
Am Fam Physician. 1998;58(4):873-884
Patient information: See related handout on skin cancer, written by the author of this article.
Malignant lesions of the skin are common. Patients who develop squamous cell carcinoma and malignant melanoma often have recognizable precursor conditions. A few skin lesions resemble malignancies. Lesions that are growing, spreading or pigmented, or those that occur on exposed areas of skin are of particular concern. Knowing the similarities and differences between these lesions allows the primary physician to make a diagnosis in most cases by simple inspection and palpation. When in doubt, it is appropriate to perform an excisional biopsy of small lesions or punch biopsy of larger lesions. Removal of premalignant lesions will reduce the occurrence of malignant disease. Almost all skin cancers can be cured by early excision or destruction. For these reasons, physicians should be aware of the risk factors for skin cancer, educate patients about risk reduction and include skin inspection for premalignant and malignant lesions as a part of routine health maintenance examinations.
Primary neoplastic disease of the skin is common. Early recognition of such lesions is important because complete excision will cure almost all cases of skin cancer if performed in the early stages. A presumptive diagnosis can often be made by considering the patient's risk factors, the history of the lesion and its location, appearance and texture. The definitive diagnosis is made by histologic examination of biopsy specimens.
Factors that Contribute to Skin Cancer
Most primary skin neoplasms occur in skin that is exposed to adverse conditions. Ultraviolet light from sunlight is most often a contributing factor. Desert sunlight is particularly dangerous, but water and snow both reflect a high proportion of the ultraviolet light from the sky, increasing the risk for sailors, beach lovers and winter-sports enthusiasts. In farmers and ranchers, the skin of the face, neck and arms is also at high risk.
Exposure to immunosuppressive drugs or ionizing radiation is a less common cause.1 Use of organic arsenics and tars predisposes to skin cancer. A history of malignant melanoma in a first-degree relative or the presence of numerous melanotic nevi, which may be familial or sporadic, greatly increases the risk of developing malignant melanoma.2–4 Persons with fair or freckled skin that does not tan are at increased risk. Dark hair and skin provide some protection from skin cancer. Family physicians should educate their patients about these risks and encourage them to protect their skin.
Skin lesions come to the attention of the physician in three ways: (1) the patient may be aware of the lesion and consult the physician about it; (2) the physician may notice the lesion when examining the patient for some other reason; or (3) the physician inspects the entire skin surface for lesions as part of a pre-employment or health maintenance examination. A complete skin examination is important particularly in high-risk patients because, at the stage when they are curable, skin cancers are painless and often inconspicuous. The top of the head, the face, the neck, the shoulders and the extensor surfaces of the arms are particularly important, but the areola, the vulva and the foreskin are also areas of high risk. In black patients, the palms of the hands, soles of the feet and periungual areas are particularly vulnerable. A detailed description and measurement of all suspicious skin lesions should be documented in the patient's medical record.
Basal Cell Carcinoma
Comprising 60 percent of primary skin cancers, the basal cell carcinoma is a slow-growing lesion that invades tissue but rarely metastasizes. Most metastatic basal cell carcinomas arise from large tumors.5 Basal cell carcinomas that have recurred after excision may be at greater risk of metastasis.6 Basal cell carcinoma is common on the face and on other exposed skin surfaces but may occur anywhere (Figure 1). The common form first appears as a small round or oval area of skin thickening. Usually there is no itching, pain or change in skin color. The area very slowly extends circumferentially, creating a slightly raised edge, which may have a shiny, pearly or slightly translucent appearance (Figure 2).


As the lesion continues to grow, the central area becomes atrophic, leaving a hollow that is covered by thin skin, often with visible vessels, which eventually ulcerates (Figure 3). The growing edges become more irregular, and the shape becomes uneven. The base is also invasive and gradually erodes the underlying tissue, making it difficult to excise the lesion completely.

Less common forms include a superficial basal cell carcinoma that resembles a patch of dermatitis, a pigmented basal cell carcinoma that resembles a nodular malignant melanoma and an aggressive-growth basal cell carcinoma. Aggressive-growth basal cell carcinoma is an infiltrating sclerosing lesion that may appear similar to a scar with a firm or hard base. In patients younger than 35 years, basal cell carcinoma tends to adopt the more aggressive forms.7
No premalignant conditions precede basal cell carcinoma. Basal cell carcinoma and lesions of similar appearance are compared in Table 1.
| Lesion | Location | Surface | Color | Outline | Other features |
|---|---|---|---|---|---|
| Basal cell carcinoma | Most common on face, but can occur anywhere | Raised, pearly, firm | Normal skin color | Round at first, irregular later | May ulcerate |
| Superficial basal cell carcinoma | Any location | Roughened | Skin-colored or pink | Round or irregular | Resembles dermatitis |
| Pigmented basal cell carcinoma | Most commonly occurs on the face | Nodule | Growing area is dark brown or black | Becomes irregular as growth progresses | Looks like a nodular malignant melanoma |
| Infiltrating basal cell carcinoma | Any location | Smooth | Skin-colored | Various | Looks like a firm scar that grows aggressively |
| Tricoepithelioma | Any location | Raised, pearly | Normal skin color | Round | Does not become malignant |
| Keloid after | Site of previous injury | Raised, rounded, smooth | Usually pink, may be skin-colored | Varies, often linear | Often large, but no growth one year |
| Molluscum contagiosum | Face and hands of children, areas of sexual contact | Raised, rounded central hollow | Skin-colored | Round | Usually multiple, in clusters or scattered; contagious |
| Soft, fleshy | |||||
| Dermatofibroma | Often occurs on limbs, rarely on face | Flat or slightly raised, edge not thickened or pearly | Skin-colored, firm under the surface but not on the surface | Usually round or oval | Usually >5 mm diameter when first noticed |
Squamous Cell Carcinoma
Squamous cell carcinoma comprises 20 percent of all cases of skin cancer. It typically occurs on areas of the skin that have been exposed to sunlight for many years. It may also appear in areas that have been subjected to ionizing irradiation or in other locations in patients who have undergone treatment with immunosuppressive drugs1 or have been exposed to organic trivalent arsenic compounds or tars. Squamous cell carcinoma of the lip may be related to pipe smoking, as well as to sunlight exposure.
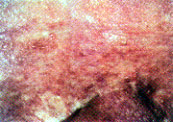
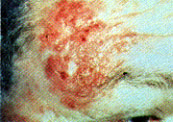
Human papillomavirus infection may be a precursor of keratoacanthoma and periungual, genital and other squamous cell carcinomas, especially in immunosuppressed patients.8 The affected area develops a slight redness, scaling, fissuring and an uneven surface. Superficial dilated vessels may be visible. The lesion often appears very dry and may bleed when stretched or abraded. It spreads laterally from the edges and may heap up irregularly. New lesions often appear near old ones. Clusters of lesions may occur as fleshy masses (Figure 4). The centers may become atrophic and develop raw patches or frank ulceration (Figure 5).


Two other skin lesions are considered part of the squamous cell carcinoma spectrum. The first type, keratoacanthoma, is closely related to squamous cell carcinoma. Like squamous cell carcinoma, it appears on skin damaged by sunlight or chemicals. It often occurs at the site of trauma, especially in immunosuppressed patients. It is sometimes associated with human papillomavirus infection. Keratoacanthoma appears as a skin-colored or pink smooth lesion, which becomes dome-shaped during a period of very rapid growth. When mature, it is volcano-shaped, with protruding masses of keratin resembling lava. Classic keratoacanthoma is not malignant and regresses spontaneously, but atypical lesions may actually be squamous cell carcinoma.7 Many dermatopathologists include keratoacanthoma in the spectrum of squamous cell carcinoma9 (Figure 6).

The second type is verrucous carcinoma, a variant of squamous cell carcinoma that features an irregular warty surface (Figure 7).

While metastasis of common sunlight-induced squamous cell carcinoma is unusual, lesions more likely to metastasize are lesions of the lip or ear, lesions that recur after previous therapy, lesions at the site of a burn and those that are more deeply invasive. Squamous cell carcinoma of the skin may be metastatic from other locations (Figure 8).
A variety of skin lesions are considered precursors of squamous cell carcinoma. Actinic keratosis appears very similar to the less severe lesions of squamous cell carcinoma. It is always found on skin that has received heavy exposure to sunlight.9,10 Actinic keratosis should be sought during routine inspection of the skin, especially in fair-skinned patients who have been exposed to sunlight frequently. Regular reexamination of affected skin and treatment of any areas showing growth or change can prevent neoplastic transformation or provide early treatment of malignancy11 (Figure 9).
Epidermodysplasia verruciformis is an uncommon autosomal recessive disorder that predisposes patients to the development of squamous cell carcinoma (Figure 10). Actinic cheilitis is a condition that is similar to actinic keratitis but occurs on the vermilion of the lips.


Human papillomavirus includes several strains that are associated with squamous cell carcinoma, especially in the genital areas.12 The virus may not be a precursor of squamous cell carcinoma but does increase the patient's risk for developing squamous cell carcinoma. In Table 2, squamous cell carcinoma and its variants are compared with other lesions of similar appearance (Figures 13 through 16).
| Lesion | Location | Surface | Color | Outline | Other features |
|---|---|---|---|---|---|
| Squamous cell carcinoma | Areas exposed to sunlight, radiation or arsenicals | Rough, irregular, sometimes scaly, sometimes has visible vessels, sometimes warty or with fleshy masses | Skin-colored at first, sometimes reddened later | Vague | New lesions may appear near old ones |
| Does not clear with corticosteroid therapy | |||||
| Keratoacanthoma (a variant of squamous cell carcinoma) | Exposed areas, especially face and hands | Smooth dome, becoming volcano-shaped | Skin-colored or slightly reddened | Well-defined | Goes through aperiod of very rapid growth, often regresses |
| Eczema and atopic dermatitis (Figure 13) | Atopic dermatitis behind ears, on flexure areas | Reddened, slightly scaly, sometimes with vesicles | Dry at first, fissured, may weep | Indefinite | Common in atopic persons and those exposed to irritants |
| Contact dermatitis (Figure 14) | Wherever skin comes in contact with an irritant | Reddened, slightly scaly, sometimes with vesicles | Dry at first, fissured, may weep | Circumscribed | Dermatitis clears with corticosteroid therapy |
| Psoriasis (Figure 15) | Elbows, knees, scalp, sacral cleft, nails | Scaly with underlying reddened base | White dry scales, smooth pink or red wherescales are removed; may bleed | Well-demarcated; round, irregular or confluent | Often widespread, sometimes itchy; varies with season |
| Seborrheic dermatitis (Figure 16) | Scalp, forehead, nasolabial fold, midline trunk | Raised, with scales | Yellow or brown | Well-demarcated | Some lesions can be easily removed |




Malignant Melanoma
Although it comprises only 1 percent of skin cancers, malignant melanoma accounts for over 60 percent of skin cancer deaths.13 It metastasizes to remote sites early, and its metastases are characteristically unresponsive to treatment. Like the other skin cancers, malignant melanoma is more common on skin that has undergone excessive exposure to sunlight, but it can occur anywhere. Four types of malignant melanoma are identified.
The lesions of superficial spreading melanoma are dark brown or black. In the initial phase they have a slowly spreading irregular outline. Some areas may be a lighter shade. Vertical growth occurs later, penetrating into the dermis and causing some parts of the lesion to become raised. This is the most common kind of melanoma (Figure 17).

Nodular melanoma grows vertically from the start and is more likely to mestastasize early. It has little or no lateral extension, appearing as a shiny black dome.
Lentigo maligna melanoma occurs in a pre-existing lentigo maligna. The appearance of one or more nodules signals the change to an invasive lesion (Figure 18).

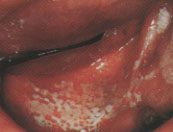
Acral lentiginous melanoma occurs on the palms of the hands, the soles of the feet, under the nails and on mucosal surfaces. It is uncommon, comprising only 5 percent of melanomas in pale-skinned persons. Dark-skinned persons rarely get melanomas, but if they do, the lesions are likely to be acral melanomas (Figure 19).

Since not all malignant melanomas are visibly pigmented, physicians should be suspicious of any lesion that is growing or that bleeds on minor trauma. If the diagnosis is in doubt, it is better to take one or more adequate full skin thickness biopsies for histologic examination.
Certain skin lesions are considered precursors of malignant melanoma. Blue nevi occasionally become the site of melanocytic malignant change. Suspicious features, such as location on the scalp of men in their forties, growth, bleeding on minor trauma and the occurrence of dark satellite lesions around the nevus, may signal this change. All blue nevi should be carefully monitored or excised (Figure 20).

Lentigo maligna (melanotic freckle of Hutchison) occurs on the face or other sun-exposed skin of older, fair-skinned persons. It is a brown macule with some color variation, spreading slowly and unevenly at the edges. Dark invasive lesions with irregular borders may grow from it (Figure 18). Congenital nevomelanocytic nevi are brown patches of skin that are present at birth or develop in infancy. They usually have an irregular surface, and they may be slightly raised and exhibit coarse hair. Lesions that are more than 20 cm across are more likely to undergo neoplastic change into malignant melanoma, often when the child is between three and five years of age.
The presence of 10 or more dysplastic nevi confers a 12-fold risk of developing malignant melanoma.2 Dysplastic nevi may appear de novo or may develop from common melanocytic nevi.3 They occur in 5 percent of the general white population, but in 30 to 50 percent of those with sporadic (nonfamilial) primary melanoma and in almost all patients with familial cutaneous melanoma.4
In Table 3, the common varieties of malignant melanoma are compared with lesions of similar appearance (Figures 21 through 23).
| Lesion | Location | Surface | Color | Outline | Other features |
|---|---|---|---|---|---|
| Superficially spreading malignant melanoma | Most common on sun-exposed skin, but can occur anywhere | Smooth; vertical growth occurs later | Dark brown or black, may be variegated | Becomes more irregular as it grows | May have a pink or reddish halo |
| Nodular melanoma | Most common on sun-exposed skin, but can occur anywhere | Nodular form | Dark brown or black, may be variegated | May be regular or irregular | Grows aggressively, invades early |
| Lentigo maligna melanoma | In a pre-existing lentigo maligna, usually facial | Nodular against a smooth background | Dark or black on pale brown background | Irregular | |
| Acral lentiginous melanoma | Nailbeds, palms of the hands, soles of the feet, mucosal areas | Smooth | Dark brown or black | Irregular | Occurs in both black and white persons |
| Common melanocytic nevi (Figure 21) | Widely scattered | Smooth, flat or uniformly elevated | Uniform light or dark brown | Regular, round or oval, rarely >10 mm diameter | Less common in black persons |
| Lentigo (freckles) | Mainly on sun-exposed surfaces | Smooth, flat brown or tan | Uniform light | Round, oval or polyhedric | Darken with sun exposure, lighten in winter |
| Blue nevi (Figure 20) | Most commonly occur on hands or feet; may occur anywhere | Papules or nodules | Blue, blue-gray, or blue-black | Round or oval, usually <10 mm diameter | Firm on palpation |
| Pigmented basal cell carcinoma (Figure 23) | Most common on the face | Nodule | Growing area is dark brown or black | Becomes irregular as growth progresses |



Other Primary Malignancies of the Skin
Kaposi's sarcoma appears as intensely red, nonblanching, slightly raised or nodular lesions of the skin and mucous membranes. Usually there are many lesions of various sizes. It occurs more frequently in patients with acquired immunodeficiency syndrome (Figure 24).

Sebaceous carcinoma has a nonspecific appearance similar to that of a squamous cell carcinoma of the skin, with nodularity, telangiectasias and hair loss (Figure 25).

Malignant eccrine spiradenoma is a slowly growing, deeply invasive sclerotic plaque that occurs on the face of older women. It is often painful (Figure 26).

Syringoid sweat duct carcinoma is a rare malignant condition that occurs on the face or scalp of elderly patients, causing local hair loss. The surface may be warty and secrete fluid (Figure 27).

Paget's disease of the nipple appears to be an unresponsive eczema of the areola but actually is a carcinoma in the ducts of the breast that grows outward to involve the skin.
Squamous cell carcinoma may be treated by excision, cryotherapy or topical chemotherapy; it should be diagnosed by full skin thickness punch biopsies. For basal cell carcinoma and other skin malignancies, it is better to remove the lesion completely whenever possible, with lateral and deep margins of several millimeters of healthy tissue. If any of the ABCD signs are found in a new pigmented lesion or in a melanocytic nevus that was previously uniformly colored, smooth, flat, round or oval (Figure 28), an excisional biopsy should be performed. All suspicious lesions should be excised down to a connective tissue base with a 2- to 3-mm lateral margin.15

If a cosmetically acceptable result would be difficult to obtain after excisional biopsy, full skin thickness punch biopsy of several areas may be performed, including the margins and any raised areas. If a biopsy shows dysplasia, the whole lesion should be removed with 5-mm margins using plastic surgical techniques, and the site should be monitored for recurrence. Malignant melanoma also requires excision with a margin of at least 5 mm, and many dermatologists recommend a 2-cm margin. All other pigmented lesions that occur in these patients should be observed for change at least annually. Serial photographs may be valuable.16
Final Comment
Physicians should assist patients in reducing factors that increase the risk for developing skin cancer. A complete skin examination for premalignant and malignant lesions should be performed during periodic health evaluations and when other opportunities occur. By doing so, the vigilant physician can intervene and reduce the morbidity and mortality of malignant skin disease. Excisional biopsy with an adequate margin is recommended whenever possible. For a large lesion, multiple punch biopsies of selected areas, including the growing edge, is an acceptable method for reaching a diagnosis. In these cases the definitive excision will require plastic surgical techniques. Mohs' micrographic surgery is a technique in which the histology of each layer of tissue is determined before removing the next layer. This technique permits complete excision without excessively large margins.17,18