
A more recent article on obstructive sleep apnea is available.
Am Fam Physician. 1999;60(8):2279-2286
Obstructive sleep apnea is a significant medical problem affecting up to 4 percent of middle-aged adults. The most common complaints are loud snoring, disrupted sleep and excessive daytime sleepiness. Patients with apnea suffer from fragmented sleep and may develop cardiovascular abnormalities because of the repetitive cycles of snoring, airway collapse and arousal. Although most patients are overweight and have a short, thick neck, some are of normal weight but have a small, receding jaw. Because many patients are not aware of their heavy snoring and nocturnal arousals, obstructive sleep apnea may remain undiagnosed; therefore, it is helpful to question the bedroom partner of a patient with chronic sleepiness and fatigue. Polysomnography in a sleep laboratory is the gold standard for confirming the diagnosis of obstructive sleep apnea; however, the test is expensive and not widely available. Home sleep studies are less costly but not as diagnostically accurate. Treatments include weight loss, nasal continuous positive airway pressure and dental devices that modify the position of the tongue or jaw. Upper airway and jaw surgical procedures may also be appropriate in selected patients, but invasiveness and expense restrict their use.
Obstructive sleep apnea is a disorder in which complete or partial obstruction of the airway during sleep causes loud snoring, oxyhemoglobin desaturations and frequent arousals. As a result, affected persons have unrestful sleep and excessive daytime sleepiness. The disorder is associated with hypertension,1 impotence and emotional problems.2 Because obstructive sleep apnea often occurs in obese persons with comorbid conditions, its individual contribution to health problems is difficult to discern. The disorder has, however, been linked to angina,3 nocturnal cardiac arrhythmias,4 myocardial infarction,5 stroke6 and motor vehicle crashes.7
Even though obstructive sleep apnea is fairly common, it often remains undiagnosed in primary care practice. Because the disorder is associated with significant morbidity and even some mortality,8 family physicians need to be familiar with its clinical presentation and treatment.
Pathophysiology
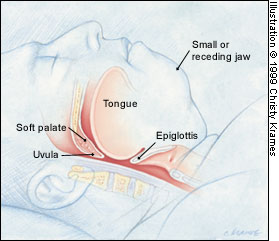
Obstructive sleep apnea is caused by repetitive upper airway obstruction during sleep as a result of narrowing of the respiratory passages. Patients with the disorder are most often overweight, with associated peripharyngeal infiltration of fat9 and/or increased size of the soft palate and tongue.10 Some patients have airway obstruction because of a diminutive or receding jaw that results in insufficient room for the tongue. These anatomic abnormalities decrease the cross-sectional area of the upper airway. Decreased airway muscle tone during sleep and the pull of gravity in the supine position further decrease airway size, thereby impeding air flow during respiration.
Initially, partial obstruction may occur and lead to snoring. As tissues collapse further or the patient rolls over on his or her back, the airway may become completely obstructed. Whether the obstruction is incomplete (hypopnea) or total (apnea), the patient struggles to breathe and is aroused from sleep. Often, arousals are only partial and are unrecognized by the patient, even if they occur hundreds of times a night. The obstructive episodes are often associated with a reduction in oxyhemoglobin saturation.
With each arousal event, the muscle tone of the tongue and airway tissues increases. This increase in tone alleviates the obstruction and terminates the apneic episode. Soon after the patient falls back to sleep, the tongue and soft tissues again relax, with consequent complete or partial obstruction and loud snoring.
Cycles of sleep, snoring, obstruction, arousal and sleep occur throughout the night. Some patients with severe apnea may have episodes of upper airway obstruction a hundred or more times in one hour. Multiple arousals with sleep fragmentation are the likely cause of excessive daytime sleepiness in patients with obstructive sleep apnea.11 Patients often complain of unrestful sleep and sometimes lament that they are sleepier in the morning than when they go to bed at night.
SITES OF AIRWAY OBSTRUCTION
Airway obstruction can occur in many areas of the nasopharynx, oropharynx and hypopharynx (Figures 1a and 1b). Although the contribution of nasal polyps and septal deviation to obstructive sleep apnea remains controversial, some investigators believe that partial or total nasal obstruction can lead to hypopnea and apnea.12
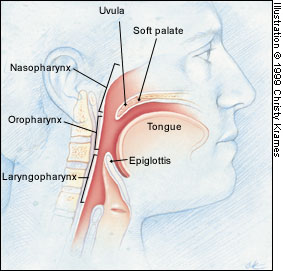
More commonly, airway obstruction occurs in the oropharynx. Redundant peripharyngeal tissue reduces the size of the posterior airway, which increases the chance of obstruction during sleep. An elongated soft palate and enlarged uvula may further compromise the airway. As mentioned previously, decreased muscle tone during sleep also contributes to airway collapse.
The base of the tongue is a common site of hypopharyngeal obstruction in sleep apnea. Patients with a small or receding jaw are at increased risk for obstruction. Occasionally, obstruction may be caused by an enlarged tongue. In this setting, obstruction occurs when the base of the tongue impinges on the airway just above the glottis.
Prevalence and Characteristic Features
Obstructive sleep apnea is more common than was previously thought. Reported prevalence rates vary widely, and asymptomatic sleep apnea is more common than symptomatic, clinically significant obstructive sleep apnea. Population-based studies suggest that 2 percent of women and 4 percent of men over the age of 50 years have symptomatic obstructive sleep apnea.13
Considering the prevalence rates, most family physicians probably have a number of patients with undiagnosed sleep apnea. The way to find these patients is to be aware of the common signs and symptoms of obstructive sleep apnea and to carefully examine any patient who complains of snoring or daytime sleepiness (Table 1). A suggested self-administered screening questionnaire is presented in Figure 2.14 Because the patient is often unaware of the nocturnal arousals, it may be helpful to have the bedroom partner also complete the questionnaire.
| Loud snoring |
| Disrupted sleep |
| Nocturnal gasping and choking |
| Witnessed apnea |
| Daytime sleepiness and fatigue |
| Crowded posterior airway |
| Short, thick neck |
TYPICAL OBSTRUCTIVE SLEEP APNEA
The patient with obstructive sleep apnea is often brought to the physician's office by a family member or bedroom partner who is being disturbed by the patient's loud snoring. The bedroom partner may describe episodes in which the patient stops breathing and then gives a loud gasp or snort when aroused by the apnea. The snoring and apneic episodes may be worse after the patient drinks alcohol or takes sleeping pills, because these sedatives decrease pharyngeal muscle tone and can exacerbate obstructive sleep apnea.15,16
Daytime fatigue and sleepiness are the most significant complaints of the patient with obstructive sleep apnea. Frequently, the patient falls asleep during sedentary activities, such as watching television or sitting in a movie theater. Near-miss automobile crashes may occur because the patient dozes off behind the wheel.
As daytime sleepiness becomes more excessive, the patient may report falling asleep in embarrassing situations, such as during meals or when sitting in a car stopped at a traffic light. The patient also complains of being tired on awakening in the morning.17 The patient often has to nap during the day but typically wakes up unrefreshed.
Physical Examination
Most patients with obstructive sleep apnea are overweight and typically have a short, thick neck (Figure 3). A neck circumference greater than 16 inches in a woman or greater than 17 inches in a man correlates with an increased risk for the disorder.18 Furthermore, increasing neck size has been shown to correlate with the severity of apnea.19,20

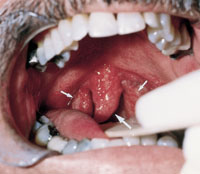
The physical examination reveals a crowded posterior airway in some patients with obstructive sleep apnea. These patients may have an enlarged floppy uvula or tonsillar hypertrophy (Figure 4).14 An elongated soft palate that rests on the base of the tongue is another cause of the airway obstruction sometimes seen in patients with sleep apnea (Figure 5).14

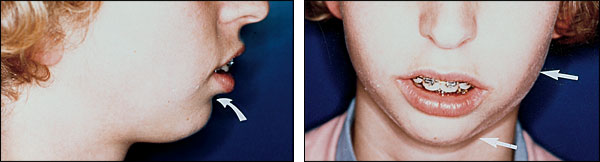
Many patients with obstructive sleep apnea have lower-face abnormalities, which may include a small chin, maxilla and mandible, as well as a large tongue (Figures 6, 7 and 8).14 These findings may not be obvious in some patients, but a receding jaw with 2 mm or more of overbite resulting in a prominent mental cleft or curling of the lower lip may be more readily discerned by the family physician.

UNCOMMON CAUSES
Occasionally, obstructive sleep apnea can be caused by less common medical problems, including hypothyroidism,21 acromegaly22 and renal failure. Neuromuscular disorders such as postpolio syndrome can result in inadequate neuromuscular control of the upper airway and lead to obstructive sleep apnea.23 Restrictive lung disease from scoliosis has also been associated with the disorder.24
Objective Evaluations
A presumptive clinical diagnosis of obstructive sleep apnea can sometimes be made in patients with a short, thick neck who complain of snoring and excessive daytime sleepiness. Still, objective testing can be helpful in confirming the diagnosis and excluding other sleep disorders that might be causing the symptoms.
LABORATORY TESTING
Nocturnal polysomnography is the gold standard for diagnosing obstructive sleep apnea. In this technique, multiple physiologic parameters are measured while the patient sleeps in a laboratory. Typical parameters in a sleep study include eye movement observations (to detect rapid-eye-movement sleep), an electroencephalogram (to determine arousals from sleep), chest wall monitors (to document respiratory movements), nasal and oral air flow measurements, an electrocardiogram, an electromyogram (to look for limb movements that cause arousals) and oximetry (to measure oxygen saturation). Apneic events can then be documented based on chest wall movement with no air flow and oxyhemoglobin desaturations.
Typically, a respiratory disturbance index (RDI) is calculated and expressed as the number of abnormal respiratory events per hour of sleep. Some sleep laboratories use an RDI of 20 episodes per hour as the cutoff point to consider continuous positive airway pressure (CPAP) treatment of obstructive sleep apnea, although the degree of symptoms is an important consideration regardless of the RDI. A multiple sleep latency test may also be performed to assess the level of daytime sleepiness.25 The average adult requires 10 or more minutes to fall asleep during the day. A mean sleep latency of less than 5 minutes is considered abnormal. More aggressive treatment of obstructive sleep apnea might be considered in a patient with a relatively low RDI who exhibits significant daytime sleepiness.
Unfortunately, laboratory sleep studies are expensive, with polysomnography costing $800 to $1,400. The multiple sleep latency test may add to this cost.
HOME TESTING
Home evaluation is sometimes used to screen patients for obstructive sleep apnea. Home studies are less expensive than laboratory testing and are certainly more convenient for patients. However, studies conducted in the home generally do not measure as many physiologic parameters as formal laboratory tests. Because no technician is present, it is not possible to adjust the equipment during the night if this becomes necessary.
Home studies may be useful in patients who have more severe sleep apnea with significant oxyhemoglobin desaturations that are easy to document with fewer parameters. Because severe apnea is often associated with significant arterial desaturation, it may be possible to use simple and inexpensive pulse oximetry as a screening method for the most severe disease.26
Overall, home evaluation is useful when the results are clearly positive. However, negative results do not rule out the presence of a sleep disorder. A recent report described successful complete polysomnography, including electro encephalographic sleep staging, that was performed in the homes of several patients.27
Medical Complications
Cardiovascular disease is common in patients with obstructive sleep apnea.28 Hypertension and obesity increase the risk of cardiac disease and are frequent findings in patients with this sleep disorder. Although hypertension is the best documented cardiovascular condition in obstructive sleep apnea, some studies have shown that patients with the disorder are also at increased risk for cardiac arrhythmias,4 including severe bradycardias, during apneic episodes. Furthermore, the prevalence of angina and myocardial infarction is increased in patients with apnea. Obstructive sleep apnea has been shown to cause dilated cardiomyopathy, which is reversible with successful treatment of the sleep disorder.29
Patients with sleep apnea who are smokers may also have coronary artery disease and obstructive airway disease. More severe oxyhemoglobin desaturations occur during apneic episodes in patients with both sleep apnea and chronic obstructive pulmonary disease. In some patients, repetitive severe nocturnal desaturations may lead to persistent pulmonary hypertension and right-sided heart failure (cor pulmonale).
Cerebrovascular diseases may also be more prevalent in patients with obstructive sleep apnea. One large population-based study found an increased incidence of cerebral infarction in patients with habitual snoring.30 Another study reported an increased number of strokes in patients who had obstructive sleep apnea.6
Psychosocial problems are common in patients who have sleep apnea. These patients often have depression, mood changes, poor memory, irritability and impaired concentration. Nocturnal panic attacks have also been associated with sleep apnea.31
Treatments
NONSURGICAL APPROACHES
Weight loss is the simplest treatment for obstructive sleep apnea in obese patients. Even a modest 10 percent weight loss may eliminate apneic episodes by reducing the mass of the posterior airway. Unfortunately, however, this treatment option is usually not successful because only a small fraction of people can permanently lose weight. Moreover, success may be limited if patients also have anatomic deficits in the jaw.
CPAP treatment is used in most patients who have obstructive sleep apnea. With CPAP, the patient wears a snugly fitting nasal mask attached to a fan that blows air into the nostrils to keep the airway open during sleep (Figure 9). Because most people sleep with their mouth closed, the mouth usually does not have to be covered, but a chin strap can be used if necessary.

Sneezing and rhinorrhea are mild but common complications of CPAP but can usually be alleviated with steroid nasal sprays. Some patients develop dry mucus membranes from the continuous positive air flow. This problem may be reduced by humidification. Another frequent problem is dermal irritation from the mask rubbing the face. Dermal irritation is most commonly reduced by changing the mask size or trying a different kind of mask.
Perhaps the biggest problem with CPAP therapy is noncompliance. Frequently, patients use the machine for only a few hours a night or a few days a week. Sneezing, nasal discharge and dryness sometimes result in noncompliance, but CPAP failure may also be caused by perceived discomfort, claustrophobia and panic attacks. Patients with more severe apnea and debilitating daytime sleepiness are often more compliant, because they are motivated by the prompt reversal of their symptoms. The cost of a CPAP machine is substantial (usually around $1,000) but is covered by most insurance carriers.
Tongue-retaining devices or bite guards can be used to bring the lower jaw forward and thereby alleviate posterior airway obstruction during sleep.32,33 These devices are not as consistently successful as CPAP treatment, but they may be useful in selected patients with mild sleep apnea who cannot tolerate CPAP13 or do not want to undergo surgery. Tongue-retaining devices may also be of some use in patients who snore heavily but do not have significant apnea.
An early study indicated that oxygen therapy was somewhat beneficial in reducing the frequency of apneic episodes and the incidence of apnea-induced bradycardia.34 These results were not borne out in later studies.
SURGICAL TREATMENTS
Younger patients and those who cannot tolerate CPAP may be candidates for surgical intervention to alleviate obstructive sleep apnea. Uvulopalatopharyngoplasty (UPPP) involves the removal of part of the soft palate, uvula and redundant peripharyngeal tissues, sometimes including the tonsils. This procedure is often effective in eliminating snoring; however, it is not necessarily curative for obstructive sleep apnea, because areas of the airway other than the soft palate also collapse in most patients with this sleep disorder. Patients who undergo UPPP must be hospitalized for a few days. Furthermore, they may experience the annoying complication of nasal regurgitation of liquids following the removal of palatal tissues.
Laser-assisted uvulopalatoplasty (LAUP) can be performed in a series of office treatments and thus has become more popular than UPPP in recent years. The clinical indications for this procedure, as well as its effectiveness, have not yet been clearly defined. Some sleep experts recommend the use of LAUP in patients who have snoring and mild apnea or patients who have no significant apnea but want to alleviate snoring.
Gastric surgery might be a consideration in some morbidly obese patients with obstructive sleep apnea.35 How weight loss causes a lessening of apnea is not clear, but it is presumably through a reduction in the adipose level of parapharyngeal tissues.
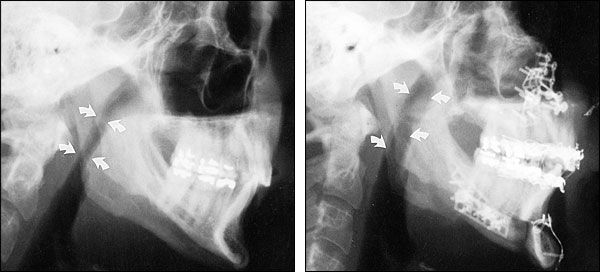
Jaw surgery is the most invasive surgical procedure used to treat obstructive sleep apnea.36 Patients who have a small, retrognathic mandible and have failed more conservative treatments may be candidates for this approach. The surgical procedure may be limited to pulling the tongue forward (genioplasty). An extensive procedure may entail moving both the mandible and maxilla. Extensive jaw surgery has a higher complication rate and a longer recovery time.
In noncompliant patients with extremely severe apnea, tracheostomy may be considered. Because of its high associated morbidity, this procedure is now seldom used.37