
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2000;61(4):1047-1052
See related patient information handout on Hashimoto's disease, written by the authors of this article.
Thyroiditis is a group of inflammatory thyroid disorders. Patients with chronic lymphocytic thyroiditis (also referred to as Hashimoto's thyroiditis) present with hypothyroidism, goiter, or both. Measurement of serum thyroid autoantibodies and thyroglobulin confirms the diagnosis. Subacute granulomatous thyroiditis (sometimes referred to as de Quervain's disease) is a self-limited but painful disorder of the thyroid. Physical examination, elevated erythrocyte sedimentation rate, elevated thyroglobulin level and depressed radioactive iodine uptake (RAIU) confirm the diagnosis. Subacute lymphocytic thyroiditis (silent thyroiditis) is considered autoimmune in origin and commonly occurs in the postpartum period. Symptoms of hyperthyroidism and depressed RAIU predominate. Acute (suppurative) thyroiditis is a rare, infectious thyroid disorder caused by bacteria and other microbes. The rare, invasive fibrous thyroiditis (Riedel's thyroiditis) presents with a slowly enlarging anterior neck mass that is sometimes confused with a malignancy.
Thyroiditis refers to a group of inflammatory diseases affecting the thyroid gland (Table 1). With the help of historical information, a physical examination and diagnostic tests, physicians can classify the type of thyroiditis and initiate appropriate treatment.
| Histologic classification | Synonyms |
|---|---|
| Chronic lymphocytic | Chronic lymphocytic thyroiditis, Hashimoto's thyroiditis |
| Subacute lymphocytic | Subacute lymphocytic thyroiditis: (1) postpartum thyroiditis and (2) sporadic painless thyroiditis |
| Granulomatous | Subacute granulomatous thyroiditis, de Quervain's thyroiditis |
| Microbial inflammatory | Suppurative thyroiditis, acute thyroiditis |
| Invasive fibrous | Riedel's struma, Riedel's thyroiditis |
Chronic Lymphocytic Thyroiditis
Chronic lymphocytic thyroiditis (Hashimoto's thyroiditis) is the most common inflammatory condition of the thyroid gland and the most common cause of goiter in the United States.1,2 It is an autoimmune condition characterized by high titers of circulating antibodies to thyroid peroxidase and thyroglobulin.3
EPIDEMIOLOGY
Chronic lymphocytic thyroiditis is the most common cause of hypothyroidism in the United States, and euthyroid persons with Hashimoto's disease develop hypothyroidism at a rate of approximately 5 percent per year.4 Up to 95 percent of cases of chronic lymphocytic thyroiditis occur in women, usually between 30 and 50 years of age.5 Chronic lymphocytic thyroiditis is also the most common cause of sporadic goiter in children.5,6 The incidence of Hashimoto's disease has risen exponentially over the past 50 years, and this increase may be related to an increased iodine content in the North American diet.6
A genetic predisposition to thyroid auto-immunity exists; it is inherited as a dominant trait.7 Hashimoto's disease has been linked to other autoimmune diseases, including systemic lupus erythematosus, rheumatoid arthritis, pernicious anemia, diabetes mellitus and Sjögren's syndrome.5 A rare but serious complication of chronic autoimmune thyroiditis is thyroid lymphoma.7 These lymphomas, generally the B-cell, non-Hodgkin's type, tend to occur in women 50 to 80 years of age and are usually limited to the thyroid gland.7
CLINICAL MANIFESTATIONS
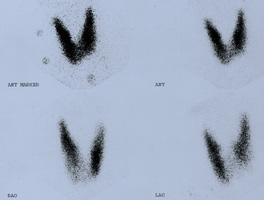
Although Hashimoto's thyroiditis is usually asymptomatic, some patients may complain of a feeling of tightness or fullness in the neck; however, neck pain and tenderness are rare6,7 (Figure 1). At the time of diagnosis, symptoms of hypothyroidism are present in 20 percent of patients.6 Physical examination generally reveals a firm, irregular, nontender goiter.7 The erythrocyte sedimentation rate (ESR) and white blood cell count are normal. The definitive indicator of chronic lymphocytic thyroiditis is the presence of thyroid-specific autoantibodies in the serum. The three main targets for thyroid antibodies are thyroglobulin (a protein carrier for thyroid hormones), thyroid microsomal antigen (also called thyroid peroxidase) and the thyroid-stimulating hormone (TSH) receptor.7 Low levels of circulating antibodies are common in other thyroid diseases, such as multinodular goiter and thyroid malignancy. Antithyroid microsomal antibodies in titers greater than 1:6,400 or antithyroid peroxidase antibodies in excess of 200 IU per mL, however, are strongly suggestive of chronic autoimmune thyroiditis.7 Testing of thyroid autoantibodies and measurement of serum thyroglobulin levels will confirm the diagnosis.7 Radioactive iodine uptake (RAIU) is variable and can be depressed, normal or increased, depending on the extent of follicular destruction (Figures 2a, 2b and 2c). Patchy uptake is common, providing little diagnostically useful information.7 Ultrasonography shows an enlarged gland with a diffusely hypoechogenic pattern in most patients.7 RAIU and thyroid ultrasonography are not necessary parts of the work-up for this disease. A dominant nodule in a patient with Hashimoto's disease should prompt a fine-needle aspiration biopsy to exclude malignancy.7

CLINICAL MANAGEMENT
[ corrected] Because thyroiditis is usually asymptomatic and the goiter is small, many patients do not require treatment.6 When hypothyroidism is present, treatment with thyroxine (T4) is indicated.7 Thyroid hormone replacement therapy is also indicated in patients with a TSH level in the normal range, to reduce goiter size and prevent progression to overt hypothyroidism in high-risk patients.7 Lifetime replacement of levothyroxine is indicated in hypothyroid patients, at a starting dosage of 25 to 50 μg per day, with gradual titration to an average daily dosage of 75 to 150 μg. A lower starting dosage (12.5 to 25 μg per day) and a more gradual titration are recommended in elderly patients and in patients with cardiovascular disease. The dosage may be increased in these patients 25 to 50 μg every four to six weeks until the TSH level is normal.6,7
In patients with an elevated TSH level and a normal thyroxine (T4) level (subclinical hypothyroidism), indications for treatment are less clear. If the TSH level is greater than 20 mU per mL (20 mU per L) with a normal T4 level, there is a high probability that the patient will develop hypothyroidism. If the TSH level is elevated but is less than 20 mU per mL and the antimicrosomal antibody titer is greater than 1:1,600, hypothyroidism will develop in 80 percent of patients.5 Therefore, it is recommended that treatment be initiated in patients with symptoms of hypothyroidism, in patients with a serum TSH level greater than 10 mU per mL (10 mU per L) and in patients with a high risk of progression to hypothyroidism (e.g., those with high antibody titers).7 Because of the risk of developing hypothyroidism, patients with a history of chronic lymphocytic thyroiditis require annual assessment of thyroid function.6
Subacute Lymphocytic Thyroiditis
Subacute lymphocytic thyroiditis occurs most often in the postpartum period but may also occur sporadically.7 Therefore, it is subdivided into two groups, postpartum thyroiditis and sporadic painless thyroiditis. Antimicrosomal antibodies are present in 50 to 80 percent of patients, while antithyroid peroxidase antibodies are present in nearly all patients.3,6,7 Subacute lymphocytic thyroiditis starts with an initial hyperthyroid phase, followed by subsequent hypothyroidism and, finally, a return to the euthyroid state. In the postpartum patient, thyrotoxicosis usually develops in the first three months following delivery and lasts for one or two months. Then the patient returns to a euthyroid state or hyperthyroidism ensues for several months.8 Patients with an initial episode of postpartum subacute lymphocytic thyroiditis have a notably high risk of recurrence in subsequent pregnancies.1,6,9 Serum TSH testing is indicated in symptomatic patients.
EPIDEMIOLOGY
Subacute lymphocytic thyroiditis comprises 29 to 50 percent of all cases of thyroiditis3 and occurs most often in women between 30 and 50 years of age.6,9 There is a higher incidence of antimicrosomal antibodies in the postpartum form (80 percent) of the disease than in the sporadic form (50 percent). A family history of autoimmune thyroid disease is found in 50 percent of patients with the postpartum form of thyroiditis. The severity of the hypothyroid phase correlates directly with the antimicrosomal antibody titer. A titer of 1:1,600 or greater early in pregnancy is associated with a high risk of postpartum hypothyroidism.10 Approximately 6 percent of patients who have the postpartum form develop chronic hypothyroidism.6
CLINICAL MANIFESTATIONS
Patients usually present with acute symptoms of hyperthyroidism, such as tachycardia, palpitations, heat intolerance, nervousness and weight loss.6,9 A small painless goiter is present in 50 percent of patients.6–9 The ESR and white blood cell count are normal. T4 and triiodothyronine (T3) levels are initially elevated, with a disproportionate increase in T4 compared with T3.9 RAIU is decreased in the hyperthyroid phase of the disease and is almost always less than 3 percent. This situation contrasts markedly with the elevated RAIU found in patients with Graves' disease.3,5,8,9
CLINICAL MANAGEMENT
Acute symptoms of hyperthyroidism are managed primarily with beta blockers.3,6,7,9 Antithyroid drugs, which inhibit the production of new T4, are not indicated in the management of patients with hyperthyroidism because symptoms are caused by the release of preformed T3 and T4 from the damaged gland.6,9 Replacement of thyroid hormone in the hypothyroid phase is indicated if the patient's symptoms are severe or of long duration.7 If the hypothyroid phase lasts longer than six months, permanent hypothyroidism is likely.11
SUBACUTE GRANULOMATOUS THYROIDITIS
Subacute granulomatous thyroiditis is the most common cause of a painful thyroid gland7 (Figure 3). It is most likely caused by a viral infection and is generally preceded by an upper respiratory tract infection.7 Numerous etiologic agents have been implicated, including mumps virus, echovirus, coxsackievirus, Epstein-Barr virus, influenza and adenovirus.3,7
EPIDEMIOLOGY
CLINICAL MANIFESTATIONS
Subacute granulomatous thyroiditis presents clinically with acute onset of pain in the thyroid region. The pain may be exacerbated by turning the head or swallowing, and may radiate to the jaw, ear or chest.3,5,6 Symptoms of hypermetabolism may be present, and the ESR usually is markedly elevated.6,7 A normal ESR essentially rules out the diagnosis of subacute granulomatous thyroiditis.7 The thyroid is firm, nodular and exquisitely tender to palpation. The leukocyte count is normal or slightly elevated.7 Thyrotoxicosis is present in 50 percent of patients in the acute phase, and the serum T4 concentration is disproportionately elevated relative to the T3 level.7 Serum TSH concentrations are low to undetectable.7 Thyroglobulin is elevated. A normal thyroglobulin level essentially rules out the diagnosis of subacute granulomatous thyroiditis.6 The RAIU is notably low, often less than 2 percent at 24 hours.7 In summary, the physical examination, an elevated ESR, an elevated thyroglobulin level and a depressed RAIU confirm the diagnosis.
CLINICAL MANAGEMENT
The natural history of subacute granulomatous thyroiditis involves four phases that generally unfold over four to six months. The acute phase of thyroid pain and thyrotoxicosis may last three to six weeks or longer. Transient asymptomatic euthyroidism follows. Hypothyroidism often ensues and may last weeks to months or may be permanent (in up to 5 percent of patients).5 The final phase is a recovery period, during which thyroid function tests normalize.
Therapy with antithyroid drugs is not indicated in patients with subacute granulomatous thyroiditis because this disorder is caused by the release of preformed thyroid hormone rather than synthesis of new T3 and T4.6,7 Therapy with beta blockers may be indicated for the symptomatic treatment of thyrotoxicosis. Nonsteroidal anti-inflammatory drugs are generally effective in reducing thyroid pain in patients with mild cases. Patients with more severe disease require a tapering dosage of prednisone (20 to 40 mg per day) given over two to four weeks.3 Up to 20 percent of patients experience the recurrence of thyroid pain on discontinuation of prednisone.7 RAIU can assist clinicians in determining patients at high risk for relapse. Low RAIU uptake implies ongoing inflammation, and steroid therapy should be continued.3
Microbial Inflammatory Thyroiditis
Microbial inflammatory thyroiditis, also known as acute suppurative thyroiditis, is a rare subtype most often caused by the presence of Gram-positive bacteria in the thyroid gland. Staphylococcus aureus is the most common infectious agent,7 but other organisms have also been implicated (Figure 3). This disorder is rare because of the inherent resistance of the thyroid gland to infection. Microbial inflammatory thyroiditis occurs most often in women 20 to 40 years of age.5,9 Most patients have a preexisting thyroid disorder, usually nodular goiter.3,5,9 Anterior neck pain and tenderness are common. Other clinical features include fever, pharyngitis and dermal erythema.5,9 The pain is typically worse during swallowing and radiates locally.5,9,12 Tachycardia is common, along with leukocytosis and an elevated ESR level.3,5,9,12 TSH, T4 and T3 levels are typically normal, while RAIU may be normal or show cold nodules in areas of abscess formation.5,9,13 The cause of infection is first determined by culture and sensitivity of samples obtained through fine-needle aspiration.
When the cause of the infection is determined, appropriate parenteral antibiotics should be prescribed.5,9,12 Patients with abscesses require surgical drainage and, possibly, a thyroid lobectomy.5,9,12 Heat, rest and aspirin provide symptomatic relief; steroids may offer additional benefit.13 The disease is usually self-limited, lasting weeks to months.13
Invasive Fibrous Thyroiditis
First described by Riedel in 1898, this remains the rarest type of thyroiditis. In addition to the development of dense fibrosis of the thyroid gland itself, extracervical sites of fibrosis frequently occur as inflammatory fibrosclerotic processes, including sclerosing cholangitis, retroperitoneal fibrosis and orbital pseudotumor.9,14,15 Studies suggest that one third of patients with fibrous thyroiditis develop multifocal fibrosclerosis.14,16 The mean age at presentation is 47.8 years, and 83 percent of all cases occur in females.16 A stone-hard or woody mass that extends from the thyroid is common.9,14–16 Symptoms vary according to the structures involved and most commonly result from a thyroid mass that produces dyspnea, dysphagia and, occasionally, stridor.9,12,14,16 The thyroid mass may grow suddenly or slowly, and is usually unilateral.14
RAIU is decreased in affected areas of the gland.12,15 Most patients remain euthyroid, and the ESR is frequently elevated.5,9,14,16 Thyroid autoantibodies are present in appreciable quantities in 45 percent of patients.5,9,14,16 Because of the similarity between fibrous thyroiditis and thyroid carcinoma, diagnosis must be made using open biopsy.5,9,12,14 The disease is usually self-limited, with surgical wedge resection of the thyroid isthmus being the mainstay of treatment in symptomatic patients.5,9,12,14
| Subtype | Etiology | Neck pain | RAIU | TSH | T4 | Thyroid autoantibodies |
|---|---|---|---|---|---|---|
| Chronic lymphocytic (Hashimoto's disease) | Autoimmune | No | Variable | Variable | Variable | Present |
| Subacute granulomatous | Viral | Yes | Decreased | Decreased | Increased | Absent |
| Subacute lymphocytic | Autoimmune | No | Decreased | Decreased | Increased | Present |
| Microbial inflammatory | Bacterial, fungal, parasitic | Yes | Variable | Normal | Normal | Absent |
| Hashitoxicosis | Autoimmune | No | Decreased | Decreased | Increased | Present |
| Invasive fibrous | Unknown | No | Variable | Normal | Normal | Variable |
Final Comment
Thyroiditis is a heterogeneous disease with several subtypes. These subtypes mimic other diseases as well as each other. Differentiation of the subtypes of thyroiditis requires an understanding of their unique clinical presentations, radiologic studies, laboratory data and indications for pharmacotherapy (Table 1).