
A more recent article on carpal tunnel syndrome is available.
Am Fam Physician. 2016;94(12):993-999
Patient information: See related handout on carpal tunnel syndrome.
Author disclosure: No relevant financial affiliations.
Carpal tunnel syndrome, the most common entrapment neuropathy of the upper extremity, is caused by compression of the median nerve as it travels through the carpal tunnel. Classically, patients with the condition experience pain and paresthesias in the distribution of the median nerve, which includes the palmar aspect of the thumb, index and middle fingers, and radial half of the ring finger. Additional clues include positive physical examination findings, such as the flick sign, Phalen maneuver, and median nerve compression test. Although patients with typical symptoms and signs of carpal tunnel syndrome do not need additional testing, ultrasonography and electrodiagnostic studies are useful to confirm the diagnosis in atypical cases and rule out other causes. If surgical decompression is planned, electrodiagnostic studies should be obtained to determine severity and surgical prognosis. Conservative treatment may be offered initially to patients with mild to moderate carpal tunnel syndrome. Options include splinting, corticosteroids, physical therapy, therapeutic ultrasound, and yoga. Nonsteroidal anti-inflammatory drugs, diuretics, and vitamin B6 are not effective therapies. Local corticosteroid injection can provide relief for more than one month and delay the need for surgery at one year. Patients with severe carpal tunnel syndrome or whose symptoms have not improved after four to six months of conservative therapy should be offered surgical decompression. Endoscopic and open techniques are equally effective, but patients return to work an average of one week earlier with endoscopic repair.
Carpal tunnel syndrome (CTS) is often a debilitating disorder that is commonly encountered in primary care. It is the most common entrapment neuropathy of the upper extremity, affecting approximately 3% of the general adult population.1 Women are three times more likely to have CTS than men, and the prevalence and severity increase with age. Work-related activities that require a high degree of repetition and force or use of hand-operated vibratory tools significantly increase the risk of CTS.2 A large prospective cohort study found that forceful hand exertion was the most important factor in the development of CTS in workers.3 Additional risk factors include family history and a personal history of diabetes mellitus, obesity, hypothyroidism, pregnancy, and rheumatoid arthritis.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Ultrasound measurement of a cross-sectional area of the median nerve by an experienced clinician may be used as a diagnostic test for carpal tunnel syndrome. | C | 14, 15 |
| Local corticosteroid injection is effective for more than one month in patients with mild to moderate carpal tunnel syndrome and delays the need for surgery at one year. | A | 20–24 |
| Splinting, therapeutic ultrasound, carpal bone mobilization, and nerve glide exercises are effective short-term treatments for carpal tunnel syndrome. | B | 25–27 |
| Endoscopic and open carpal tunnel release are equally effective, long-lasting treatments for carpal tunnel syndrome. | A | 30 |
The carpal tunnel is bordered superiorly by the transverse carpal ligament and inferiorly by the carpal bones, through which the median nerve and nine flexor tendons of the forearm pass. Increased pressure in the carpal tunnel leads to compression and damage of the median nerve.4
Symptoms
The hallmarks of CTS are pain and paresthesias in the distribution of the median nerve, which includes the palmar aspect of the thumb, index and middle fingers, and radial half of the ring finger (Figure 15). Symptoms can vary widely and occasionally localize to the wrist or the entire hand, or radiate to the forearm or rarely the shoulder. Patients often awaken with symptoms and shake out their hand to provide relief. This is known as the flick sign, and is 93% sensitive and 96% specific for CTS.6 Other provoking factors include tasks that require repetitive wrist flexion or hand elevation, such as driving or holding a telephone for extended periods.

Because sensory fibers are more susceptible to compression than motor fibers, paresthesias and pain usually predominate early in the course of CTS. In more severe cases, motor fibers are affected, leading to weakness of thumb abduction and opposition. Patients may describe difficulty holding objects, opening jars, or buttoning a shirt. Disappearance of pain is a late finding that implies permanent sensory loss.
Physical Examination
A complete examination of the entire upper extremity, including neck, shoulder, elbow, and wrist, should be conducted to exclude other causes (Table 15). Most patients with early, mild to moderate CTS will not have physical examination findings. However, initial inspection of the hand and wrist can provide clues to precipitating factors, such as signs of injury or arthritic changes. A square-shaped wrist (increased depth-to-width ratio) has an odds ratio of 4.56 (95% confidence interval, 2.97 to 6.99) for CTS, likely related to obesity.7

| Condition | Characteristics |
|---|---|
| Carpometacarpal arthritis of the thumb | Painful thumb motion, positive grind test, radiographic findings |
| Cervical radiculopathy (C6) | Neck pain, numbness of the thumb and index finger only, positive Spurling test |
| de Quervain tendinopathy | Tenderness at the distal radial styloid |
| Peripheral neuropathy | History of diabetes mellitus; bilateral, lower extremity involvement |
| Pronator syndrome (median nerve compression at the elbow) | Forearm pain; sensory loss over the thenar eminence; weakness with thumb flexion, wrist extension, and forearm pronation |
| Raynaud syndrome | Symptoms related to cold exposure, typical color changes |
| Ulnar compressive neuropathy | Paresthesias of the ring and little fingers, positive Tinel sign and compression tests at the elbow or wrist (Guyon canal) |
| Vibration white finger | Use of vibratory hand power tools, symptoms of Raynaud phenomenon |
| Wrist arthritis | Painful wrist motion, radiographic findings |
In more severe disease, permanent sensory and motor deficits occur. Patients may have decreased sensation to pain (hypalgesia) on the palmar aspect of the index finger compared with the ipsilateral little finger on the affected hand. Lack of two-point discrimination manifests as the inability to distinguish between points less than 6 mm apart.8,9 Sensation over the thenar eminence should be normal in patients with CTS because it is supplied by the palmar cutaneous branch of the median nerve, which branches off proximal to the carpal tunnel. Therefore, decreased sensation over the thenar eminence indicates a median nerve lesion proximal to the carpal tunnel. Weakness of thumb abduction and opposition and atrophy of the thenar eminence may occur in advanced CTS.
The diagnostic accuracy of provocative maneuvers for CTS varies widely (Table 2).5,6,8,9 However, these tests are simple to perform, and a combination of positive findings increases the likelihood of CTS.9 The hand elevation test has similar sensitivity and specificity as the Phalen maneuver and the Tinel sign.10 To perform the hand elevation test, the patient raises his or her hands above the head for one minute; the onset of symptoms is a positive result. One systematic review found that a classic or probable pattern on a hand symptom diagram (Figure 211) has a higher diagnostic accuracy than any single maneuver.8

| Finding | Sensitivity (%) | Specificity (%) | Technique |
|---|---|---|---|
| Flick sign | 93 | 96 | History of awakening with symptoms and shaking the hand to provide relief |
| Positive findings on both the median nerve compression test and the Phalen maneuver | 80 | 92 | See individual maneuvers |
| Classic or probable pattern on hand symptom diagram | 64 to 75 | 73 | See Figure 2 |
| Nighttime or morning symptoms | 70 | 43 | — |
| Positive findings on the Phalen maneuver | 57 to 68 | 58 to 73 | Flex the patient's wrist 90 degrees with the elbow in full extension; pain or paresthesias in the fingers innervated by the median nerve within 60 seconds are a positive result |
| Thumb abduction weakness | 29 to 65 | 65 to 80 | Ask the patient to raise the thumb perpendicular to the palm, then apply downward pressure on the distal phalanx while the patient resists |
| Median nerve compression test | 64 | 83 | Apply direct pressure over the transverse carpal ligament; sensory symptoms within 30 seconds are a positive result |
| Square-shaped wrist | 53 | 80 | Increased depth-to-width ratio |
| Tinel sign | 36 to 50 | 77 | Repeatedly tap the volar surface of the patient's wrist over the transverse carpal ligament; pain or paresthesias in the fingers innervated by the median nerve are a positive result |
| Hypalgesia | 39 | 88 | Decreased sensation to pain on the palmar aspect of the index finger compared with the ipsilateral little finger on the affected hand |
| Thenar atrophy | 12 to 16 | 90 to 94 | — |

Adjunctive Tests
The diagnosis of CTS is clinical in a patient with characteristic symptoms and physical examination findings. However, electrodiagnostic studies aid in confirming the diagnosis in atypical cases, determining severity, and planning for surgery. Evidence suggests that ultrasonography may also be useful in diagnosing CTS.
ELECTRODIAGNOSTIC STUDIES
Electrodiagnostic studies include nerve conduction studies and electromyography. Nerve conduction studies confirm CTS by detecting impaired median nerve conduction across the carpal tunnel, with normal conduction elsewhere. Electromyography assesses pathologic changes in the muscles innervated by the median nerve, typically the abductor pollicis brevis muscle.
Electrodiagnostic studies can exclude other conditions, such as polyneuropathy and radiculopathy, and gauge the severity of CTS. Electrodiagnostic studies have a sensitivity of 56% to 85% and specificity of 94% to 99% for CTS.12 Results may be normal in up to one-third of patients with mild CTS.13 Therefore, these studies should be reserved for confirming CTS in atypical cases and excluding other causes. Electrodiagnostic studies should be obtained before surgery to confirm the diagnosis and estimate prognosis because patients with more severe CTS are less likely to have complete recovery after surgery. Repeat nerve conduction studies showing improvement can help reassure these patients.
ULTRASONOGRAPHY
The cross-sectional area of the median nerve is closely correlated with CTS symptoms and severity. A meta-analysis found that a cross-sectional area of 9 mm2 or more is 87.3% sensitive and 83.3% specific for CTS.14 Experience in performing ultrasonography for the diagnosis of CTS correlates with greater inter-rater reliability when measuring the cross-sectional area.15 Advantages of ultrasonography include lower cost; noninvasiveness; patient comfort; and evaluation of etiologies such as tenosynovitis, mass lesions, and tendinopathies. However, ultrasonography relies on local expertise and cannot rule out etiologies such as polyneuropathies or gauge severity of CTS.
OTHER TESTS
Plain radiography may be useful if structural abnormalities, such as bone or joint disease, are suspected. Magnetic resonance imaging is not generally indicated. Laboratory testing for comorbidities, such as diabetes or hypothyroidism, may be considered if there are other signs suggesting disease.
Treatment
Management of CTS is based on disease severity. In mild to moderate cases, a trial of conservative treatment is recommended. Patients with severe CTS or nerve damage on electrodiagnostic studies should be offered surgical decompression. Conservative treatment modalities include splinting, corticosteroids, physical therapy, therapeutic ultrasound, and yoga. Conservative therapy usually improves symptoms in two to six weeks and reaches maximal benefit at three months.16 If there is no improvement after six weeks, another approach should be considered.
SPLINTING
Splinting is a first-line treatment for mild to moderate CTS because of its simplicity, low cost, and tolerability. A 2012 Cochrane review found nocturnal wrist splinting to be more effective than placebo, but found insufficient evidence to recommend one splint design over another or compare effectiveness of splinting to other conservative interventions.17 However, one study showed that patients wearing a neutral wrist splint were twice as likely to report symptom relief compared with patients wearing an extension splint.18 Splinting is advisable in reversible cases of CTS, such as in pregnancy, and can be combined with other treatment modalities.
LOCAL CORTICOSTEROID INJECTION
Increasing evidence supports local carpal tunnel corticosteroid injection as an effective treatment for CTS. A 2007 Cochrane review found symptomatic benefit for up to one month; however, more recent evidence shows improvement lasting 10 weeks to more than one year.19 Corticosteroid injections can also delay the need for surgery. A double-blinded randomized controlled trial of 111 patients treated with a single injection of 80-mg methylprednisolone, 40-mg methylprednisolone, or saline found greater improvement at 10 weeks with the methylprednisolone injections compared with placebo, and patients in the 80-mg injection group were less likely to have surgery at 12 months.20 Notably, most patients underwent surgery by one year. Additional randomized controlled trials that included repeat injections showed symptomatic improvement beyond 12 months and similar findings of decreased need for surgery at one year.21–23
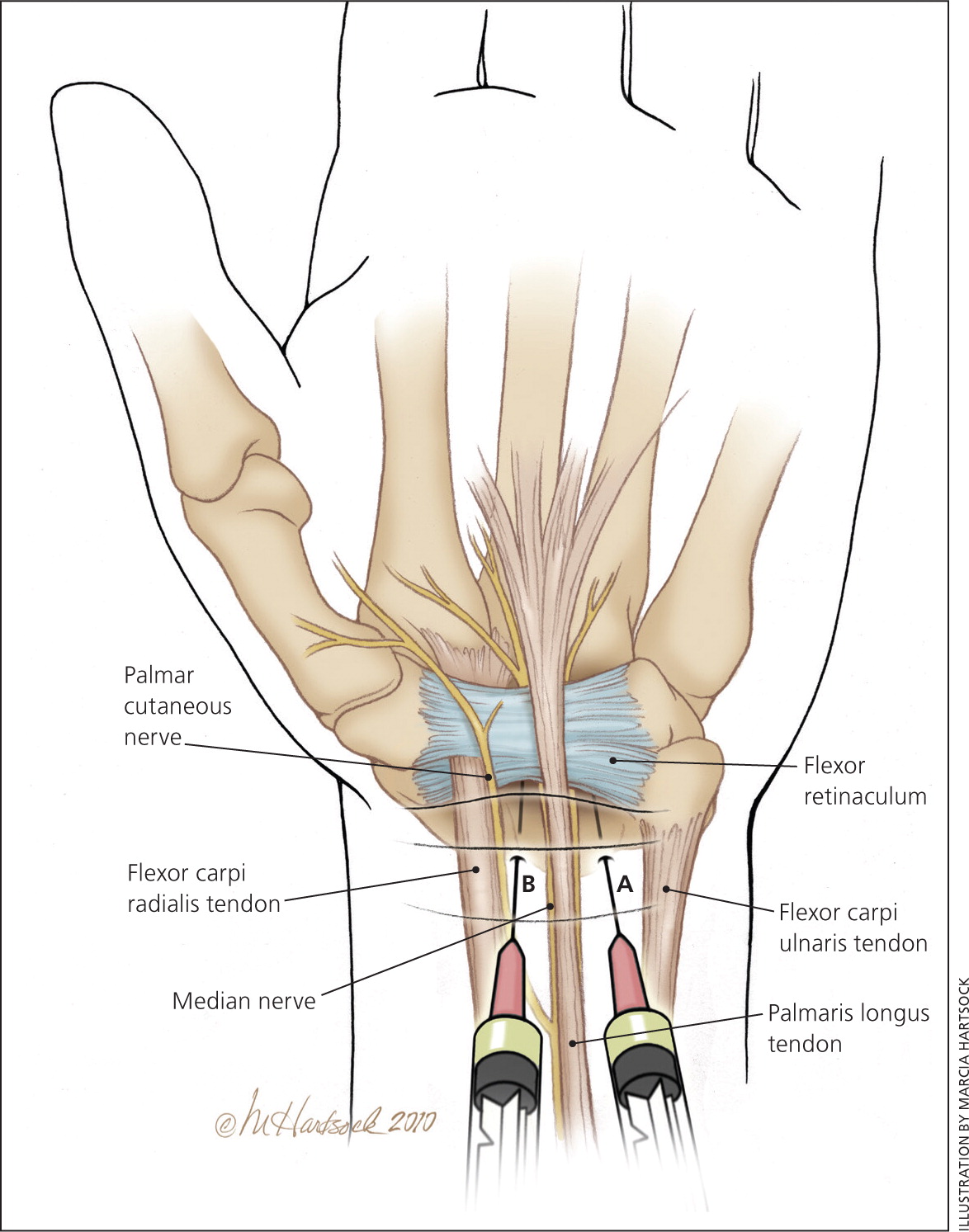
Evidence does not support one injection technique over another or a particular steroid formulation. However, ultrasound-guided injection may be more effective than blind injection24 and allows for direct visualization to ensure accurate and safe needle placement (Table 35 and Figure 35). Although injection is generally safe, there is risk of median nerve injury and tendon rupture. A repeat injection in the same wrist may be offered after six months. If symptoms recur after two injections, another treatment or surgery should be considered.

| Patient should be in a seated position with the forearm supinated and wrist slightly extended |
| Identify the injection site medial to the palmaris longus tendon or midway between the palmaris longus and the flexor carpi ulnaris tendons, and 1 cm proximal to the most distal wrist crease (Figure 3) |
| Cleanse the area with chlorhexidine or povidone-iodine solution |
| Using a 25-gauge needle and sterile technique, inject 1 mL of 10-mg-per-mL triamcinolone acetonide and 1 mL of lidocaine 1% without epinephrine |
| Direct the needle at a 45-degree angle distally until the tip of the needle lies under the midpoint of the flexor retinaculum |
| Inject slowly; if the patient experiences shock-like pain or paresthesias, stop the injection and redirect the needle medially |
ORAL MEDICATION
Oral prednisone at a dosage of 20 mg daily for 10 to 14 days improves symptoms and function compared with placebo; the improvement lasts up to eight weeks.25 Oral corticosteroids are less effective than corticosteroid injection. Nonsteroidal anti-inflammatory drugs, diuretics, and vitamin B6 are not effective therapies.25
PHYSICAL THERAPY
There is limited evidence that physical therapy techniques such as carpal bone mobilization, therapeutic ultrasound, and nerve glide exercises are effective CTS treatments.26,27 Nerve glide exercises are simple hand and finger movements that theoretically restore normal movement of the median nerve, which can become “tethered” from nerve compression. A video demonstrating these exercises is available at https://www.youtube.com/watch?v=B5goXA9MqCA. Although the evidence for these techniques is limited, they are easy to learn; can be done at home; and can be combined with other treatments, such as splinting.
Therapeutic ultrasound and carpal bone mobilization require an experienced therapist, have limited evidence of effectiveness, and require multiple sessions (typically five days per week for two to four weeks with therapeutic ultrasound).27
One randomized trial of 42 patients with CTS found that yoga improved pain at eight weeks vs. wearing a wrist splint.28
SURGICAL DECOMPRESSION
Carpal tunnel decompression provides a lasting, good outcome in 70% to 90% of cases.29 Surgery is the treatment of choice for patients with severe median nerve damage as characterized by permanent sensory or motor loss, or ongoing axonal loss or denervation on electrodiagnostic studies.29 Endoscopic and open techniques are equally effective; however, patients return to work on average eight days earlier with endoscopic repair than with open repair.30 The most common complications are a painful scar and pillar pain (pain adjacent to the site of ligament release). Most patients note significant improvement in one week and are able to return to normal activities in two weeks. However, some patients (especially those with severe CTS) take up to one year to recover fully. Postoperative splinting does not improve outcomes and may increase stiffness and adhesion formation.31
This review updates previous articles on this topic by LeBlanc and Cestia5 and by Viera.32
Data Sources: A PubMed search was completed in Clinical Queries using the key terms carpal tunnel, carpal tunnel syndrome, treatment, diagnosis, ultrasound, and corticosteroid injection. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality evidence reports, Bandolier, the Cochrane database, Database of Abstracts of Reviews of Effects, Essential Evidence Plus, the National Guideline Clearinghouse, choosingwisely.org, and UpToDate. Search dates: September to October 2015, and August 2016.
