
Am Fam Physician. 2022;105(5):469-478
Author disclosure: No relevant financial relationships.
Constipation in children is usually functional constipation without an organic cause. Organic causes of constipation in children, which include Hirschsprung disease, cystic fibrosis, and spinal cord abnormalities, commonly present with red flag signs and symptoms. A history and physical examination can diagnose functional constipation using the Rome IV diagnostic criteria. The first goal of managing constipation is to treat fecal impaction, and then maintenance therapy is used to prevent a recurrence. Polyethylene glycol is the first-line treatment for constipation. Second-line options include lactulose and enemas. Increasing dietary fiber and fluid intake above usual daily recommendations and adding probiotics provide no additional benefits for treating constipation. Frequent follow-up visits and referrals to a psychologist can assist in reaching some treatment goals. Clinicians should educate caregivers about the chronic course of functional constipation, frequent relapses, and the potential for prolonged therapy. Clinicians should acknowledge caregivers' specific challenges and the negative effects of constipation on the child's quality of life. Referral to a pediatric gastroenterologist is recommended when there is a concern for organic causes or constipation persists despite adequate therapy.
Constipation in children and adolescents is defined as passing delayed or infrequent hard stools with pain and excessive straining.1,2 The prevalence of constipation in children and adolescents is estimated to be as high as 30% worldwide.3 Constipation in children accounts for 3% of primary care physician visits and up to 25% of referrals to pediatric gastroenterologists.1 Children with constipation incur three times the health care costs of children without constipation,4 and chronic constipation can have a negative effect on the child's quality of life.5
Normal Defecation Patterns
The number of daily bowel movements decreases as a child ages, averaging four stools per day for infants, two stools per day by two years of age, and one stool per day after four years of age.1 Infants who are exclusively breastfed are exceptions to these patterns because there may normally be several days between bowel movements.6
Classification
Functional constipation, for which there is no organic cause, is the most common type of constipation in children and adolescents, accounting for 95% of cases.7 Only 5% of constipation cases in children and adolescents can be attributed to an underlying etiology such as Hirschsprung disease, cystic fibrosis, Down syndrome, anorectal malformations, neuromuscular disorders, spinal cord abnormalities, or celiac disease. Certain medications such as opiates, antacids, or anticholinergics can also cause constipation.7
Functional constipation is classified as a functional gastrointestinal disorder that cannot be explained by structural or biochemical findings.8 Other functional gastrointestinal disorders in children that may be associated with constipation are infant dyschezia and nonretentive fecal incontinence. Infant dyschezia occurs in infants younger than nine months who have constipation-like symptoms, including straining, crying, and transient reddening of the face, but frequently pass soft stools. These symptoms resolve on their own and are usually due to a discoordination of anal sphincter muscles.2,7 Nonretentive fecal incontinence differs from functional constipation by the presence of fecal incontinence without stool impaction, a normal number of stools, and normal colonic transit time in children four to 18 years of age. Significant psychosocial problems or neurologic lesions may be found in children with nonretentive fecal incontinence.2
Encopresis is not mentioned in the Rome IV diagnostic criteria for constipation; however, it is included in the Diagnostic and Statistical Manual of Mental Disorders, 5th ed., as an elimination disorder that can occur with or without fecal retention. Encopresis is the repeated passage of feces in inappropriate places (i.e., clothing or floor), with one or more events occurring each month for three or more months, and the key feature is soiling.2,6–10
Etiology and Pathophysiology
Constipation leads to painful bowel movements, which can cause the child to withhold stool. Withholding stool increases colonic water absorption, making the stool firmer and more difficult to pass. The child contracts the anal sphincter or gluteal muscles by stiffening the body to avoid another painful bowel movement. The child may hide in a corner, rock back and forth, or fidget with each urge to defecate. Parents often confuse these withholding behaviors as straining to defecate.12 Over time, fecal retention stretches the rectum, which decreases the urge to defecate. The accumulation of stool in the rectum causes a decrease in gastric emptying, resulting in abdominal distention, abdominal pain, nausea, and loss of appetite.2 Although children may have painful or traumatic defecation experiences, resulting in stool withholding, adolescents suppress the urge to defecate as a learned behavior.13
Clinical Diagnosis
| ≥ 2 of the following, occurring at least once per week for at least 1 month: |
| ≤ 2 defecations in the toilet per week in a child ≥ 4 years of age |
| ≥ 1 episode of fecal incontinence per week |
| History of retentive posturing or excessive volitional stool retention |
| History of hard or painful bowel movements |
| Presence of large fecal mass in rectum |
| Large diameter stools that obstruct toilet |
| After appropriate medical evaluation, the symptoms cannot be explained by another medical condition |
A comprehensive history and physical examination (Table 2 and Table 32,12,14) are usually sufficient to diagnose functional constipation and should exclude red flag signs and symptoms suggesting organic causes6,10 (Table 49,12,15). Urinary tract infection symptoms should also be considered in the history because of the possible association with constipation.16
| History | Clinical significance |
|---|---|
| Abdominal pain | It is important to determine whether pain is relieved or affected by defecation (may suggest irritable bowel syndrome); other causes should be ruled out because abdominal pain is often misdiagnosed as being related to constipation |
| Age at onset of symptoms | Infants younger than 1 month with constipation have a relatively greater likelihood of an organic etiology |
| Dietary changes | May suggest food allergy or intolerance |
| Family history, social history, stressors, school entry | May be associated with the onset of constipation |
| Family's definition of constipation | It is important to assess what caregivers consider as constipation to avoid under/overdiagnosis |
| Fecal incontinence | Suggests fecal impaction |
| Hematochezia | May suggest stools that are hard enough to produce fissures or that are associated with an allergy |
| Other systemic signs (i.e., fever, chills, anorexia, weight loss) | May indicate an organic etiology, such as Hirschsprung disease |
| Presence of withholding behaviors | Important contributor to constipation in younger children; behavior interventions may be beneficial |
| Review of current and previous therapies, including diet, behavior, and medications | It is important to understand factors that may influence treatment outcomes |
| Stool parameters (frequency, consistency using the Bristol stool scale, caliber) | Larger, hard stools may be a sign of withholding; normal bowel movement frequency associated with symptoms may indicate irritable bowel syndrome |
| Timing of meconium passage after birth | Lack of a bowel movement in first 48 hours suggests Hirschsprung disease |
| Urinary symptoms | May suggest urinary tract infection secondary to urinary stasis from chronic constipation |
| Physical examination | Clinical significance |
|---|---|
| Digital rectal examination (not routinely recommended) | Hirschsprung disease, anorectal malformations |
| External examination of the perineum and perianal area (look for anal fissures, skin tags) | Hemorrhoids, anorectal malformations |
| Growth parameters (height, weight, head circumference) | Abnormal growth parameters may indicate an organic etiology (e.g., hypothyroidism, cystic fibrosis) |
| Lax abdominal musculature | May suggest prune belly (Eagle-Barrett syndrome) |
| Neurologic evaluation of reflexes (look for cremasteric, anal wink, patellar) and lower extremities (muscle bulk, tone, power) | Spinal cord abnormality |
| Palpable mass in the lower left quadrant | May suggest impaction |
| Severe abdominal distension | Obstruction, severe or advanced constipation, Hirschsprung disease |
| Spine or back examination (look for hair patches, pits, dimples, scoliosis) | Spinal cord abnormality |
| Thyroid examination (look for thyromegaly, nodules) | Congenital thyroid disease |
| Signs and symptoms | Potential diagnosis |
|---|---|
| Abdominal distension | Hirschsprung disease, impaction, neuroenteric condition (e.g., pseudo-obstruction) |
| Abnormal neurologic examination findings (tight anal sphincter, absent anal wink, absent cremasteric reflex, decreased lower extremity reflexes or tone) | Spinal cord abnormality, anorectal malformation, Hirschsprung disease |
| Delayed passage of meconium (> 48 hours after birth) | Hirschsprung disease, cystic fibrosis, congenital malformation of anorectum or spine |
| Extraintestinal symptoms (bilious vomiting, fever, ill appearance) | Hirschsprung disease, neuroenteric condition |
| Failure to thrive | Hirschsprung disease, cystic fibrosis, metabolic condition, malabsorption |
| Family history of Hirschsprung disease | Hirschsprung disease |
| Gushing of stool with rectal examination | Hirschsprung disease |
| Intermittent diarrhea and explosive stools | Hirschsprung disease |
| Midline pigmentary abnormalities of lower spine | Spinal cord abnormality |
| Occult blood in stool | Hirschsprung disease, food allergy, necrotizing enterocolitis |
| Onset before 1 month of age | Hirschsprung disease, cystic fibrosis, congenital malformation of anorectum or spine, metabolic or endocrine conditions |
| Perianal fistula, abnormal position of anus | Spinal cord abnormality |
| Pilonidal dimple covered by tuft of hair | Spinal cord abnormality |
| Stool caliber | Organic causes such as Hirschsprung disease (constriction from aganglionic segments in Hirschsprung disease results in narrow stools) |
There is insufficient evidence to support routine digital rectal examination for the diagnosis of constipation, especially in children older than one year with no red flag signs or symptoms.6,15 Digital rectal examination may be performed when the diagnosis of constipation is uncertain, to confirm the success of disimpaction treatment, or if organic causes are suspected.
Additional diagnostic testing (i.e., laboratory tests, radiography, colonic transit time, and anorectal manometry) is not required in children with functional constipation and no red flag signs or symptoms.6,17,18 Abdominal radiography is of limited value in diagnosing constipation because it does not have interobserver reliability and accuracy. Abdominal radiography should be reserved for specific clinical circumstances in which a rectal examination is needed but undesirable (e.g., in a child with a history of trauma), the diagnosis is uncertain, or to reevaluate following treatment for disimpaction.2,6,12
Differential Diagnosis
The differential diagnosis for children presenting with constipation is listed in Table 5.12,17,19 Hirschsprung disease can present with delayed passage of meconium (longer than 48 hours after birth), constipation in the first few months of life, severe abdominal distension, and inadequate weight gain. The physical examination can demonstrate an empty rectum with explosive stool upon finger withdrawal. Constipation prevalence in children with cystic fibrosis is between 10% to 57%20 and should be considered in patients who have a family history of the disease or present with constipation and other signs such as respiratory symptoms and failure to thrive. Cow's milk protein allergy can cause constipation associated with blood in the stool.21 There are also psychological and behavior factors that can result in functional constipation, particularly in patients with autism and attention-deficit/hyperactivity disorders.22,23
| Conditions | Recommended diagnostic evaluation (if appropriate) |
|---|---|
| Anatomic malformations of the colon and rectum | |
| Anteriorly displaced anus, anal or colonic stenosis, imperforate anus, pelvic mass (sacral teratoma), stricture | Physical examination, barium enema |
| Drug use/toxin exposure | |
| Antacids, anticholinergics, antidepressants, antihypertensives, attention-deficit/hyperactivity disorder medications, botulism, calcium channel blockers, chemotherapy, diuretics (dehydration), iron intake, heavy metal toxicity (i.e., lead), opiates, phenobarbital, sucralfate (Carafate), vitamin D toxicity | History, drug level, lead level |
| Dietary etiologies | |
| Lack of fiber, starting rice cereal, transitioning from breast milk to formula or cow's milk | Dietary history, cultural patterns of food intake |
| Functional constipation | History and physical examination; routine testing not needed |
| Metabolic conditions | |
| Diabetes insipidus | Serum and urine osmolality |
| Diabetes mellitus | Fasting glucose level |
| Hypercalcemia, hypokalemia | Serum calcium and potassium levels |
| Hypothyroidism | Thyroid studies |
| Neuropathic gastrointestinal disorders | |
| Hirschsprung disease | Rectal suction biopsy in children younger than 12 months; full-thickness biopsy for older children |
| Internal anal sphincter achalasia | Anorectal manometry |
| Visceral myopathy/neuropathy | Colonic manometry |
| Neuronal intestinal dysplasia | Anorectal and colonic manometry |
| Other systemic disorders | |
| Celiac disease | Tissue transglutaminase IgA, total IgA, small intestine mucosal biopsy |
| Connective tissue disorder, mitochondrial disorders | Special testing |
| Cow's milk protein intolerance | Cow's milk elimination from diet |
| Cystic fibrosis | Sweat test, genetic testing |
| Psychiatric disorders | Psychological and psychiatric evaluation |
| Psychosocial | |
| Birth of sibling, depression/anxiety, parental strife/divorce, starting school, sexual abuse, toilet phobia, toilet training | Social history |
| Spinal cord anomalies | |
| Meningomyelocele, spinal cord tumor, tethered cord, trauma | Spinal magnetic resonance imaging, anorectal manometry, urodynamics |
| Other | |
| Abnormal abdominal musculature (prune belly [Eagle-Barrett syndrome], gastroschisis, Down syndrome); anismus, Chagas disease, multiple endocrine neoplasia type 2B, porphyria, uremia | As indicated for the suspected condition |
Treatment
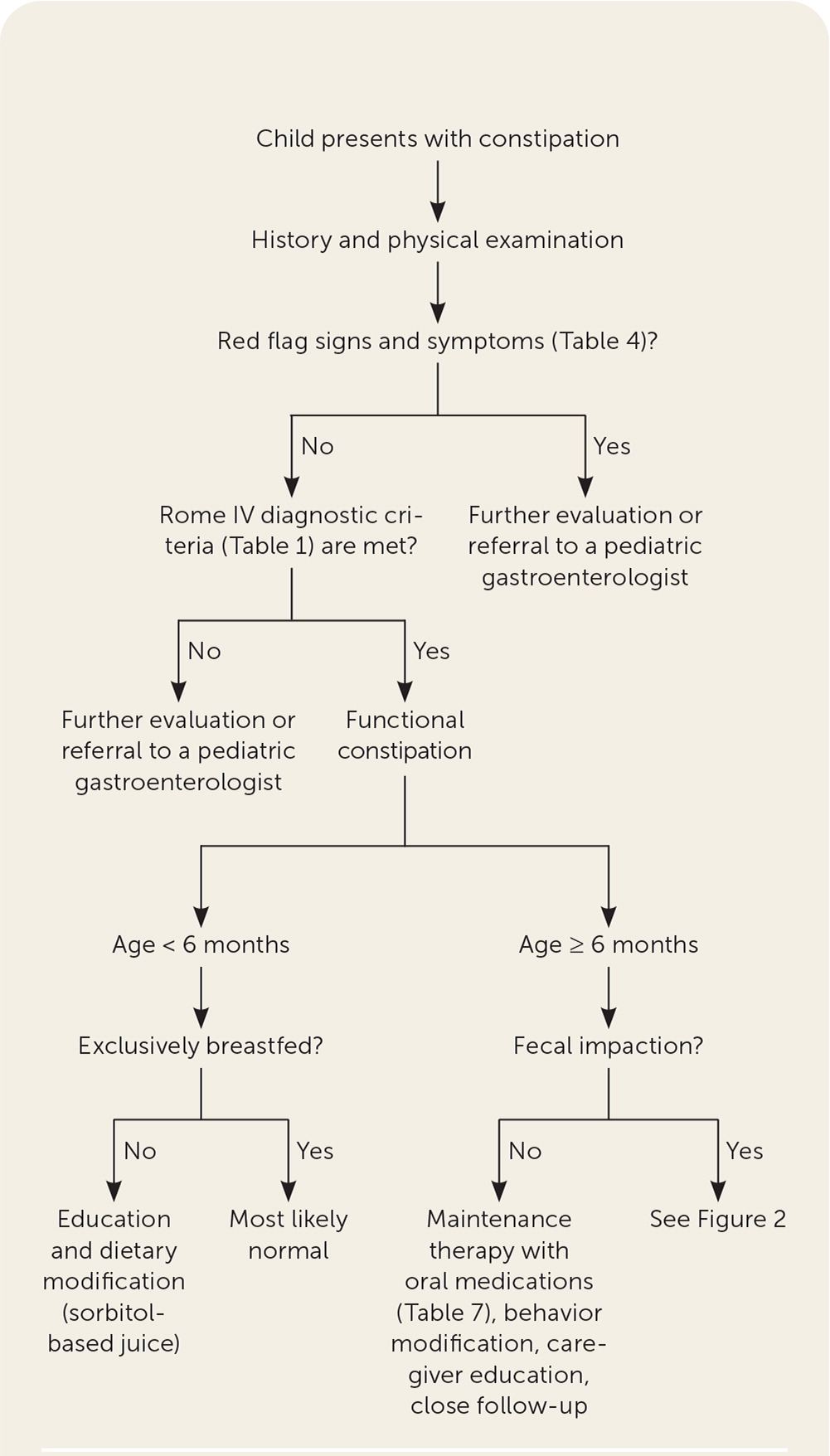
Management of constipation includes dietary modifications, behavior interventions, medications, and disimpaction if needed (Figure 1). Treatment does not differ for preschool-aged children, older children, and adolescents.
DIETARY MODIFICATIONS
Infants respond well to juices containing sorbitol (e.g., apple, prune, pear), which can increase stool frequency and water content in stools. The recommended dose of prune juice for children younger than six months is 1 to 3 mL per kg, which can be diluted with 1 to 2 oz of water.12 Dietary interventions should be used only as first-line treatment for constipation in infants.15
Although low fluid and fiber intake may contribute to the development of constipation, increasing fluid (water, milk, other beverages) or fiber intake above usual daily recommendations does not improve constipation in children.14,24 The recommended daily fluid intake is approximately 4 cups per day for children one to three years of age, 5 cups for children four to eight years of age, and 7 to 8 cups for older children.25 Children and adolescents obtain adequate daily fiber intake from five servings of fruits and vegetables. Recommended daily fiber intake can be calculated by adding 5 g to the child's age in years.26
BEHAVIOR INTERVENTION
Quality of life scores are lower in children with chronic constipation than those without constipation. Children with functional constipation may experience shame, peer rejection, bullying, and recurrent treatment failures.5,24 Adolescents with functional constipation are at increased risk of depression, anxiety, somatic symptoms, withdrawal, and social problems.28 Current evidence does not support intensive behavior therapy or biofeedback in the treatment of functional constipation. However, minor behavior modifications such as structured toilet training with a reward system, in which the child is instructed to defecate after each meal, may prevent recurrence of fecal impaction.6,17
Some studies have shown that combining medical and behavior therapy can improve fecal incontinence and other clinical outcomes.29–31 Clinicians should consider referring children with functional constipation to a child psychologist, particularly when a normal defecating pattern is not restored within three months of starting treatment.29,30
Clinicians should acknowledge the possible negative effects of functional constipation on the child's parents or caregivers. Parents caring for children with constipation report having unmet needs, including lack of knowledge about medication use, a sense of isolation, feeling blamed for the child's condition, dealing with treatment failure, and being dismissed by clinicians.32
DISIMPACTION
For children presenting with fecal impaction, removing the hard stool from the colon is the first step in treating constipation. Fecal impaction can be diagnosed by a history of overflow soiling, the presence of a palpable fecal mass during an abdominal examination, or hard stool in a dilated rectum if a digital rectal examination is warranted.
Disimpaction can be achieved by using oral or rectal medications (Figure 2). Polyethylene glycol (Miralax) is a polymer that is minimally absorbed by the gastrointestinal tract, leading to water retention in the intestine and softened stools. Polyethylene glycol is the first-line treatment because it is more effective than other agents for disimpaction and maintenance therapy, is well-tolerated, and has a low risk of adverse effects.31,33,34
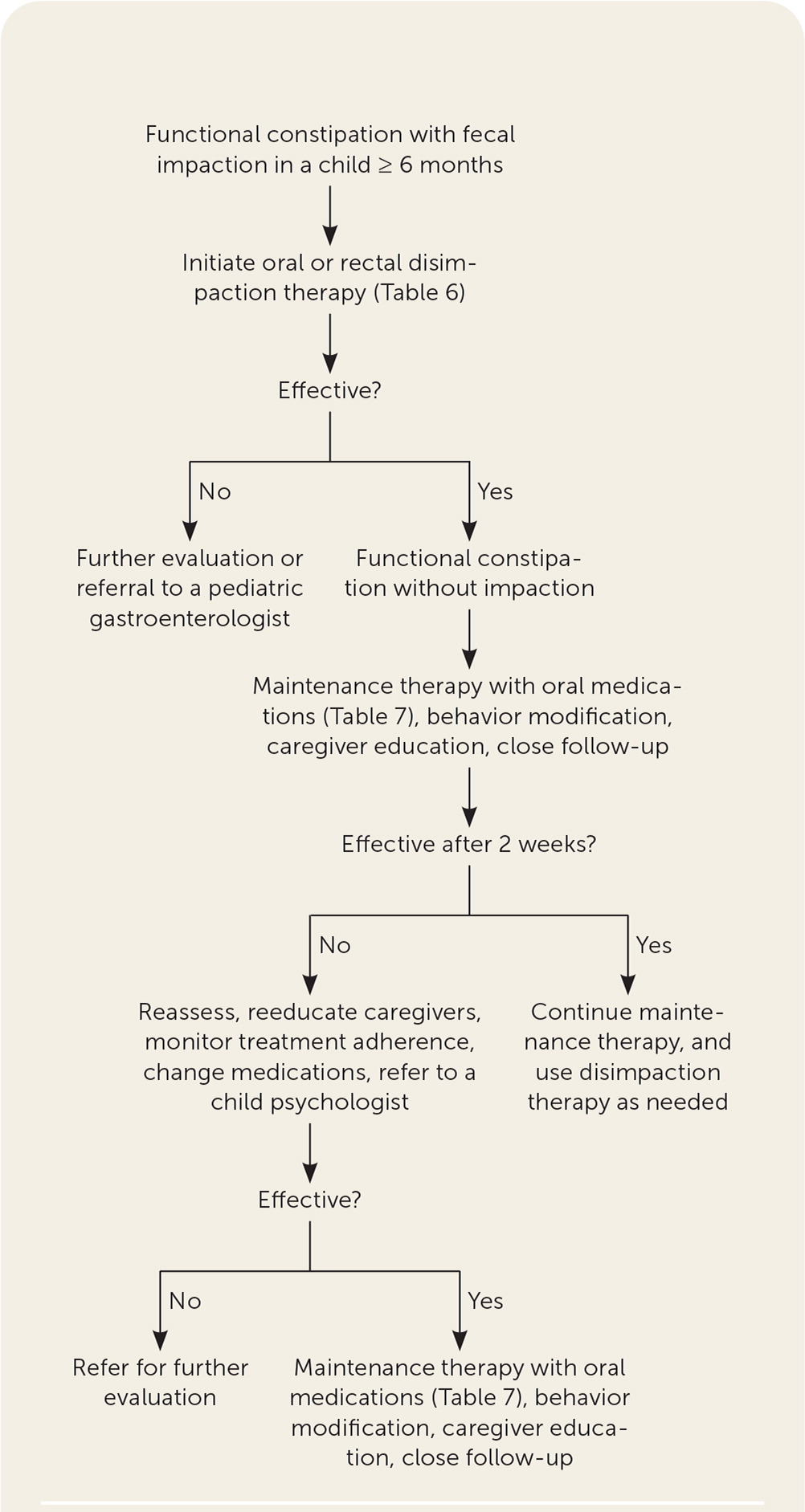
For disimpaction, 1 to 1.5 g per kg of polyethylene glycol mixed in 6 to 8 oz of water or juice is given daily for two to six days. Other oral agents are second-line therapy.12 The North American Society of Pediatric Gastroenterology, Hepatology, and Nutrition recommends using an enema once per day for three to six days as a second-line treatment if polyethylene glycol is not available.6 Enemas are not indicated for infants; therefore, glycerin suppositories are often used. Oral and rectal therapies for disimpaction are summarized in Table 6.2,12
| Therapy | Dosage |
|---|---|
| Oral | |
| Polyethylene glycol (Miralax)* | 1 to 1.5 g per kg per day |
| Lactulose | 1 mL per kg twice per day for up to 12 weeks |
| Magnesium citrate | 4 mL per kg per day |
| Rectal | |
| Enemas (1 per day for 3 to 6 days) | |
| Saline | 5 to 10 mL per kg, administered in the evening |
| Mineral oil | 15 to 30 mL per year of age up to 240 mL |
| Sodium phosphate | < 2 years: should not be used because of the risk of electrolyte abnormality |
| 2 to 4 years: 1 oz on 2 to 3 consecutive evenings | |
| 5 to 11 years: 2.25 oz on 2 to 3 consecutive evenings | |
| 12 years: 4.5 oz on 2 to 3 consecutive evenings | |
| Suppository (1 per day) | |
| Bisacodyl (Dulcolax) | ≥ 2 years: 5 to 10 mg (0.5 to 1 suppository) |
| Glycerin* | 0.5 to 1 infant suppository for those up to five years of age; adult suppository for those ≥ 6 years |
| Other | |
| Manual (rarely used; general anesthesia needed) | — |
If disimpaction is not successful at home, hospitalization is required so that polyethylene glycol can be administered by nasogastric tube. This treatment is started at 10 mL per kg per hour and increased by 10 to 20 mL every one to two hours to a maximum dosage of 40 mL per kg per hour. Digital disimpaction is rarely used and is associated with a risk of colon perforation.2
MAINTENANCE THERAPY
Maintenance therapy should be started in children without impaction or when disimpaction is achieved. The goals of maintenance therapy are to achieve soft stool daily or every other day and to prevent stool impaction. Polyethylene glycol is superior to other oral laxatives and is recommended as a first-line maintenance treatment for constipation.6,35 The starting maintenance dosage of polyethylene glycol is 0.4 g per kg per day, and caregivers should be advised that it can be increased or decreased to maintain soft stool every day or every other day without diarrhea. Polyethylene glycol appears to be safe for long-term use in children.36 Lactulose is a second-line maintenance treatment if polyethylene glycol is not available. Other second-line therapies include milk of magnesia, stimulant laxatives, and mineral oil.6 Table 7 summarizes maintenance therapies, including dosing and common adverse effects.12,15
| Therapy | Dosage | Adverse effects |
|---|---|---|
| First-line osmotics | ||
| Polyethylene glycol (Miralax)* | 0.4 to 1.5 g per kg up to 17 g per day | Anaphylaxis, flatulence |
| Second-line osmotics | ||
| Lactulose* | 1 to 3 mL per kg per day in 2 divided doses | Abdominal cramps, flatulence |
| Milk of magnesia (magnesium hydroxide) | < 2 years: 0.5 mL per kg per day 2 to 5 years: 5 to 15 mL per day 6 to 11 years: 15 to 30 mL per day ≥ 12 years: 30 to 60 mL per day Medication may be given at bedtime or in divided doses | Infants are susceptible to magnesium overdose (hypermagnesemia, hyperphosphatemia, hypocalcemia) |
| Sorbitol (e.g., prune juice)* | 1 to 3 mL per kg once or twice per day in infants | Similar to lactulose |
| Stimulants | ||
| Bisacodyl (Dulcolax) | 3 to 12 years: 5 to 10 mg (1 to 2 tablets) once per day > 12 years: 5 to 15 mg (1 to 3 tablets) once per day | Abdominal cramps, diarrhea, hypokalemia, abnormal rectal mucosa, proctitis (rare), urolithiasis (case reports) |
| Senna* | 1 to 2 years: 1.25 to 2.5 mL (2.2 to 4.4 mg) at bedtime; maximum of 5 mL or 8.8 mg per day 3 to 6 years: 2.5 to 3.75 mL (4.4 to 6.6 mg) or 0.5 tablet (4.3 mg) at bedtime; maximum of 7.5 mL or 1 tablet per day 7 to 12 years: 5 to 7.5 mL (8.8 to 13.2 mg) or 1 tablet (8.6 mg) at bedtime; maximum of 15 mL or 2 tablets per day > 12 years: 10 to 15 mL (26.4 mg) or 2 tablets (17.2 mg) at bedtime; maximum of 30 mL or 4 tablets per day | Idiosyncratic hepatitis, melanosis coli, hypertrophic osteoarthropathy, analgesic nephropathy |
| Lubricants | ||
| Mineral oil | 1 to 3 mL per kg per day divided into 2 doses | Lipoid pneumonia if aspirated, theoretical interference with absorption of fat-soluble substances, foreign body reaction in intestine |
Maintenance therapy should be continued for at least two months or at least one month after a good response to treatment.6 Medications should be weaned gradually and may need to be continued for months or years in some patients. If functional constipation develops before toilet training, maintenance therapy should be continued until after toilet training is achieved. Relapses are common and should be treated with maintenance therapy or disimpaction therapy when appropriate.
Rarely, surgical intervention is required to treat refractory constipation. Emerging therapies such as neuromodulation, microbiome therapies, and fecal microbiota transplantation may have a role in treating constipation in the future.24 Other organic causes of constipation are treated with the same medications as functional constipation in conjunction with evaluation and treatment of the underlying cause.
Long-term Prognosis
After constipation is diagnosed and the treatment plan is determined, frequent follow-up is recommended to ensure that disimpaction has been achieved and that maintenance therapy is effective.7 These follow-up visits also ensure caregiver education and discussions of barriers to implementing treatment recommendations. Clinicians should educate caregivers about functional constipation's chronic course and frequent relapses, and the possible need for prolonged therapy. A patient handout on functional constipation is available at https://gikids.org/wp-content/uploads/2020/03/Constipation-all-English.pdf.
A recovery rate of 50% to 60% is reported after one year of intensive treatment,6 and about 25% of children continue to have symptoms through adulthood.37 Clinician use of treatment and medication dosing guidelines can decrease the risk of undertreating functional constipation.38 Referral to a pediatric gastroenterologist is recommended if the patient has red flag signs and symptoms or treatment is ineffective.
This article updates previous articles on this topic by Nurko and Zimmerman12 and Biggs and Dery.39
Data sources: A PubMed search was completed in Clinical Queries using the key terms constipation, constipated, and children or child. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were Scopus, Embase, Google Scholar, Web of Science, Cochrane database, Essential Evidence Plus, and DynaMed. Search dates: November 19, 2020, and December 14, 2021.
