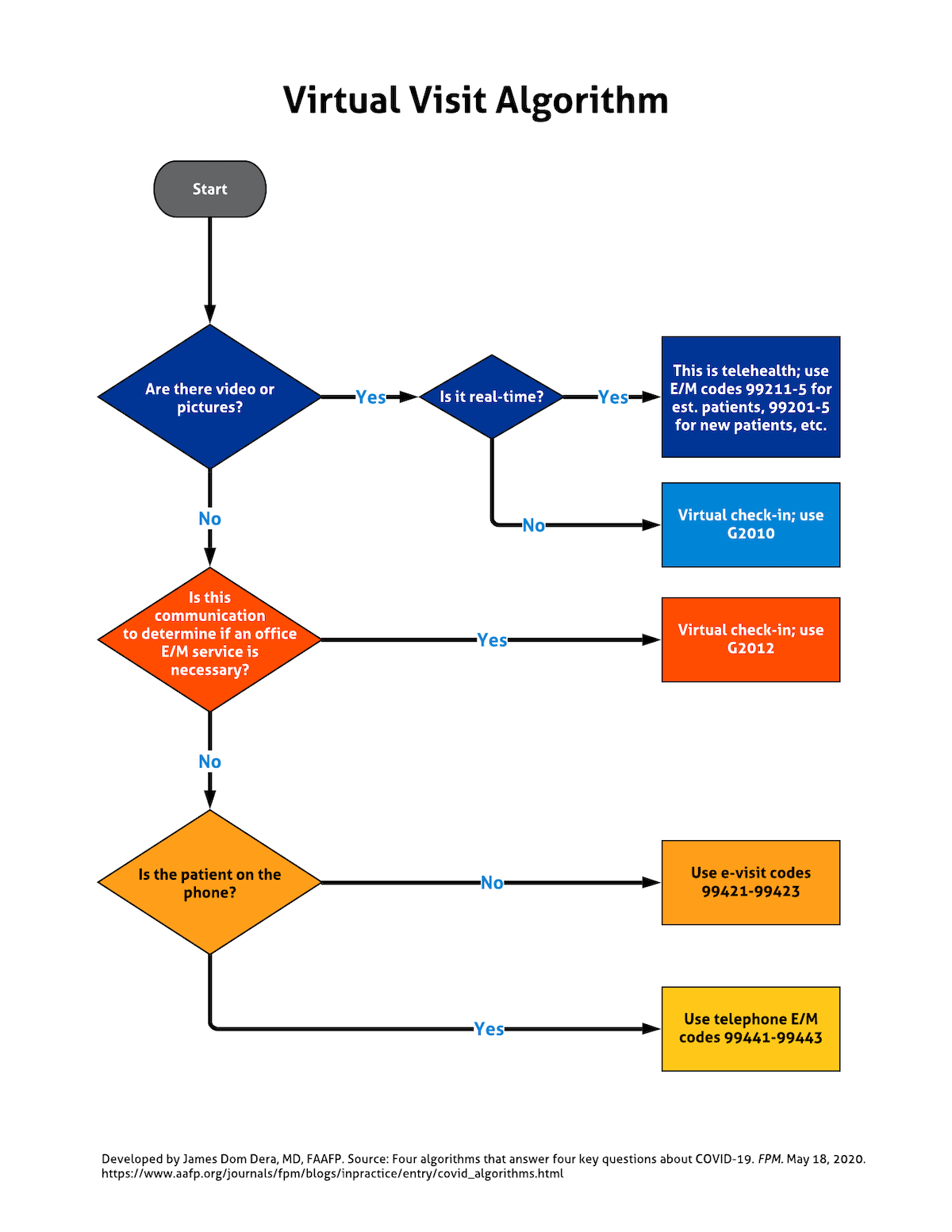
A virtual visit algorithm: how to differentiate and code telehealth visits, e-visits, and virtual check-ins
Virtual visits have quickly become vital in the primary care setting as a way to continue providing care while reducing exposure during the COVID-19 national public health emergency. The Centers for Medicare & Medicaid Services (CMS) has temporarily relaxed certain requirements for Medicare telehealth visits to make them more widely available, even through the use of basic tools such as Facetime, Skype, and Zoom. Some private payers are also expanding their coverage of virtual visits, but the American Academy of Family Physicians is calling on all payers to do the same.
There are four types of virtual visits:
- Telehealth visits (real-time audio and video),
- E-visits (online E/M visits),
- Virtual check-ins (assessments by telephone or other telecommunication device to determine whether an in-office encounter is needed for the patient’s concern),
- Telephone E/M visits (which are not covered by Medicare but may be covered by some private payers).
The following algorithm, developed by James Dom Dera, MD, FAAFP, provides a quick way for physicians to tell these services apart and to assign proper codes for reimbursement.
Note: On March 30, CMS announced another broad expansion of telehealth capabilities, including audio-only telephones. You can read more about it here. The list of specific codes covered can be found here. For more information on the other types of virtual visits, CMS has put together a toolkit for primary care practices.
Virtual visit algorithm
Get "Quick Tips" in your inbox
Sign up to receive FPM's free, weekly e-newsletter, "Quick Tips & Insights," featuring practical, peer-reviewed advice for improving practice, enhancing the patient experience, and developing a rewarding career.
Other Blogs
- Getting Paid from FPM journal
- AFP Community Blog
- AAFP Voices Blog
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. All comments are moderated and will be removed if they violate our Terms of Use.