Health Equity Fellow Targets Obesity in Clinic, Community
January 06, 2020 09:00 am David Mitchell – Keisha Harvey, M.D., can relate to some of the biggest challenges patients face in Washington Parish, La., where 37% of the population has obesity and 25% lives below the poverty line.
"It hits home for me. My mother suffered from obesity," said Harvey. "My mother put forth her best efforts to live a healthier lifestyle and lose weight. We would get up every morning at 5 a.m. and walk to attempt to lose weight. We tried multiple diets that would only lead to short-term weight loss. Due to my journey with my mom, I learned that just because you're overweight doesn't mean you have to have negative health outcomes. There's a holistic aspect to health. You have to start with what's best for yourself and what you can improve."
Harvey, one of the AAFP's Health Equity Fellows, is trying to help patients at her solo practice do just that. Her yearlong fellowship project will include educating patients about healthy lifestyles, encouraging changes and assessing their progress, as well as an education component for residents at the Louisiana State University Rural Family Medicine Residency Program in Bogalusa and outreach to local physicians regarding obesity bias.
"I'm going to do everything I can to make sure this is a community effort and not just my personal agenda," said Harvey, who also is connecting with civic leaders and has secured an agreement with a local church to provide free gym space. "I'm going to do the work and hopefully we can get a good, strong group of people who want to make changes."
The residency program already has a weekly Walk With a Doc program that encourages patients to exercise and connects them to physicians, but Harvey hopes to expand the concept to offer other forms of exercise that might draw more participants and build more relationships between patients and doctors.
The need is great. In addition to the staggering obesity statistic, more than half of the parish's population has hyperlipidemia, half has hypertension and 13% has diabetes. Harvey is doing a series of interviews with a local radio station about obesity and related issues, including nutrition, exercise and mental health, in an effort to reach patients.
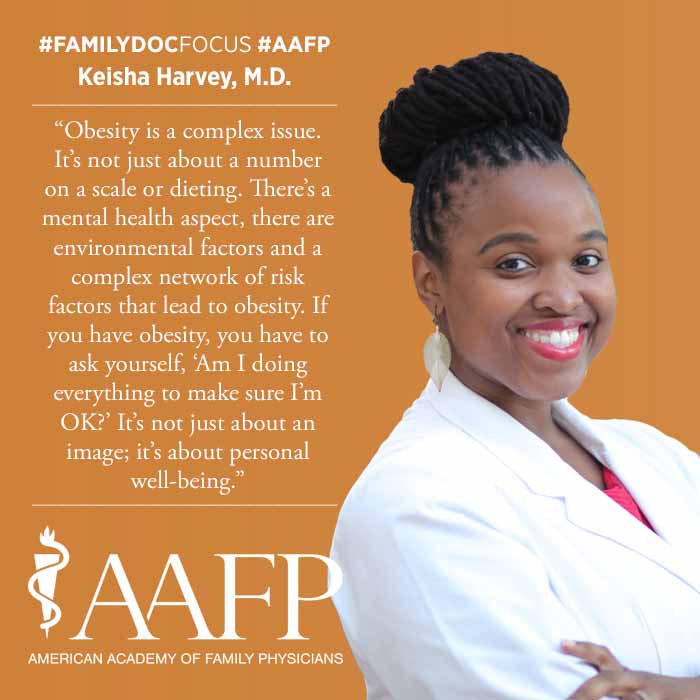
"Obesity is a complex issue," she said. "It's not just about a number on a scale or dieting. There's a mental health aspect, there are environmental factors and a complex network of risk factors that lead to obesity. If you have obesity, you have to ask yourself, 'Am I doing everything to make sure I'm OK?' It's not just about an image; it's about personal well-being."
Harvey also hopes to reach her peers. Too often, she said, doctors don't do enough to address weight gain or obesity. Physicians can help patients with obesity be more comfortable in health care settings -- and be more likely to seek care -- by addressing obesity bias. That, Harvey added, means equipping practices with chairs, exam tables and gowns that are sized appropriately for patients with obesity. Practices also can take extra steps, such as avoiding weighing patients in busy hallways to protect their privacy.
In addition to tracking patients' progress, Harvey hopes to assess what residents learn during the project, as well as what changes other physicians make regarding their approach to obesity.