
A more recent article on vaginitis is available.
Am Fam Physician. 2011;83(7):807-815
Related letter: Conventional vs. Liquid-Based Cytology Pap Smears for Diagnosing Trichomoniasis
Patient information: See related handout on vaginitis, written by the authors of this article.
Author disclosure: Dr. Hainer is on the speaker's bureau for Merck and Sanofi Pasteur regarding immunizations, but has no financial disclosure relevant to the topic of this article. Dr. Gibson has nothing to disclose.
Bacterial vaginosis, trichomoniasis, and vulvovaginal candidiasis are the most common infectious causes of vaginitis. Bacterial vaginosis occurs when the normal lactobacilli of the vagina are replaced by mostly anaerobic bacteria. Diagnosis is commonly made using the Amsel criteria, which include vaginal pH greater than 4.5, positive whiff test, milky discharge, and the presence of clue cells on microscopic examination of vaginal fluid. Oral and topical clindamycin and metronidazole are equally effective at eradicating bacterial vaginosis. Symptoms and signs of trichomoniasis are not specific; diagnosis by microscopy is more reliable. Features of trichomoniasis are trichomonads seen microscopically in saline, more leukocytes than epithelial cells, positive whiff test, and vaginal pH greater than 5.4. Any nitroimidazole drug (e.g., metronidazole) given orally as a single dose or over a longer period resolves 90 percent of trichomoniasis cases. Sex partners should be treated simultaneously. Most patients with vulvovaginal candidiasis are diagnosed by the presence of vulvar inflammation plus vaginal discharge or with microscopic examination of vaginal secretions in 10 percent potassium hydroxide solution. Vaginal pH is usually normal (4.0 to 4.5). Vulvovaginal candidiasis should be treated with one of many topical or oral antifungals, which appear to be equally effective. Rapid point-of-care tests are available to aid in accurate diagnosis of infectious vaginitis. Atrophic vaginitis, a form of vaginitis caused by estrogen deficiency, produces symptoms of vaginal dryness, itching, irritation, discharge, and dyspareunia. Both systemic and topical estrogen treatments are effective. Allergic and irritant contact forms of vaginitis can also occur.
Vaginitis is defined as a spectrum of conditions that cause vaginal and sometimes vulvar symptoms, such as itching, burning, irritation, odor, and vaginal discharge. Vulvovaginal complaints are one of the most common reasons for women to seek medical advice.
| Clinical recommendation | Evidence rating | Reference |
|---|---|---|
| Clindamycin and metronidazole (Flagyl, Metrogel) are equally effective for eradicating symptoms of bacterial vaginosis. | A | 33 |
| Nitroimidazole drugs (e.g., metronidazole) given orally in a single dose or over a longer period result in parasitologic cure of trichomoniasis in 90 percent of cases. | A | 44 |
| Oral and vaginal antifungals are equally effective for the treatment of uncomplicated vulvovaginal candidiasis. | A | 47 |
| All methods of estrogen delivery relieve the symptoms of atrophic vaginitis. | A | 49 |
Etiology and Diagnosis of Vaginitis
The most common infectious causes of vaginitis are bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis. Physicians traditionally diagnose vaginitis using the combination of symptoms, physical examination, pH of vaginal fluid, microscopy, and the whiff test. When combined, these tests have a sensitivity and specificity of 81 and 70 percent, respectively, for bacterial vaginosis; 84 and 85 percent for vulvovaginal candidiasis; and 85 and 100 percent for trichomoniasis when compared with the DNA probe standard.1 Table 1 describes common causes, symptoms, and signs of vaginitis,2,3 and Table 2 lists risk factors that contribute to the development of the condition.3–11
| Type | Etiology | Clinical symptoms | Clinical signs | |||
|---|---|---|---|---|---|---|
| Discharge | Pain | Pruritus | Vagina | Vulva | ||
| Bacterial vaginosis | Gardnerella vaginalis, Mycoplasma hominis | Malodorous; homogenous; clear, white, or gray; fishy odor | Not primary symptom | Not primary symptom | No signs of inflammation | Unaffected |
| Anaerobic bacteria: Prevotella species, Mobiluncus species | ||||||
| Trichomoniasis | Trichomonas vaginalis | Green-yellow, frothy | Pain with sexual intercourse, vaginal soreness, dysuria | Not primary symptom | Signs of inflammation, “strawberry cervix” | Vestibular erythema may be present |
| Vulvovaginal candidiasis | Candida albicans, Candida krusei, Candida glabrata | White, thick, lack of odor | Burning, dysuria, dyspareunia | Frequent | Signs of inflammation, edema | Excoriations |
| Atrophic vaginitis | Estrogen deficiency | Yellow, greenish, lack of odor | Vaginal dryness, pain with sexual intercourse | Rare | Vagina mildly erythematous, easily traumatized | Vestibule thin and dry; labia majora lose their subcutaneous fat; labia minora irritated and friable |
| Erosive lichen planus | Etiology is unknown | Yellow or gray | Intense pain, dyspareunia, postcoital bleeding | Intense | Erythema with friable epithelium | Erosions, white plaques |
| Irritant or allergic contact dermatitis | Contact irritation or allergic reaction with episodic flares | Minimal | Burning on acute contact, soreness | More likely in allergic reactions | Vulvar erythema possible | Erythema with or without edema; vesicles or bullae rare |
| Type of vaginitis | Risk factors |
|---|---|
| Bacterial vaginosis | Low socioeconomic status, vaginal douching, smoking, use of an intrauterine contraceptive device, new/multiple sex partners, unprotected sexual intercourse, homosexual relationships, frequent use of higher doses of spermicide nonoxynol-9 |
| Trichomoniasis | Low socioeconomic status, multiple sex partners, lifetime frequency of sexual activity, other sexually transmitted infections, lack of barrier contraceptive use, illicit drug use, smoking |
| Vulvovaginal candidiasis | Vaginal or systemic antibiotic use, diet high in refined sugars, uncontrolled diabetes mellitus |
| Atrophic vaginitis | Menopause, other conditions associated with estrogen deficiency, oophorectomy, radiation therapy, chemotherapy, immunologic disorders, premature ovarian failure, endocrine disorders, antiestrogen medication |
| Irritant contact dermatitis | Soaps, tampons, contraceptive devices, sex toys, pessary, topical products, douching, fastidious cleansing, medications, clothing |
| Allergic contact dermatitis | Sperm, douching, latex condoms or diaphragms, tampons, topical products, medications, clothing, atopic history |
In a review of studies published between 1966 and 2003, bacterial vaginosis was diagnosed in 22 to 50 percent of symptomatic women, vulvovaginal candidiasis in 17 to 39 percent, and trichomoniasis in 4 to 35 percent. Approximately 30 percent of symptomatic women remained undiagnosed after clinical evaluation.2 Among multiple individual symptoms and signs, only the following were found to be helpful for the diagnosis of vaginitis in symptomatic women:
A lack of itching makes diagnosis of vulvovaginal candidiasis unlikely (range of likelihood ratios [LRs], 0.18 [95% confidence interval (CI), 0.05 to 0.70] to 0.79 [95% CI, 0.72 to 0.87]).
A lack of perceived odor makes bacterial vaginosis unlikely (LR, 0.07 [95% CI, 0.01 to 0.51]).
Presence of inflammatory signs is more commonly associated with vulvovaginal candidiasis (range of LRs, 2.1 [95% CI, 1.5 to 2.8] to 8.4 [95% CI, 2.3 to 3.1]).
Presence of a fishy odor on examination is predictive of bacterial vaginosis (LR, 3.2 [95% CI, 2.1 to 4.7]).
Lack of odor is associated with vulvovaginal candidiasis (LR, 2.9 [95% CI, 2.4 to 5.0]).2
Individual symptoms and signs, pH level, and microscopy results often do not lead to an accurate diagnosis of vaginitis. Laboratory tests perform better than standard office-based evaluation for diagnosing causes of vaginitis,2 but they do not add substantially to the treatment threshold and are justified only in patients with recurrent or difficult-to-diagnose symptoms. Table 3 describes laboratory tests used to diagnose infectious causes of vaginitis.2,12–24
| Test | Bacterial vaginosis | Trichomoniasis | Vulvovaginal candidiasis | Cost* |
|---|---|---|---|---|
| Point-of-care tests* | ||||
| Amsel criteria | Sensitivity, 69%; specificity, 93% | NA | NA | $$ |
| pH | pH > 5: sensitivity, 77%; specificity, 35% | pH > 5.4: sensitivity, 92%; specificity, 51% | pH < 4.9: sensitivity, 71%; specificity, 90% | $ |
| Whiff test (the amine odor produced by mixing 10% potassium hydroxide solution with a sample of vaginal discharge) | Positive test: sensitivity, 67%; specificity, 93% | Positive test: sensitivity, 67%; specificity, 65% | Negative test | $ |
| Fem Exam card (Cooper Surgical, Shelton, Conn.) Two colorimetric strips: card 1 measures pH and amine levels; card 2 measures proline aminopeptidase activity | Cards 1 and 2 combined: sensitivity, 91%; specificity, 61% | NA | NA | $$ |
| Rapid (two minutes), less subjective than whiff test, easily performed | ||||
| Microscopy (with 10% potassium hydroxide solution, saline) | Clue cells, bacilli with corkscrew motility, scant or absent lactobacilli | Motile protozoa with flagella; more leukocytes than epithelial cells | Budding filaments, mycelia with 10% potassium hydroxide solution | $ |
| Sensitivity, 53 to 90%; specificity, 40 to 100% | Sensitivity, 50 to 70% (may be increased by vaginal lavage to 74%); specificity, 100% | Sensitivity, 61%; specificity, 77% | ||
| pH, trimethylamine card (QuickVue Advance Quidel, San Diego, Calif.) | Sensitivity, 53%; specificity, 97% | NA | NA | $ |
| Rapid, simple, comparable with pH and whiff test | ||||
| Proline aminopeptidase card (Pip Activity TestCard, Litmus Concepts, Inc., Santa Clara, Calif.) Indirect test for a chemical produced by the organisms associated with bacterial vaginosis | Sensitivity, 70%; specificity, 81% | NA | NA | $ |
| Rapid, simple, comparable with Fem Exam card 2 | ||||
| OSOM Trichomonas Rapid Test (Genzyme Diagnostics, Cambridge, Mass.), uses color immunochromatographic “dipstick” technology with murine monoclonal antibodies | NA | Sensitivity, 90 to 100% 10 minutes to complete test | NA | $$$ |
| BD Affirm VPIII Microbial Identification Test (BD Diagnostic Systems, Sparks, Md.) | Sensitivity, 95 to 100% 45 minutes to complete test | Sensitivity, 90 to 100% | Sensitivity, 90 to 100% | $$$ |
| False-positive results may occur, especially in low-prevalence groups | ||||
| Polymerase chain reaction: based on DNA amplification (Quest Diagnostics, Madison N.J.), Instagene Matrix (Bio-Rad Laboratories, Hercules, Calif.) | Effective at identifying bacteria responsible for bacterial vaginosis | Sensitivity, 80%; specificity, 97% | Polymerase chain reaction more sensitive than culture in detecting Candida; not yet commercially available as a diagnostic test | $$$ |
| Reference laboratory testing* | ||||
| Culture | Predictive value of a positive Gardnerella vaginalis culture is less than 50%; generally not recommended, but may have value in recalcitrant cases | InPouch Culture System (Biomed, White City, Ore.) | Positive culture alone does not necessarily indicate that the yeast identified are responsible for vaginal symptoms | $$$ |
| Combined wet-mount preparation and culture kit; can be kept at room temperature for up to 18 hours; samples taken during menses were not adversely affected | ||||
| Sensitivity, 81 to 100% | ||||
| Patient-performed tests | ||||
| Over-the-counter test for vaginal infections (Fem-V; Synova Healthcare, Inc., New York, NY) | Positive test suggests possibility of bacterial vaginosis and need for physician visit (20% false-positive rate) | Positive test suggests possibility of trichomoniasis and need for physician visit (20% false-positive rate) | Negative test suggests possibility of yeast infection | $ |
| Over-the-counter antifungal treatment recommended (10% false-negative rate) | ||||
| Over-the-counter rapid yeast detection test (Savyon Diagnostics, Ashdod, Israel): uses the concept of lateral flow immunoassay systems | NA | NA | Positive test: sensitivity, 73%; specificity, 84% | $ |
| Patient-performed tests have results similar to physician-performed tests | ||||
| Negative test: not sensitive enough to rule out yeast infection and avoid a culture | ||||
A cost-effectiveness analysis of diagnostic strategies for vaginitis undiagnosed by pelvic examination, wet-mount preparation, and related office tests showed that the least expensive strategy was to perform yeast culture, gonorrhea and chlamydia probes at the initial visit, and Gram stain and Trichomonas culture only when the vaginal pH exceeded 4.9. Other strategies cost more and increased duration of symptoms by up to 1.3 days.25
Bacterial Vaginosis
Bacterial vaginosis is the most prevalent cause of vaginal discharge or malodor, occurring in up to 30 percent of women.26 It occurs when the normal Lactobacillus species in the vagina are replaced with anaerobic bacteria, resulting in reduced levels of hydrogen peroxide and organic acids usually present in the vagina.
The underlying cause of bacterial vaginosis is not fully understood. More than 50 percent of women with bacterial vaginosis are asymptomatic. The fishy odor caused by production of amines from anaerobic bacteria found in many of these patients is predictive of bacterial vaginosis.2 When vaginal alkalinity increases after sexual intercourse (with the presence of semen) and during menses (with the presence of blood), the odor becomes more prevalent.27 Vaginal discharge is a more common but less specific symptom. Bacterial vaginosis is not associated with vaginal mucosal inflammation and rarely causes vulvar itch.27
Bacterial vaginosis, even when asymptomatic, is associated with a high incidence of endometritis and pelvic inflammatory disease following abortion and gynecologic procedures in the general population. Among women with bacterial vaginosis, no overall increased risk of developing pelvic inflammatory disease has been found.28 Bacterial vaginosis is associated with late miscarriages, premature rupture of membranes, and preterm birth.29 Both symptomatic and asymptomatic bacterial vaginosis have been strongly linked with an increased risk of human immunodeficiency virus (HIV)-1 transmission (relative risk, 1.89; 95% CI, 1.46 to 2.43).30
DIAGNOSIS
In clinical practice, bacterial vaginosis is diagnosed by the presence of three out of four Amsel criteria31:
Thin, homogenous vaginal discharge
Vaginal pH greater than 4.5
Positive whiff test (fishy amine odor when 10 percent potassium hydroxide solution is added)
At least 20 percent clue cells (vaginal epithelial cells with borders obscured by adherent coccobacilli on wet-mount preparation or Gram stain; Figure 1).
In a prospective observational study of 269 women, a vaginal pH of more than 4.5 was found to be the most sensitive (89 percent) and a positive whiff test was the most specific (93 percent) method of detecting bacterial vaginosis.12 The positive presence of these two tests is as sensitive as three or more Amsel criteria.12 Culture of Gardnerella vaginalis is not recommended because of low specificity. Cervical cytology has no clinical value for diagnosing bacterial vaginosis, especially in asymptomatic women, because it has low sensitivity.13
TREATMENT IN NONPREGNANT WOMEN
Current treatment recommendations from the Centers for Disease Control and Prevention (CDC) are listed in Table 4.13,32 Nonpregnant women with symptomatic disease require antibacterial therapy to relieve vaginal symptoms. Other benefits of treatment include decreasing the risk of HIV and other sexually transmitted infections and reducing infectious complications following abortion or hysterectomy.13

| Medication/dosage | Cost per course of therapy | |||
|---|---|---|---|---|
| Bacterial vaginosis | ||||
| Recommended regimen | ||||
| Metronidazole (Flagyl) | $$ | |||
| 500 mg orally twice daily for seven days | ||||
| Metronidazole gel (Metrogel) | $$$ | |||
| One full applicator (5 g) intravaginally once daily for five days | ||||
| Clindamycin 2% cream | $$$ | |||
| One full applicator (5 g) intravaginally at bedtime for seven days | ||||
| Alternative regimen | ||||
| Tinidazole (Tindamax) | $$$ | |||
| 2 g orally for two days or 1 g for five days | ||||
| Clindamycin | $$$ | |||
| 300 mg orally twice daily for seven days | ||||
| Clindamycin ovules | $$$ | |||
| 100 mg intravaginally once daily at bedtime for three days | ||||
| Pregnancy* | ||||
| Metronidazole | $$ | |||
| 500 mg orally twice daily for seven days | ||||
| Metronidazole | $$ | |||
| 250 mg orally three times daily for seven days | ||||
| Clindamycin | $$ | |||
| 300 mg orally twice daily for seven days | ||||
| Trichomoniasis | ||||
| Recommended regimen | ||||
| Metronidazole | $ | |||
| 2 g orally in a single dose | ||||
| Tinidazole | $$$ | |||
| 2 g orally in a single dose | ||||
| Alternative regimen | ||||
| Metronidazole | $$ | |||
| 500 mg orally twice daily for seven days | ||||
| Pregnancy* | ||||
| Metronidazole | $ | |||
| 2 g orally in a single dose | ||||
| Vulvovaginal candidiasis, uncomplicated | ||||
| Butoconazole 2% cream (Gynazole-1)† | $$ | |||
| 5 g intravaginally once daily for three days | ||||
| Butoconazole 2% cream, sustained release | $ | |||
| 5 g intravaginally in a single dose | ||||
| Clotrimazole 1% cream† | $ | |||
| 5 g intravaginally once daily for seven to 14 days | ||||
| Clotrimazole 2% cream† | $ | |||
| 5 g intravaginally once daily for three days | ||||
| Miconazole 2% cream† | $ | |||
| 5 g intravaginally once daily for seven days | ||||
| Miconazole 4% cream† | $ | |||
| 5 g intravaginally once daily for three days | ||||
| Miconazole vaginal suppository† | ||||
| 100-mg vaginal suppository once daily for seven days | $ | |||
| 200-mg vaginal suppository once daily for three days | $$ | |||
| 1,200-mg vaginal suppository in a single dose | $$ | |||
| Nystatin vaginal tablet | $ | |||
| 100,000-unit vaginal tablet once daily for 14 days | ||||
| Tioconazole 6.5% ointment† | $$ | |||
| 5 g intravaginally in a single dose | ||||
| Terconazole 0.4% cream | $$ | |||
| 5 g intravaginally once daily for seven days | ||||
| Terconazole 0.8% cream | $$ | |||
| 5 g intravaginally once daily for three days | ||||
| Terconazole vaginal suppository | $$ | |||
| 80-mg vaginal suppository once daily for three days | ||||
| Fluconazole (Diflucan) | $$ | |||
| 150 mg orally in a single dose | ||||
| Vulvovaginal candidiasis, complicated | ||||
| Recurrent | ||||
| Initial regimen | ||||
| Any topical agent | ||||
| Seven to 14 days | ||||
| Fluconazole | $$$ | |||
| 100, 150, or 200 mg orally once daily every third day for three doses | ||||
| Maintenance regimen | ||||
| Fluconazole | $$$ | |||
| 100, 150, or 200 mg orally once weekly for six months | ||||
| Severe | ||||
| Any topical azole | $$ | |||
| Intravaginally once daily for seven to 14 days | ||||
| Fluconazole | $$$ | |||
| 150 mg orally once daily in two doses 72 hours apart | ||||
| Vulvovaginal candidiasis, nonalbicans | ||||
| Nonfluconazole azole (oral or topical) | $ | |||
| Seven to 14 days | ||||
| Boric acid gelatin capsule | $$ | |||
| Intravaginally once daily for 14 days | ||||
| Pregnancy* | ||||
| Any topical azole | $$ | |||
| Intravaginally once daily for seven days | ||||
A Cochrane review of 24 randomized controlled trials (RCTs) showed that clindamycin and metronidazole (Flagyl) are equally effective, achieving clinical cure in 91 and 92 percent of cases, respectively, after two to three weeks of treatment.33 Six RCTs showed topical and oral antibiotic preparations to be equally effective. One disadvantage of oral regimens is a longer duration of treatment.33 Intravaginal clindamycin cream is preferred in case of allergy or intolerance to metronidazole. Metronidazole in a single 2-g dose has the lowest effectiveness for treating bacterial vaginosis and is no longer recommended. Metronidazole, 500 mg twice daily for one week, is effective for treating bacterial vaginosis and trichomoniasis.
Although lactobacillus probiotics are safe, there is no conclusive evidence that they are superior to or enhance the effectiveness of antibiotics in the treatment of bacterial vaginosis or prevent its recurrence.34 Treatment of sex partners and follow-up visits if symptoms are resolved are not recommended.
BACTERIAL VAGINOSIS IN PREGNANCY
Bacterial vaginosis is present in up to 20 percent of women during pregnancy. The effect of treating bacterial vaginosis in symptomatic or asymptomatic pregnant women on subsequent preterm delivery has produced conflicting results in clinical trials.13,35 The U.S. Preventive Services Task Force (USPSTF) recommends against routine bacterial vaginosis screening of asymptomatic pregnant women at low risk of preterm delivery (USPSTF grade D recommendation).36
RECURRENT BACTERIAL VAGINOSIS
Most relapses of bacterial vaginosis occur within the first year and strongly correlate with new sex partners. Reported recurrence rates are 15 to 30 percent within three months.37,38 One RCT on persistent bacterial vaginosis indicated that metronidazole gel 0.75% (Metrogel), used twice weekly for six months after initial treatment, effectively maintained a clinical cure for six months.39
Trichomoniasis
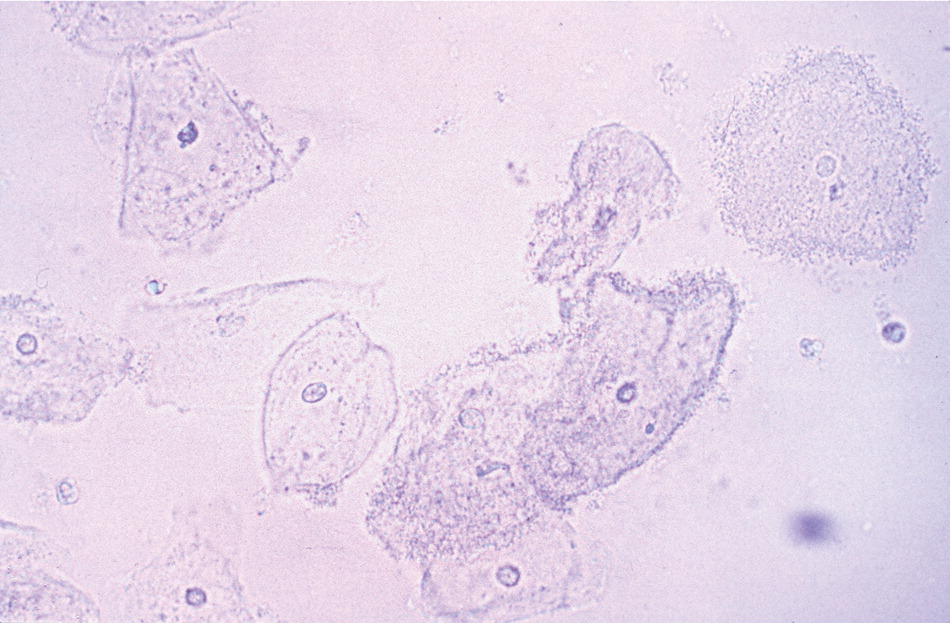
Symptoms and signs of trichomoniasis are not specific, and diagnosis by microscopy is more reliable. Features suggestive of trichomoniasis are trichomonads seen with saline, leukocytes more numerous than epithelial cells, positive whiff test, and vaginal pH greater than 5.4.2 The wet-mount preparation is an inexpensive and quick test with variable sensitivity of 58 to 82 percent,40 and is influenced by the experience of the examiner and the number of parasites in the vaginal fluid sample (Figure 2; a video of motile trichomonads is available at http://www.youtube.com/watch?v=DKJnDz6yBSs&feature=fvsr). Adding examination of the spun urine specimen can increase the detection rate of Trichomonas vaginalis from 73 to 85 percent.41
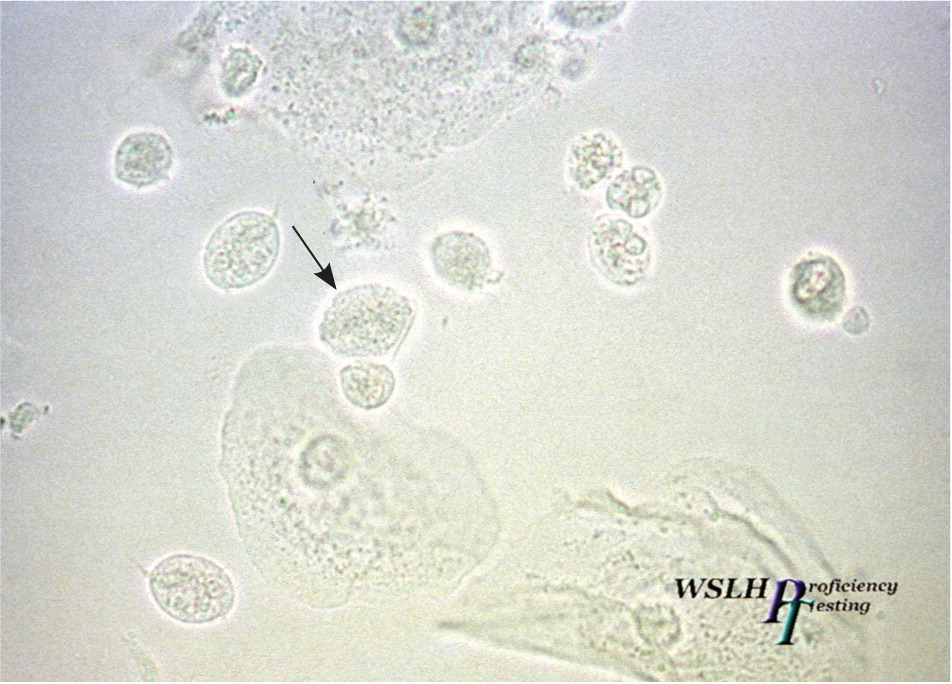
Treatment should not be based on a Papanicolaou (Pap) smear finding of trichomonads. Newer point-of-care tests (Table 32,12–24 ) are more accurate but costly. In one study, the sensitivities of wet-mount preparation, microbiologic culture, rapid antigen testing, and nucleic acid amplification testing were 51, 75, 82, and 98 percent, respectively. Specificity was close to 100 percent for each method.42 Polymerase chain reaction analysis of samples from tampons and introital specimens is more accurate than vaginal or cervical swabs and Pap smears, and may be preferable for patient comfort.43
TREATMENT
Almost any nitroimidazole drug given orally in a single dose or over a longer period results in parasitologic cure in 90 percent of cases.44 A single 2-g dose of metronidazole is adequate but can cause dyspepsia and metallic taste; compliant patients may prefer a longer regimen at a lower daily dosage with fewer adverse effects. Metronidazole in a dosage of 500 mg twice daily for seven days will treat bacterial vaginosis and trichomoniasis. Metronidazole in a dosage of 2 to 4 g daily for seven to 14 days is recommended for metronidazole-resistant strains.
The parasitologic cure rate of intravaginal nitroimidazole creams is an unacceptably low 50 percent. In RCTs, combined oral and intravaginal treatments have been more effective than oral treatment alone. Sex partners should be treated simultaneously.44 To reduce recurrence, partners should avoid resuming sexual intercourse until both have completed treatment and are asymptomatic. Test of cure is not required.13
TRICHOMONIASIS IN PREGNANCY
A Cochrane review found that metronidazole is effective against trichomoniasis when taken by women and their partners during pregnancy. A trial of women treated before 23 weeks of gestation was stopped early because women taking metronidazole were more likely to give birth preterm and have low-birth-weight infants.45 The CDC (Table 413,32 ) recommends giving 2 g of metronidazole as a single dose, preferably after 37 weeks of gestation, and counseling patients about the potential risks and benefits of treatment.
Vulvovaginal Candidiasis
An estimated 75 percent of women will have at least one episode of vulvovaginal candidiasis, and 40 to 45 percent will have two or more.46 Changes in the host vaginal environment precipitate and induce pathologic effects of the organism.14 Several risk factors for vulvovaginal candidiasis are listed in Table 2.3–11
DIAGNOSIS
Although symptoms of vulvovaginal candidiasis such as pruritus, vaginal soreness, dyspareunia, and vaginal discharge are common, none of them are specific.2 Most patients can be diagnosed by microscopic examination (Figure 3) of vaginal secretions with a 10% potassium hydroxide solution (sensitivity, 65 to 85 percent). Vaginal pH is usually normal (4.0 to 4.5). Vaginal culture should be considered in recurrently symptomatic women with negative microscopy and a normal pH. The Pap smear, although specific, is insensitive, with positive results in only about 25 percent of patients with culture-positive symptomatic vulvovaginal candidiasis.14 A rapid yeast detection test (Savyon Diagnostics) can be performed by the patient and costs less than $10, compared with a mean of $65 for the yeast culture.15 Polymerase chain reaction testing is considered the most sensitive method, but is very expensive.

TREATMENT
On the basis of clinical presentation, microbiology, host factors, and response to therapy, vulvovaginal candidiasis can be classified as uncomplicated or complicated.13 Patients with uncomplicated vulvovaginal candidiasis are not pregnant, are otherwise healthy, and have all of the following:
Mild to moderate disease
Fewer than four episodes of candidiasis per year
Pseudohyphae or hyphae visible on microscopy.
Patients with complicated vulvovaginal candidiasis have one or more of the following:
Moderate to severe disease
Four or more episodes of candidiasis per year
Only budding yeast visible on microscopy
Adverse host factors (e.g., pregnancy, diabetes mellitus, immunocompromise).
Noninfectious Causes of Vaginitis
Irritant contact dermatitis and allergic contact dermatitis are two noninfectious causes of vaginitis. They may be associated with use of feminine hygiene products or contraceptive materials, among many other causes. Atrophic vaginitis can manifest clinically with symptoms of vaginal dryness, itching, discharge, irritation, and dyspareunia. It affects 10 to 40 percent of women who have conditions associated with estrogen deficiency.4 Diagnosis is based on history and physical findings, supplemented by vaginal pH levels, vaginal wet-mount preparation (to exclude superimposed infection), and, rarely, culture or cytology. Both systemic and topical estrogen treatments are effective in relieving symptoms. Topical vaginal estrogen is preferred because of the low systemic absorption and reduced risk of adverse effects compared with oral therapy. Estrogen-containing creams, pessaries, intravaginal tablets, and the estradiol vaginal ring appear equally effective for the symptoms of atrophic vaginitis.49
Data Sources: We reviewed recent relevant publications in the Cochrane Database, InfoPOEMS, and the National Guideline Clearing-house, and searched Pub Med for vaginitis topics. The search included meta-analyses, randomized controlled trials, clinical reviews, and clinical trials. Terms included vaginitis, trichomoniasis, bacterial vaginosis, candidal vulvovaginitis, and atrophic vaginitis. Search date: March 2010.
