaningful users must perform by completing the required measures.
In Stage 1, eligible professionals could satisfy the requirements by completing 20 of 25 objectives, each of which had one measure. In Stage 2, an eligible professional must still complete 20 objectives, but four of the required objectives now have two or more measures that need to be satisfied. This means that in Stage 2 one must satisfy a total of 26 measures.
Of those, more than half represent existing Stage 1 measures, most with either a larger scope or a higher threshold, and about half are completely new. Six Stage 1 measures are being “retired” even though you will still need to perform them to complete other objectives in Stage 2.
On top of this are the clinical quality measures that eligible professionals must report to CMS. That number has increased from six to nine in Stage 2, and all providers must now report those measures whether they are participating in meaningful use or not. Providers can use the Physician Quality Reporting System (PQRS) to report these measures, an option they didn't have in Stage 1.
All of these changes mean that although you may hear CMS and others say that there's not a big jump in the quantity of things you have to do from Stage 1 to Stage 2, they are talking about the number of objectives and not measures.
Mighty morphing Stage 1 objectives
The table “Meaningful use Stage 2 objectives and measures” lists the core set (complete all 17) and menu set (complete three of six) objectives required for Stage 2, but we'll focus first on the ones that differ significantly from what was required in Stage 1. For example, the Stage 1 objective for computerized physician order entry required that 30 percent of patients who had at least one medication in their medication list had at least one medication ordered through the entry system. In Stage 2, more than 60 percent of medication orders have to be entered into the system electronically. Stage 2 also requires that more than 30 percent of laboratory orders and more than 30 percent of radiology orders must be entered electronically.
| Core Set (must complete all 17) | |
|---|---|
| Objectives | Measures |
| Use computerized physician order entry (CPOE)* | More than 60 percent of medication orders, more than 30 percent of laboratory orders, and more than 30 percent of radiology orders are recorded using CPOE. |
| Implement electronic prescribing (eRx)* | More than 50 percent of all permissible prescriptions are queried for a drug formulary† and transmitted electronically. |
| Record patient demographics (preferred language, gender, race, ethnicity, and date of birth)* | More than 80 percent of patients have demographics recorded as structured data. |
| Record and chart changes in vital signs* | More than 80 percent of all patients have blood pressure (age 3 and older only), height, and weight recorded as structured data. |
| Record smoking status* | More than 80 percent of patients age 13 and older have smoking status recorded as structured data. |
| Use clinical decision support to improve performance on high-priority health conditions* | Implement five clinical decision support interventions related to four or more clinical quality measures. Absent four clinical quality measures related to scope of practice or patient population, interventions must be related to high-priority health conditions. Enable functionality for drug-drug and drug-allergy interaction checks.* |
| Give patients the ability to view online, download, and transmit their health information | More than 50 percent of all patients are provided electronic access to their health information within four business days of it being updated in the electronic health record (EHR). More than 5 percent of all patients view, download, or transmit to a third party their health information. |
| Provide clinical summaries for patients for each office visit* | Provide clinical summaries to patients for more than 50 percent of office visits within one business day. |
| Protect electronic health information created or maintained by the certified EHR technology* | Conduct or review a security risk analysis, implement security updates as necessary, and correct identified security deficiencies. Also, ensure data is stored according to encryption/storage of data regulations. |
| Incorporate clinical laboratory results as structured data† | More than 55 percent of all lab test results reported in a positive/negative or numerical format are incorporated in the EHR as structured data. |
| Generate lists of patients by conditions† | Generate at least one report that lists patients with a specific condition. |
| Identify patients needing preventive/follow-up care and send reminders, per patient preference† | More than 10 percent of all patients who have had two or more office visits in the last two years are sent an appropriate reminder. |
| Provide patient-specific education resources to the patient as appropriate† | More than 10 percent of all patients are sent patient-specific education resources. |
| Perform medication reconciliation whenever appropriate† | Perform medication reconciliation for more than 50 percent of patients arriving from another care setting. |
| Provide summary of care records† | Provide a summary of care record for more than 50 percent of patient referrals or transitions of care (expected to include an up-to-date problem list of current and active diagnoses,* an active medication list,* and an active medication allergy list*). Provide 10 percent of summary of care records for patient referrals or transitions of care either through the EHR or a properly governed health information exchange. Perform one or more successful exchanges of a summary of care with a provider using an EHR developed by a different technology vendor OR perform one or more successful tests with the CMS designated test EHR. |
| Be able to submit electronic data to immunization registries or immunization information systems† | Successful ongoing submission of electronic immunization data from the EHR to an immunization registry or immunization information system. |
| Use secure electronic messaging to communicate with patients on relevant health information | More than 5 percent of patients send a secure message through the EHR to the physician. |
Three other Stage 1 objectives – maintaining a patient problem list, maintaining a medication list, and maintaining an allergy list – have been folded into the separate core objective of providing a summary of care when patients are referred or transferred to another provider. That means that although you don't have to report those to CMS anymore, you still must maintain a patient's problem list, medication list, and allergy list for the other objective. It reduces some of the administrative burden of meaningful use, but it doesn't mean you'll do less work.
You will still have to provide these summaries for more than 50 percent of transitions and referrals, but there's a new requirement that you must send 10 percent of those summaries in electronic format. This will be more challenging, and you may want to see if there's a health information exchange in your area that would make connecting with other providers easier. You'll also want to ask your EHR vendor how they have complied with the Direct Project to make messaging more secure.
A core objective that has changed significantly involves the office visit summary, which details what happened during the visit and includes any next steps for the patient to follow. The objective still requires providing summaries to more than 50 percent of your patients, but you now must do it within one business day and not the three you had in Stage 1. This essentially means you will need to complete the summary before you're done seeing the patient. This will obviously affect your workflow if you typically finish your charting later or if you wait two days before completing the summaries so that you can include lab or other test results. There have been questions about whether the summary is part of the medical legal document and needs to be reproducible in the event of an audit. You likely won't need to reproduce the summary as the intent is to send or give it to the patient, but if an auditor demands proof that you sent the required percentage of summaries to patients, then you need to have some ability to track that, probably through the EHR. Stage 2 better defines the data elements that the summary must include (in fact, three different summaries are defined in Stage 2), so EHR vendors should be better able to help you create those.
Another big change involves patient electronic access. In Stage 1, you had an optional item to provide more than 10 percent of your patients with the ability to access their information online within four business days of it being updated and a required item to provide to more than 50 percent of patients, on request, an electronic copy of their health information within three business days. Stage 2 functionally replaces or eliminates these items in favor of a new core objective requiring that more than 50 percent of patients be able to view, download, or transmit to a third party their health information within four days of it being available. Also, at least 5 percent of patients during the reporting period must actually view, download, or transmit their health information to a third party. Note that the system must be certified to do all three, but the patient has to do just one to be counted in the 5 percent. It should be obvious that a patient portal is now necessary to achieve meaningful use.
The rules also are placing more emphasis on protecting your patients' health information. Although storing data in compliance with HIPAA was a Stage 1 requirement, the rules now also demand that you encrypt that data while it is stored on disk (also known as “at rest”). Why? Many of the major security breaches that we've seen in the last several years occurred when mobile devices were stolen out of a practice, home, or vehicle. You now must report such losses to the federal government and indicate the extent to which patient information may have been improperly disclosed. Once again, check with your EHR vendor, and if you need additional information on complying with HIPAA and the new Health Information Technology for Economic and Clinical Health Act of 2009, the American Academy of Family Physicians has a manual.
Brand new in Stage 2
A number of brand-new items may require some additional technology or expertise in your office. For example, your EHR now must provide access to radiographic imaging. You do not have to store the images locally but could connect to a hospital or imaging center that has a picture archiving and communications system to store digital results. This is a menu item, so it is optional, but if you are already sending images or orders for imaging to a particular hospital and can access that through your EHR, this is a good menu item to choose. Note that while the description of the imaging study may have already been accessible, that is not enough anymore. It has to be the actual picture of the X-ray, MRI, or CT scan rather than just the radiology report.
Another new menu item requires recording family history for a first-degree relative in structured data. This could be easy to complete if your system can display a family member's problem list in the family history section of the patient's record. Another menu item is having electronic progress notes for 30 percent of unique patients seen. These notes must be text searchable, meaning a term like “diabetes” will be highlighted in the note upon searching, similar to searching a webpage.
It should be noted that in states that lack such things as cancer or disease symptom registries (the subjects of the other menu items), physicians will have much less freedom in choosing menu items.
Stage 2 also requires, as a core item, that more than 5 percent of patients send a secure message to you through your EHR portal. This could be problematic as it requires action by the patient for you to achieve meaningful use. If patients aren't interested in sending you messages, how will you get 5 percent to do it? Time will tell how difficult this measure is for physicians to satisfy.
Continuing challenges
The meaningful use journey – and it will continue to be a journey as future stages of meaningful use come about – is about being able to adapt your practice, develop a clear vision of what you want your practice to be, establish the methods and the processes, and then put the structures in place so that you can achieve that vision. The challenges of meaningful use Stage 2 are substantial, from the significant increase in the number and difficulty of measures eligible professionals must satisfy to the implementation of patient portals and the need to persuade patients to use them. However, while we may question how the decisions of CMS and the Office of the National Coordinator for Health Information Technology will affect our practices, this continuing saga is ultimately about providing the best care possible to the patients who rely on us.
