Am Fam Physician. 2019;100(12):745-750
Patient information: See related handout on amblyopia.
Author disclosure: No relevant financial affiliations.
Amblyopia is the leading cause of monocular vision loss in children. Early recognition and treatment are important to prevent vision loss. The U.S. Preventive Services Task Force recommends vision screening for all children at least once between three and five years of age to detect the presence of amblyopia or its risk factors. The American Association for Pediatric Ophthalmology and Strabismus and the American Academy of Pediatrics recommend routine, age-appropriate red reflex testing, examination for signs of strabismus, and vision chart testing. Photoscreening may be a useful adjunct to traditional vision screening, but there is limited evidence that it improves visual outcomes. Treatments for amblyopia include patching, atropine eye drops, and optical penalization of the nonamblyopic eye. In children with moderate amblyopia, patching for two hours per day is as effective as six hours, and daily atropine is as effective as daily patching. Children younger than seven years receive the most benefit from treatment, but older children may still benefit. Amblyopia recurs in 25% of children, so continued surveillance is important.
Amblyopia is a decrease in best-corrected visual acuity resulting from abnormal vision development in infancy and early childhood.1,2 The term is derived from a Greek word meaning dullness of vision; it is also called “lazy eye.” Amblyopia is the leading cause of childhood monocular vision loss, with an estimated prevalence of 1% to 6%,3 and it is responsible for permanent vision loss in 2.9% of adults.4 Although amblyopia may be bilateral, it is usually unilateral. The ocular structures are usually normal on physical examination. Associated conditions include unequal refractive error and strabismus (misalignment of the eyes).1 Amblyopia may result from conditions such as cataracts and eyelid ptosis, which disrupt the visual axis and impede a clear image reaching the retina. Children with high refractive error may develop bilateral amblyopia. Once amblyopia is established, corrective lenses usually will not sharpen vision. Early recognition and referral during infancy and childhood are important to prevent vision loss.
Etiology
Amblyopia is thought to develop during a critical time in infancy and early childhood when visual development depends on the eyes and the brain's visual cortex working together.5 Inadequate stimulation of the visual pathways leads to disuse of the visual cortex and resultant amblyopia.
| Type | Description |
|---|---|
| Strabismic | Misalignment of eyes (strabismus) results in visual cortex suppression of the visual input of the deviating eye |
| Anisometropic | Difference of visual acuity (refractive error) between eyes leads to visual blurring of one eye and visual cortex suppression of the visual input of the blurred eye |
| Combined strabismic and anisometropic | Eye misalignment and refractive error leads to visual cortex suppression of the chronically blurred image |
| Ametropic | Bilateral, symmetric high refractive error resulting in blurred vision in both eyes and inadequate development of the visual cortex |
| Deprivation | Obstruction of the visual axis results in suppression of the visual cortex |
Strabismic amblyopia occurs when the eyes are misaligned. The visual cortex suppresses visual input from the deviating eye because the brain cannot fuse the different images from each eye. This type of amblyopia results in loss of binocular vision and thus, depth perception (stereopsis).
Anisometropic amblyopia (also called refractive amblyopia) occurs when there is a difference in visual acuity between the eyes, leading to the blurring of vision in one eye. The eye with the higher refractive error (more blur) requires greater effort to focus and form a clear image; therefore, it tends to remain unfocused. Chronic blur leads to amblyopia as the visual cortex ignores the chronically blurred visual input. Amblyopia is more commonly associated with anisometropia due to farsightedness or astigmatism rather than nearsightedness.
Ametropic amblyopia occurs in children with bilateral, symmetric high refractive error; the eyes cannot accommodate, and the blurred vision results in inadequate development of the visual cortex. Deprivation amblyopia results from obstruction of the visual axis by unusual conditions such as congenital ptosis or cataracts.
Screening and Diagnosis
Early diagnosis of amblyopia is key to optimize the likelihood of successful treatment.7 Children younger than seven years are more likely than older children to have a good response to treatment.8 Recommendations from the U.S. Preventive Services Task Force (USPSTF), supported by the American Academy of Family Physicians, suggest screening all children three to five years of age for amblyopia or its risk factors at least once.9 The USPSTF found inadequate evidence that screening in children younger than three years leads to improved vision outcomes. The American Academy of Pediatrics and the American Association for Pediatric Ophthalmology and Strabismus recommend starting screening in newborns.10 Children with an increased risk of amblyopia should be referred for an ophthalmologic examination as soon as a risk factor is identified.11 These include ptosis, gestational age less than 30 weeks, birth weight less than 1,500 g (3 lb, 5 oz), cerebral palsy, syndromes with ocular involvement (e.g., Down syndrome), and a family history of amblyopia or strabismus.
History
Detection of amblyopia should begin with a careful medical and family history.11 A family history of congenital cataracts, glaucoma, or amblyopia should prompt referral to an ophthalmologist for a comprehensive examination. Likewise, if either parent has strabismus, the child has a fourfold greater risk and should undergo comprehensive examination.12
Parents should be asked about clinical clues that may suggest amblyopia in their children, including a wandering eye, squinting of one eye, torticollis (head tilting), nystagmus, or strabismus. Torticollis may be a sign that the child is trying to better align the eyes. Children with nystagmus may turn their head to find a visual zone that decreases the eye movement. Squinting of one eye may indicate eye wandering or exotropia.
Examination
Physical examination should include inspection for ptosis, cataracts, and corneal opacities; pupillary examination; assessment of ocular motility and alignment (corneal light reflection, binocular red reflex test, and cover/uncover tests); and vision testing. Methods for performing these examinations are discussed in a previous American Family Physician article.13
The American Association for Pediatric Ophthalmology and Strabismus age-based examination and vision screening guidelines are outlined in Table 2.14 External inspection of the eyes and lids, assessment of ocular motility, and red reflex testing are valuable for detecting risk factors for amblyopia in infants and children, such as a cataracts, refractive error, and retinal pathology. The binocular red reflex (Bruckner) test is performed in a darkened room. The examiner shines an ophthalmoscope light toward the eyes from approximately 18 to 30 inches away and compares the reflex in both eyes for asymmetry in position, color, or intensity15 (Figure 113).
| Age | Tests | Referral criteria |
|---|---|---|
| Newborn to 12 months | External inspection of the eyes and lids Ocular history Ocular motility assessment Pupil examination Red reflex examination Vision assessment | Infants who do not track well after 3 months of age, or who have an abnormal red reflex or history of retinoblastoma in a parent or sibling |
| 12 months to 3 years | External inspection of the eyes and lids Objective screening device (photoscreening) Ocular history Ocular motility assessment Ophthalmoscopy Pupil examination Red reflex examination Visual acuity testing | Infants with strabismus or chronic tearing or discharge; children who have positive photoscreening results |
| 3 to 5 years | External inspection of the eyes and lids Ocular history Ocular motility assessment Ophthalmoscopy Pupil examination Red reflex examination Vision assessment Visual acuity testing (preferred) or photoscreening | Children who cannot read at least 20/40 with either eye; must be able to identify most of the optotypes on the 20/40 line |
| 5 years and older | External inspection of the eyes and lids Ocular history Ocular motility assessment Ophthalmoscopy Pupil examination Red reflex examination Vision assessment Visual acuity testing | Children who cannot read at least 20/32 with either eye; must be able to identify most of the optotypes on the 20/32 line; children not reading at grade level |
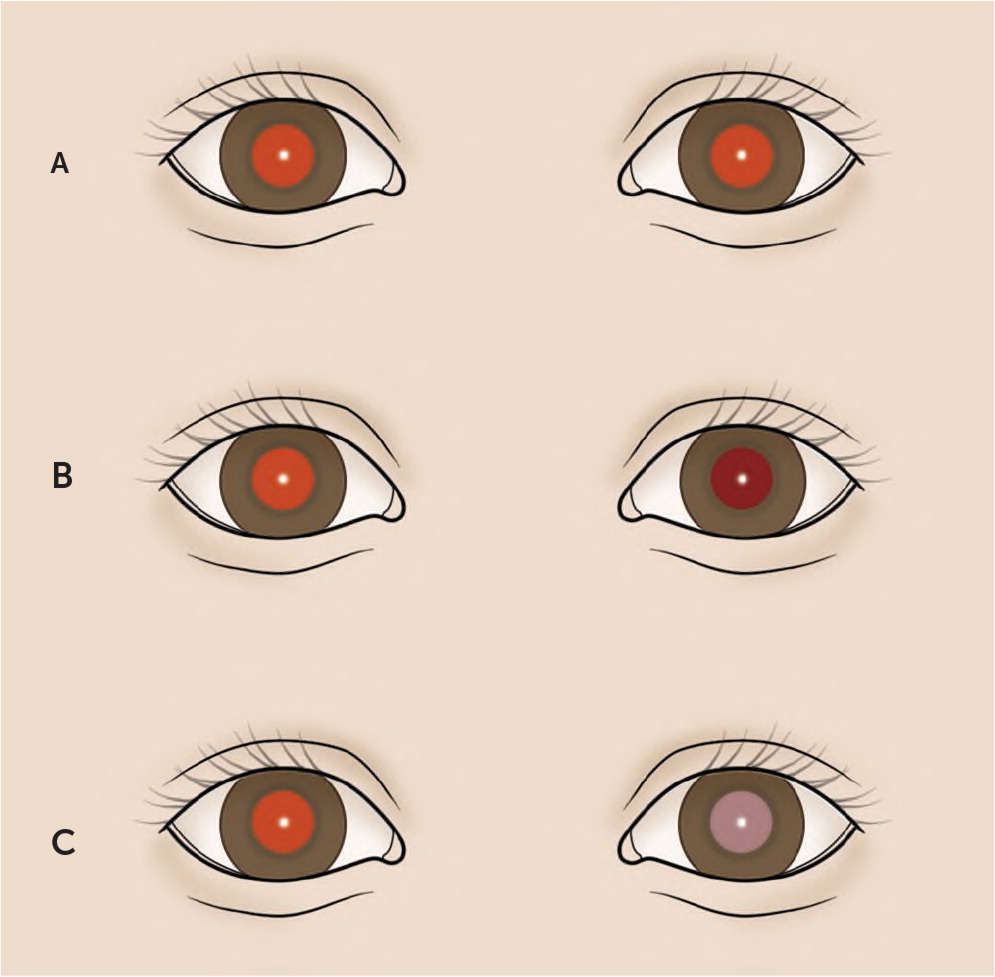
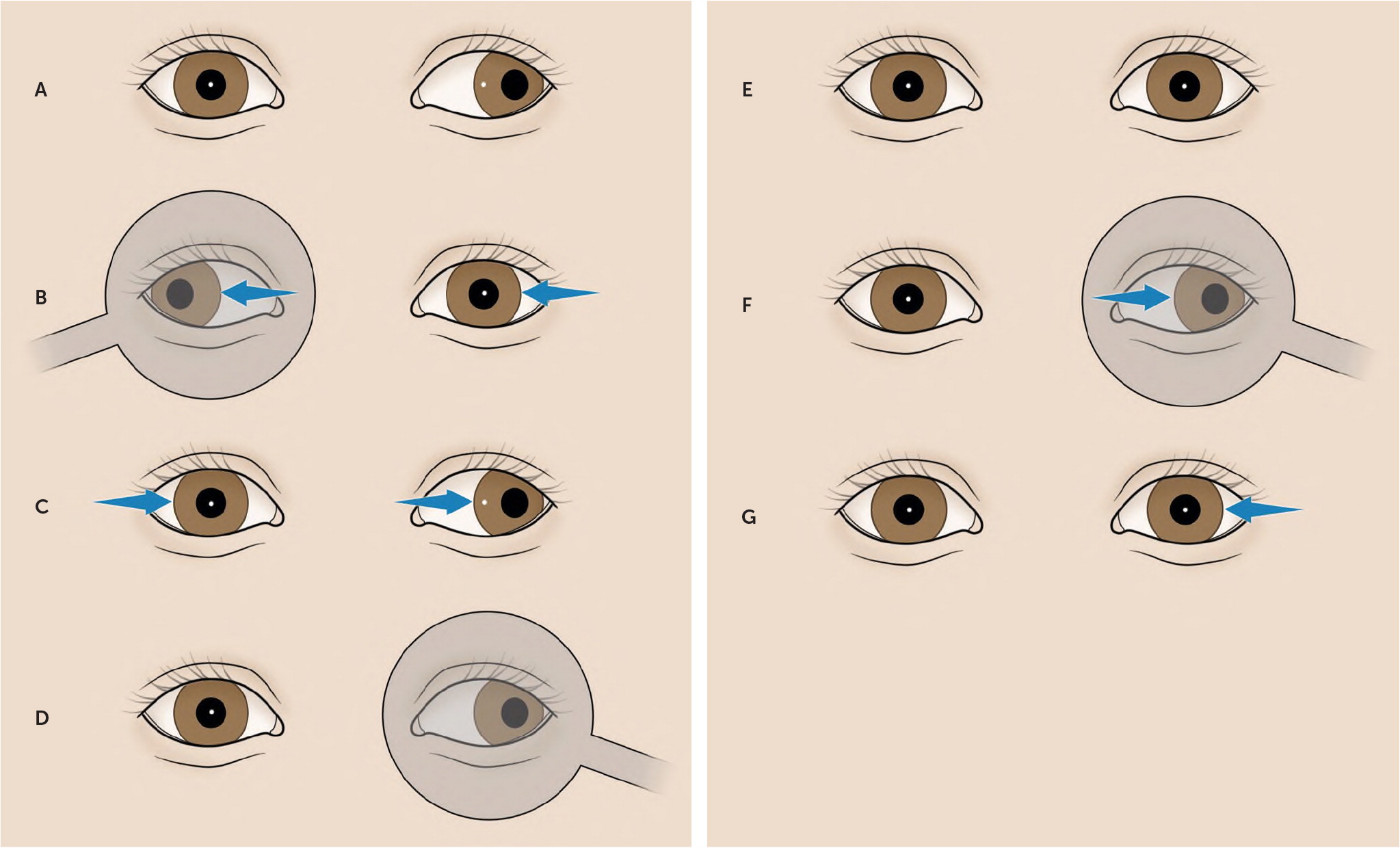
In infants and children up to three years of age, visual assessment can be accomplished using fixation testing or the cover-uncover test (Figure 2).13 A toy is used as a fixation target to hold the child's attention, then one eye is occluded; the child should follow the moving toy with the nonoccluded eye. A fixation preference for one eye can indicate amblyopia. A child with strabismus will show fixation preference in the nondeviating eye. Amblyopia should be suspected if the child is uncooperative when occluding one eye.
Vision testing should be performed in children three years and older, using standard eye charts (with pictures, a single letter [e.g., the tumbling E], or lines of letters) at a distance of 10 or 20 ft (3 to 6 m).13 An occluder may be used to cover the eye during testing; however, an adhesive patch is preferred because children may peek around the occluder, and amblyopia can be missed. Any child three to five years of age with visual acuity less than 20/40 in either eye, or any child five years or older with visual acuity less than 20/32 in either eye or with a two-line difference between eyes should be referred for a comprehensive ophthalmic examination.14
Photoscreening
Photoscreening is a useful adjunct to detect amblyopia risk in younger children, those who are uncooperative with chart-based vision testing, or those who are nonverbal. In photoscreening, the red reflex of both eyes is taken simultaneously with digital or flash photography and evaluated for signs of uncorrected refractive error, ocular opacities, or misalignment. The images are analyzed by software or human interpreters, and if an abnormality is detected, referral to an ophthalmologist is recommended.16–18 Previously, a physician would have had to buy a photoscreener to perform this screening, which was usually cost prohibitive. However, there is now a photoscreening app for mobile devices that is affordable and easily accessible.19 A photograph of the eyes is taken with the phone, and the app analyzes it for amblyopia risk factors. It has a sensitivity of 65% and a specificity of 83%.19
Treatment
Treatment of amblyopia relies on addressing the source of the visual deprivation (e.g., removal of cataracts, strabismus surgery in selected cases) and correcting the refractive error, then on promoting use of the amblyopic eye by hindering the visual input from the better eye.11 Methods to encourage the use of the amblyotic eye include patching, pharmacologic therapy, and optical penalization of the better eye.20 Regardless of treatment, correction of refractive errors with glasses should be addressed first.
A patch should be affixed over the nonamblyotic eye. It should not be applied to eyeglasses because the child could easily look around it. In one multicenter randomized controlled trial of children with moderate amblyopia (visual acuity 20/40 to 20/80), patching for two hours per day was as effective as six hours for improving visual acuity.21 In another multicenter randomized controlled trial, the improvement with six hours of daily patching was equal to that from full-time patching (all but one hour per day) in children with severe amblyopia (20/100 to 20/400).22 In children with strabismic amblyopia, vision correction with glasses plus patching the amblyotic eye was more effective than glasses alone.12 Atropine 1% ophthalmic drops block parasympathetic innervation to the ciliary muscle and pupil, causing temporary paralysis of accommodation (cycloplegia) and dilation of the pupil. This results in blurring in the nonamblyopic eye and inability to focus at near distance, thus stimulating the preferential near fixation of the amblyopic eye and subsequent visual improvement.
Atropine given on two consecutive days per week is as effective as daily use in children with moderate amblyopia.23 Daily atropine is as effective as daily patching in those with moderate amblyopia.24,25 Optical penalization with a Bangerter filter, a translucent filter applied to the eyeglass lens over the nonamblyotic eye, may be used in children with moderate amblyopia.26 The filter is as effective as two hours of patching per day; compliance with wearing glasses should be monitored to maximize effectiveness.
Treatment regimens should be individualized based on age, visual acuity, previous treatments, adherence, and psychosocial factors.1,11 Careful surveillance is necessary for children successfully treated for amblyopia because 25% will have recurrence within one year.27 Treatment of children older than seven years is less effective than in younger children. However, there are likely many factors that contribute to the variability in treatment response; thus, older children still may benefit from treatment.8,28
This article updates previous articles on this topic by Bradfield1 and by Doshi and Rodriguez.2
Data Sources: We searched the Cochrane database, PubMed Clinical Queries, the Agency for Healthcare Research and Quality evidence reports, the National Guideline Clearinghouse, and Essential Evidence Plus using the keywords amblyopia, vision screening, and strabismus. Last search date: September 3, 2019.