
Am Fam Physician. 2008;78(3):347-352
Author disclosure: Nothing to disclose.
Hematuria, symptomatic and incidental, that involves more than three red blood cells per high-power field on two of three properly collected urinalysis specimens warrants some type of imaging to evaluate the upper tracts. Traditionally, excretory urography or the intravenous pyelogram has been the mainstay of the hematuria work-up, but computed tomography urography has more recently been recognized to have significant advantages. Multidetector computed tomography urography, a cross-sectional technique, is less susceptible to overlying bowel gas and more sensitive for detection of small tumors and calculi. Moreover, intravenous-pyelogram–like images can be obtained by using reconstruction techniques. In specific cases, ultrasound examination and magnetic resonance imaging can also be useful, and are particularly helpful in children and pregnant women. Neither modality has the sensitivity of computed tomography for calculi, but small tumors may be visible on magnetic resonance imaging. This article reviews the appropriateness criteria for the various radiologic imaging tests used in the evaluation of hematuria, as proposed by the American College of Radiology.
Hematuria is one of the most common presentations of patients with urinary tract diseases; therefore, it is a common reason for urinary tract imaging. The most appropriate imaging for adult patients presenting with hematuria as a symptom is reviewed in this article, based on the Appropriateness Criteria from the American College of Radiology. The American Urologic Association (AUA) has previously published guidelines regarding the use of imaging in asymptomatic hematuria.1,2 The AUA guidelines recommended upper tract imaging for low- and high-risk patients with microscopic hematuria, defined as three or more red blood cells per high-power field from two of three properly collected urinalysis specimens. Patients whose urinary tracts have no detectable pathology normally release small amounts of blood into urine, so that one or two red cells per high-power field may normally be visible upon microscopic examination of the spun sediment. This fact, together with the low prevalence of clinically detectable disease in patients with asymptomatic microscopic hematuria, has led investigators to suggest that such minimal microhematuria in an asymptomatic young adult needs no evaluation.3
Gross hematuria clearly conveys a much higher risk of malignancy than microscopic disease and should be thoroughly evaluated,4,5 but virtually all cases of hematuria as defined by AUA guidelines need a complete work-up. It is clear that hematuria of any degree can be associated with significant urinary tract pathology. Other diagnostic modalities, including cytology, cystoscopy, and renal biopsy may be appropriate in the work-up of hematuria, but are beyond the scope of this article.1,2
Illustrative Case
A 69-year-old man with a long history of smoking presented with gross hematuria. An excretory urogram (intravenous pyelogram) demonstrated a radiolucent filling defect in the distal left ureter (Figure 1A). Transaxial computed tomography (CT) during the excretory phase of enhancement revealed a soft-tissue–filling defect in the left ureter (Figure 1B). A curved reformatted image was obtained from the excretory-phase enhanced transaxial CT urography and showed that the polypoid filling defect has a stalk, an additional small polypoid ureteral filling defect was present, and there was a defect near the ureteric insertion into the bladder (Figure 1C).
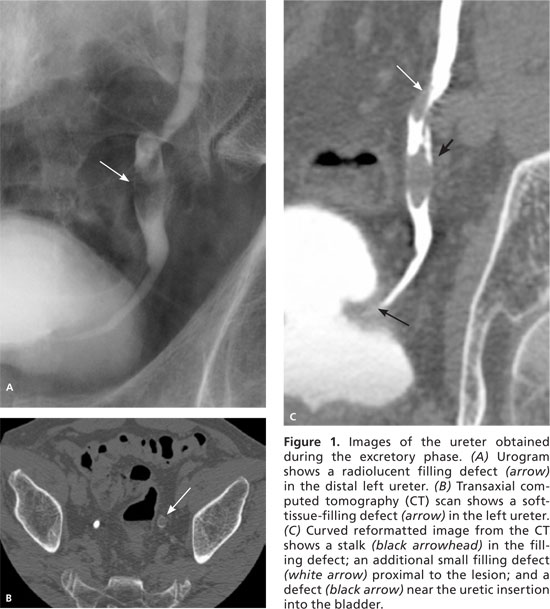
The patient underwent a left distal ureterectomy with a left ureteroneocystostomy. The tumors were noninvasive grade 2 (of 3) papillary urothelial carcinomas (transitional cell carcinoma). The bladder lesions were also noninvasive grade 2 (of 3) papillary urothelial carcinomas and were treated with fulguration.
Must Imaging Always Be Performed?
There may be specific circumstances in which a complete radiologic work-up is not necessary.6 Young women with a clinical picture of simple cystitis and whose hematuria completely and permanently resolves after successful therapy will probably not require any imaging.7,8 Patients who have clear-cut evidence of glomerulopathy also constitute a special group—chest radiography 8 to search for any of the numerous manifestations of glomerulonephritis (including cardiac enlargement, pleural and pericardial effusions, pulmonary congestion and edema, and pulmonary bleeding) and ultrasonography (to display the site and number of kidneys before biopsy and to screen for renal morphologic abnormalities that may coexist by chance in a patient with glomerulonephritis) should be obtained.9–13 However, the decision to pursue this course requires firm demonstration that the glomerular abnormality is responsible for the hematuria; such evidence includes heavy proteinuria (sufficient to indicate that plasma proteins, rather than proteins in red cells, account for the protein in the urine), red cell casts, or evidence of severe red cell dysmorphism (only given reliable methods of identifying such abnormalities).
| Radiologic examination procedure | Appropriateness rating | Comments |
|---|---|---|
| Multidetector CT urography | 8 | This is becoming the method of choice for hematuria, supplanting intravenous pyelography, even though their appropriateness ratings are the same |
| Radiography, intravenous urography (intravenous pyelogram, excretory urography) | 8 | — |
| Ultrasonography, kidney and bladder, transabdominal | 6 | May miss ureteral and urothelial lesions; abdominal radiography, retrograde pyelography, and cystoscopy are useful adjuncts |
| Radiography, retrograde urography | 5 | — |
| MRI urography | 4 | — |
| CT, abdomen and pelvis | 4 | CT may follow intravenous pyelogram or ultrasonography if initial findings are ambiguous |
| Kidney, angiography | 4 | Rarely, vascular malformations may cause hematuria and require angiography for diagnosis |
| Radiography, abdomen, KUB | 2 | It is assumed that a plain film of the abdomen will be part of the indicated intravenous pyelogram; if an intravenous pyelogram is not performed, KUB may be performed with ultrasonography |
| MRI, abdomen, and pelvis | 2 | — |
| Urinary tract scintigraphy | 2 | — |
| Virtual cystoscopy | 2 | — |
Radiologic Work-up of Hematuria
Radiologic evaluation will almost always be accompanied by cystoscopy because many bleeding urinary tract lesions arise in the bladder and lower urinary tract, and no imaging technique is completely satisfactory for ruling out disease at these sites.2 A complete history, physical examination, urinalysis, and appropriate blood tests should precede or accompany the imaging examinations. At the time of cystoscopy, bilateral retrograde pyelography (in which iodinated contrast is injected through catheters placed in the ureters during cystoscopy and plain radiographs are obtained) is often employed to evaluate the upper tracts for pathology.6
There is no universal agreement about the optimal imaging work-up of hematuria. Traditionally, excretory urography (intravenous pyelogram) was the standard,6–8 but the establishment of this practice preceded the development of high-quality ultrasonography,17 CT, and magnetic resonance imaging (MRI). Recently, multidetector CT scans, in which each rotation of the radiography beam produces multiple sets of images instead of just one set, have become routine. They provide cross-sectional images and can be reformatted to demonstrate the urinary tract in a manner similar to traditional intravenous pyelograms. Similarly, MRI can be used to detect urinary tract abnormalities, but has limited use because of its expense and the lack of data supporting its use.
Increasing Role of CT Urography
Conventional abdominal CT of the entire urinary tract can be augmented by delayed thin-section images of the contrast-opacified collecting systems, ureters, and bladder 18; the combined examination is known as CT urography. The intravenous-pyelogram–like portions of the examination may be obtained by exposing film (or direct digital) images when intravenous contrast, previously administered for the CT, has opacified the urinary tract. Intravenous-pyelogram–like images may alternatively be produced by reformatting delayed CT images in the coronal or sagittal planes. Presumably, the pyelogram portion of this examination could be comparable with a standard intravenous pyelogram examination, making CT more sensitive and specific (statistically and pathologically) than ultrasonography or nephrotomography with regard to focal renal parenchymal abnormalities.
Nephrotomography is an older technique, used before the invention of CT, which images 1-cm coronal sections of the kidneys as part of an intravenous pyelogram. Thus, a distinction should be made between a routine CT of the abdomen and pelvis that may not be optimized for the urinary tract and a dedicated CT urogram that is tailored to evaluate the urinary tract for sources of hematuria. The latter study typically employs oral water instead of oral positive contrast media, as this will greatly aid the reconstruction of images.
In the CT urogram, all patients receive water, primarily to hydrate the kidneys and distend the collecting system and ureter. Next, a noncontrast helical CT of the kidneys is obtained to evaluate renal calculi. This is followed by the injection of iodinated contrast media with the acquisition of a high-resolution (1- to 2-mm sections) nephrographic phase and a high-resolution delayed (five to 10 minutes) phase to evaluate for tumors and filling defects. The latter can be reconstructed to evaluate the urinary tract and bladder. Some investigators employ a hybrid of CT urography and intravenous-pyelogram–like delayed images to form one complete study, which is also known as CT urography and has shown equal or superior sensitivity to intravenous pyelogram for causes of hematuria.19,20
Virtual cystoscopy—the acquisition of high-resolution CT images reconstructed to allow virtual “fly-throughs” of the bladder—can be used to evaluate the bladder for causes of hematuria.21 Virtual cystoscopy is inaccurate for small lesions and lesions located near the ureteric orifices. The urethra cannot be evaluated, so virtual cystoscopy cannot replace actual cystoscopy.
Role of Ultrasonography and MRI
There is some support for the use of ultrasonography as the initial imaging study for selected patients with hematuria.17,22,23 Ultrasonography is believed to have moderately high sensitivity with respect to the wide range of abnormalities that may be encountered, including urinary tract neoplasms of all sorts, stone disease, inflammatory processes, congenital abnormalities, vascular lesions, and obstruction from a wide variety of lesions.5,22–24 Nevertheless, it appears that ultrasonography has similar rates of detection compared with excretory urography (intravenous pyelogram) for diagnosing clinically important lesions.25 Ultrasonography and urography tend to miss different sorts of lesions, and ultrasonography is not likely to detect nonobstructing ureteral stones or small urothelial abnormalities, whereas urography with nephrotomography may miss small exophytic anterior and posterior renal masses and small bladder lesions.26,27
The choice of examination may be affected by clinical circumstances (e.g., a positive urinary cytologic analysis may make urography crucial, whereas serious risk factors for contrast reactions may make ultrasonography more appropriate). When ultrasonography is negative and the source of hematuria remains obscure, urography should be added; if urography is negative, CT may be ordered.8,27,28 When ultrasonography is used as the primary screening modality, the yield from imaging may be increased by adding a plain film of the abdomen. Ultrasonography has a particularly important role in children and pregnant women with hematuria, in whom ionizing radiation must be avoided.
MRI urography currently serves as an alternative imaging technique for children and pregnant women and for patients with a contraindication to iodinated contrast media.29 It has the potential to be useful in the search for important abnormalities (e.g., urothelial cancers, stones, renal tumors) that cause hematuria. MRI urography has not been widely adopted in clinical practice, is expensive, and has not been evaluated for effectiveness, so it cannot be recommended as an initial examination.
Final Comments
Most adults with hematuria require urinary tract imaging. Intravenous pyelogram and CT urography represent the leading techniques, with an increasing trend for the latter. Ultrasonography and MRI have secondary roles in selected populations. Carefully selected patients may require no further work-up if their clinical history can reasonably determine the cause of their hematuria (Table 230 ).
| Causes of hematuria in adults* |
| Calculi |
| Infection |
| Cancer (bladder, kidney, prostate, urothelial) |
| Obstruction |
| Bleeding diathesis |
| Anticoagulation |
| Antibiotics (rifampin [Rifadin]) |
| Diabetes |
| Hypertension |
| Sickle cell anemia |
| Chronic renal disease |
| Congenital |
| Vascular malformations and aneurysms |
| Artifactual causes of hematuria |
| Food (e.g., beets, berries, rhubarb) |
| Food coloring |
| Medications |
| Menstrual blood |