
Am Fam Physician. 2004;69(4):865-872
An examination of the feet is an essential component of an evaluation of a newborn. A thorough examination can be performed quickly. Despite its small size, the newborn foot is a complex structure. Most deformities can be diagnosed easily with physical examination alone, using few diagnostic studies. A thorough examination includes assessment of vascular, dermatologic, and neurologic status of the lower extremities, and observation, palpation, and evaluation of joint range of motion in both feet. Common newborn foot abnormalities include metatarsus adductus, clubfoot deformity, calcaneovalgus (flexible flatfoot), congenital vertical talus (rigid flatfoot), and multiple digital deformities—polydactyly, syndactyly, overlapping toes, and amniotic bands. Most treatments include conservative measures, such as observation, stretching, and splinting, which can be performed easily in the family medicine setting. Cases that require surgical correction should be referred to a subspecialist with expertise in correcting lower extremity deformities in children. When surgery is indicated, procedures generally are postponed for six to nine months so that the child will better tolerate anesthesia.
The examination of the feet is an essential component of a comprehensive evaluation of a newborn. With proper skills, this examination, which often is reassuring to new parents, can be performed quickly, yet thoroughly. Early detection of foot problems in infants allows timely corrective treatment, if required.
| Feature | Newborn | Adult |
|---|---|---|
| Arch | Flatter, less defined | Usually well defined, except in pes planus |
| Typical joint range of motion | Greater range of motion | Lesser range of motion |
| End point of range of motion | Soft, subtle, difficult to appreciate | Firm, well defined |
| Amount of subcutaneous fat tissue | Greater | Lesser |
Examination Techniques
Despite its small size, the newborn foot is complex, consisting of 26 to 28 bones. The foot can be divided into three anatomic regions (Figure 1): the hindfoot or rearfoot (talus and calcaneus); the midfoot (navicular bone, cuboid bone, and three cuneiform bones); and the forefoot (metatarsals and phalanges). Differences between a newborn foot and an adult foot are summarized in Table 1.
Simultaneous observation of both feet can reveal many deformities. The skin should be examined for unusual creases or folds that can be formed by various foot deviations. Certain areas of the skin might be abnormally taut, indicating extra tension on the skin, while the skin on the opposite side of the foot might reveal loose, excessive skinfolds.
During the next part of the examination, various foot and ankle joints are moved through their respective ranges of motion. The joints should be assessed for flexibility or rigidity, unusual positions, lack of motion, and asymmetry.
Finally, the vascular examination consists of assessment of capillary refill and skin color, because pulses are difficult to palpate. Fortunately, the majority of newborns exhibit excellent lower extremity vascular supply, unless it is compromised by an extrinsic factor, such as an intrauterine amniotic band.

Common Foot Abnormalities
METATARSUS ADDUCTUS
On inspection, the toes angle abruptly toward the midline, creating a C-shaped lateral foot border with a prominent styloid process of the fifth metatarsal.2 (Figures 3a and 3b). A splay can appear between the great and second toes. Skin examination frequently reveals a deep skin cleft at the medial midfoot.

A simple test that can raise the clinician's suspicions of MTA is the “V”-finger test (Figure 4). In this test, the heel of the foot is placed in the “V” formed by the index and middle fingers, and the lateral aspect of the foot is observed from a plantar side for medial or lateral deviation from the middle finger. Medial deviation from the middle finger at the styloid process indicates MTA.3
Treatment is based on the severity of the condition and is controversial. While some authors1 advocate only observation without active intervention for mild cases, others would intervene early in all severe cases or by two months of age, if the condition is not resolved.4 Other authors3 recommend treatment as soon as possible, especially in moderate to severe cases. Based on the natural course of the condition, a more conservative approach seems reasonable. Of MTA cases identified at birth, 85 to 90 percent resolve by one year of age.1,3 Another prospective study5 confirmed these findings—87 percent of MTA cases had resolved by six years of age, with only about 4 percent remaining at age 16.

Mild (flexible, passively correctable) MTA requires only parental reassurance. Moderate (semi-flexible, reducible) MTA can be treated with stretching exercises at every diaper change. First, the heel is stabilized within the notch between the thumb and index finger. Then, the forefoot is slightly pulled distally, held between the thumb and index finger of the other hand, and gently pushed into a corrected position.1
For the majority of MTA cases, the prognosis is quite good. In severe cases, excessive compensation at the level of the mediotarsal joint can lead to the development of bunions, hammertoes, and other disorders.6 Therefore, severe (rigid) MTA can be referred for serial casting and bracing. Evidence-based comparisons of splinting or casting versus manipulation alone are not yet available.4
CLUBFOOT
Clubfoot, or talipes equinovarus, is a congenital deformity that typically has four main components: inversion and adduction of the forefoot; inversion of the heel and hindfoot; equinus (limitation of extension) of the ankle and subtalar joint; and internal rotation of the leg.

Clubfoot is a complex, multifactorial deformity with genetic and intrauterine factors. One popular theory postulates that a clubfoot is a result of intrauterine maldevelopment of the talus that leads to adduction and plantarflexion of the foot.7 Clubfoot occurs in one to two per 1,000 live births; however, the incidence is higher in Hispanics and lower in Asians.8
On inspection, the “down and in” appearance of the foot, which somewhat resembles that of MTA, is obvious (Figure 5).3 The foot appears smaller, with a flexible, softer heel because of the hypoplastic calcaneus. The medial border of the foot is concave with a deep medial skin furrow, and the lateral border is highly convex. The heel is usually small and is internally rotated, making the soles of the feet face each other in cases of bilateral deformities.


Clubfoot can be classified into extrinsic (supple) type, which is essentially a severe positional or soft tissue deformity; and intrinsic (rigid) type, where manual reduction is impossible. The type of clubfoot determines the specific therapy. Extrinsic clubfoot can be treated by serial casting, while intrinsic clubfoot eventually may require surgery. Plaster casting should be attempted on virtually all clubfeet, supple or rigid, as soon as practical. Casts initially are changed at semiweekly to weekly intervals and are continued until the deformity responds and is corrected fully. Persistent cast treatments by experienced clinicians have been reported to be successful in most patients.9 However, if a plateau is reached in treatment, surgery by a specialist in pediatric foot deformities should be considered, usually when the child is between six and nine months of age.10 The goal is to obtain a stable, “platform-like” position of the foot for future ambulation.
CALCANEOVALGUS
The axis of calcaneovalgus deformity is in the tibiotalar joint, where the foot is positioned in extreme hyperextension, with its dorsum frequently touching the distal leg. Females are affected more often than males, and this deformity can be unilateral or bilateral.3 It occurs in about 5 percent of all newborns5 and is associated with external rotation of the calcaneus, an overstretched Achilles tendon, and tight anterior leg musculature, all of which warrant treatment.11

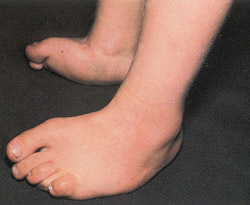
On inspection, the foot has an “up and out” appearance, with the dorsal forefoot practically touching the anterior aspect of the ankle and lower leg (Figure 8). The ankle generally can be plantarflexed to only 90 degrees or less. Radiographs can confirm clinical diagnosis.
Calcaneovalgus is a positional deformity that is highly amenable to treatment. According to some authors,10,12 it has an excellent natural history and can spontaneously resolve on its own. Others3 advocate a more aggressive approach because of the possibility of future complications, such as permanent muscle imbalance, peroneal tendon dislocation, and delayed ambulation. Generally, the more severe the limitation of ankle plantar flexion, the more treatment is warranted.
Treatment should begin as early as possible. Mild cases can be treated with stretching exercises performed at each diaper change. Stretching consists of gentle plantarflexion of the foot with mild inversion for a count of 10, repeated three times. In moderate cases or when stretching fails to correct the deformity, splinting or firm, high-top, lace-up shoes that prevent dorsiflexion can be used. For severe deformities with significant limitation of ankle plantarflexion, serial mobilization casting is performed until corrected, followed by nightly maintenance use of a bivalved cast or splinting of the posterior aspect of the leg for a two- to 10-week course.3
CONGENITAL VERTICAL TALUS
Congenital vertical talus is a rare deformity that must be distinguished from calcaneovalgus. Otherwise known as rocker-bottom foot, it is a rigid deformity, as opposed to a flexible calcaneovalgus foot, so it does not respond to stretching and, in most cases, requires surgery.
The hindfoot is in equinus rather than calcaneus position, with talus and calcaneus pointing downward and the forefoot dorsiflexed. This results in dislocation of the midtarsal bones on the head and neck of the talus.11
It is important to examine the entire child, looking for other abnormalities, such as arthrogryposis (multiple joint contractures present at birth) and meningomyelocele, which might be present in up to 60 percent of children with congenital vertical talus.10,13 The foot examination usually reveals a rigid foot with a “reversed” arch, a convex plantar surface, and a deep crease on the lateral dorsal side of the foot. The ankle joint is plantarflexed, while the midfoot and forefoot are extended upward (Figure 9). Lateral foot radiographs are helpful in confirming the diagnosis.
Conservative therapy can assist in stretching the forefoot and hindfoot, but surgery is needed in most cases. Surgery is complex, requiring correction in all three cardinal planes, and should be performed by a specialist in pediatric foot deformities.
Digital Deformities
Polydactyly
The incidence of polydactyly (supernumerary digits of hands or feet) is the same in both sexes, with simultaneous polydactyly of the hands and feet present in about one third of cases.14 It is more common in blacks than whites (3.6 to 13 cases per 1,000 live births versus 0.3 to 1.3 cases per 1,000 live births, respectively).15
The primary cause of polydactyly is thought to be genetic. Polydactyly usually involves border digits, especially the fifth. Although some cases involve only a distal phalanx, other cases are much more complex, involving the entire digit, with duplication of nails, tendons, and vascular structures.
Treatment of complex cases involving bone requires removal of duplicated structures, whereas cases involving soft tissue can be treated with only ligation sutures applied in the nursery. Surgery generally is performed at six to nine months of age, before the child is ambulatory but able to tolerate general anesthesia.10,15
Syndactyly
Syndactyly (webbed toes or fingers) occurs in approximately one in 2,000 to 2,500 live births.15 There are various levels of syndactylization, from partial to complete. The most frequent site is between the second and third toes. Syndactyly is thought to be genetic, with an autosomal dominant pattern of inheritance.
Simple syndactyly is more of a cosmetic problem than a functional one, and rarely requires treatment.10 A radiographic evaluation is not indicated unless radical treatment is being contemplated. If the parents desire surgery, it is advisable to wait until the child is old enough to take part in the decision and participate in postoperative care. The most common complication of the surgery is skin-flap slough, leading to a recurrence of the problem.
Overlapping Toes
Overlapping toes are often familial, with the fifth toe being the most commonly affected. Frequently bilateral, the condition is distributed evenly between boys and girls. This deformity presents as adduction of the little toe with some external rotation of the digit. The metatarsophalangeal joint is dorsiflexed, and the nail plate is frequently smaller than expected.15
In newborns, the condition is frequently passively correctable with gentle stretching or use of various toe spacers. Nighttime paper-tape splinting to the adjacent toe has been empirically recommended, but this method lacks evidence-based outcome studies.16 However, if a child starts to walk before the deformity is corrected, it can become rigid, causing symptoms, and can require surgical correction.13
Amniotic (Annular) Bands
Amniotic bands commonly involve toes and fingers. Occurring in one in 15,000 live births, they are produced by thin bands of amniotic membrane wrapping around various parts of the extremity in utero.15 Simple bands create swelling of the distal part of the toe with concomitant lymphedema, and deeper bands can produce complete amputations.17
Contractions and resultant bulbous ends of the involved digits are seen easily during examination. In addition to lymphedema, it is essential to rule out vascular compromise, which is manifested by pale, cool skin with delayed capillary refill.
| Condition | Major features | Treatment approach |
|---|---|---|
| Metatarsus adductus | C-shaped lateral foot border | Mild: observation |
| Prominent styloid process of fifth metatarsal | Moderate: stretching exercises | |
| Splay between the great and second toes | Severe: casting, bracing | |
| “V”-finger test deviation of lateral foot border | ||
| Clubfoot (talipes equinovarus) | “Down and in” foot appearance | Extrinsic (supple): serial castings, followed by maintenance splinting |
| Small atrophic heel, rotated internally | Intrinsic (rigid): initial casting, usually followed by surgical correction | |
| Concave medial foot border, convex lateral | ||
| Deep medial skin furrow | ||
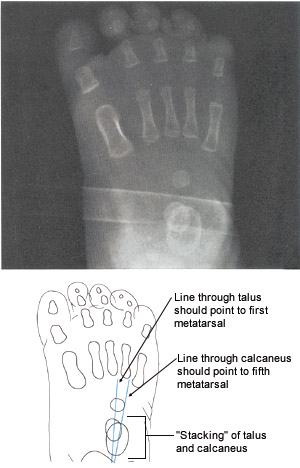
| Radiographs show parallel axes of talus and calcaneus | ||
| Calcaneovalgus | “Up and out” foot appearance | Mild: stretching exercises |
| Foot in extreme dorsiflexion (hyperextension) | Moderate: splinting and high-top, rigid-sole, lace-up shoes | |
| Externally rotated heel | Severe: serial castings, followed by nightly splinting or bivalved casting | |
| Dorsal forefoot can be touching outer leg | ||
| Congenital vertical talus (rocker-bottom foot) | Rigid foot appearance with “reversed” arch | Initial conservative therapy to stretch soft tissues, followed by surgical correction |
| Plantarflexed ankle joint with upwardly extended midfoot and forefoot | ||
| Need lateral foot radiograph to confirm | ||
| Polydactyly (supernumerary digits) | Usually involves border toes, most commonly the fifth | Surgical: ligation suture (less complex); removal of duplicated structures (more complex) |
| Could present as partial (i.e., two nail plates) or complete digit duplication | ||
| No radiographs needed unless surgery is being contemplated | ||
| Syndactyly (webbed toes) | Most commonly affects second and third toes | Problem is more cosmetic, rarely requires treatment |
| Various levels of webbing, from partial to complete | If surgery is desired, it should be postponed until child is old enough to take part in the decision | |
| Overlapping toes | Usually fifth toe over fourth toe | Stretching, use of silicone toe spacers, taping |
| Frequently bilateral | Surgical correction in older children, if symptomatic | |
| Adduction and external rotation of the little toe, dorsiflexed digit | ||
| Smaller nail plate | ||
| Amniotic (annular) bands | Constriction bands over various parts of extremity | Simple bands are cosmetic problems and do not require treatment |
| Can lead to vascular compromise, lymphedema | Complex bands require surgical release, especially if neurovascular compromise is present | |
| Deeper bands can produce complete amputations |