
A more recent article on nail abnormalities is available.
Am Fam Physician. 2012;85(8):779-787
Author disclosure: No relevant financial affiliations to disclose.
Knowledge of the anatomy and function of the nail apparatus is essential when performing the physical examination. Inspection may reveal localized nail abnormalities that should be treated, or may provide clues to an underlying systemic disease that requires further workup. Excessive keratinaceous material under the nail bed in a distal and lateral distribution should prompt an evaluation for onychomycosis. Onychomycosis may be diagnosed through potassium hydroxide examination of scrapings. If potassium hydroxide testing is negative for the condition, a nail culture or nail plate biopsy should be performed. A proliferating, erythematous, disruptive mass in the nail bed should be carefully evaluated for underlying squamous cell carcinoma. Longitudinal melanonychia (vertical nail bands) must be differentiated from subungual melanomas, which account for 50 percent of melanomas in persons with dark skin. Dystrophic longitudinal ridges and subungual hematomas are local conditions caused by trauma. Edema and erythema of the proximal and lateral nail folds are hallmark features of acute and chronic paronychia. Clubbing may suggest an underlying disease such as cirrhosis, chronic obstructive pulmonary disease, or celiac sprue. Koilonychia (spoon nail) is commonly associated with iron deficiency anemia. Splinter hemorrhages may herald endocarditis, although other causes should be considered. Beau lines can mark the onset of a severe underlying illness, whereas Muehrcke lines are associated with hypoalbuminemia. A pincer nail deformity is inherited or acquired and can be associated with beta-blocker use, psoriasis, onychomycosis, tumors of the nail apparatus, systemic lupus erythematosus, Kawasaki disease, and malignancy.
A thorough inspection of the finger-nails and toenails during the physical examination may reveal localized nail abnormalities that should be treated, or may provide clues to an underlying systemic disease requiring further workup. Tables 11–9 and 21,10–15 list nail abnormalities with localized and systemic etiologies.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Oral terbinafine (Lamisil) has been shown to be an effective long-term therapy for onychomycosis caused by fungal infections. Oral itraconazole (Sporanox) may be more effective for yeast or nondermatophytic mold infections. | A | 2, 3, 21 |
| Treatment of squamous cell carcinoma of the nail includes Mohs surgery or amputation. | C | 8 |
| If no abscess is present, oral antibiotics should be used to treat severe acute paronychia, with consideration for methicillin-resistant Staphylococcus aureus coverage in high-prevalence areas and anaerobic bacteria coverage if exposure to oral flora is suspected. | C | 5–7, 23 |
| Surgical treatment modalities for pincer nail include nail bed cutting with or without splinting. | C | 26 |
| Nail finding | Etiologies | Treatment | |
|---|---|---|---|
| Dystrophic nails (Figure 2) |
| Stop manipulation | |
| Leukonychia (Figure 3) |
| No treatment | |
| Longitudinal melanonychia (vertical nail bands; Figure 4) |
| No treatment if idiopathic, treatment of underlying condition, biopsy if concern for melanoma1 | |
| Onychomycosis (Figure 5) |
| Oral terbinafine (Lamisil),2 itraconazole (Sporanox),3 or fluconazole (Diflucan)4 | |
| Paronychia | |||
| Acute (Figure 6A) |
| Warm soaks, topical antibiotic, topical corticosteroid, surgical drainage (if abscess is present)6 | |
| Chronic (Figure 6B) |
| Avoidance of irritant, treatment of underlying illness, broad-spectrum topical antifungals for superinfection, biopsy if concern for malignancy7 | |
| With pseudomonal superinfection (Figure 6C) |
| Topical neomycin | |
| Squamous cell carcinoma (Figure 7) |
| Mohs surgery, possible amputation of affected digit8 | |
| Subungual hematoma (Figure 8) |
| Nail puncture to relieve pressure, possible nail removal9 | |
| Nail finding | Etiologies |
|---|---|
| Beau lines (Figure 9) | Severe illness, Reynaud disease, pemphigus, chemotherapy, high fever1 |
| Clubbing (Figure 10) | Unilateral: hemiplegia, vascular disorders |
| Bilateral: empyema, cystic fibrosis, pulmonary fibrosis, celiac sprue, bronchiectasis, cardiac disease, cirrhosis, chronic obstructive pulmonary disease, inflammatory bowel disease1 | |
| Koilonychia (spoon nail; Figure 11) | Iron deficiency with or without anemia, hemochromatosis, trauma, Raynaud disease, hypothyroidism, systemic lupus erythematosus, occupational exposure to petroleum-based solvents, nail-patella syndrome10 |
| Mees lines | Arsenic poisoning,1 other heavy metal poisoning, renal failure11 |
| Muehrcke lines (Figure 12) | Hypoalbuminemia, nephrotic syndrome, liver disease, malnutrition12 |
| Pincer nail (Figure 13) | Systemic lupus erythematosus, psoriasis, onychomycosis, tumors of the nail apparatus, Kawasaki disease, malignancy, beta-blocker use13,14 |
| Splinter hemorrhage (Figure 14) | Endocarditis; psoriasis; renal, pulmonary, endocrine diseases; systemic skin conditions15 |
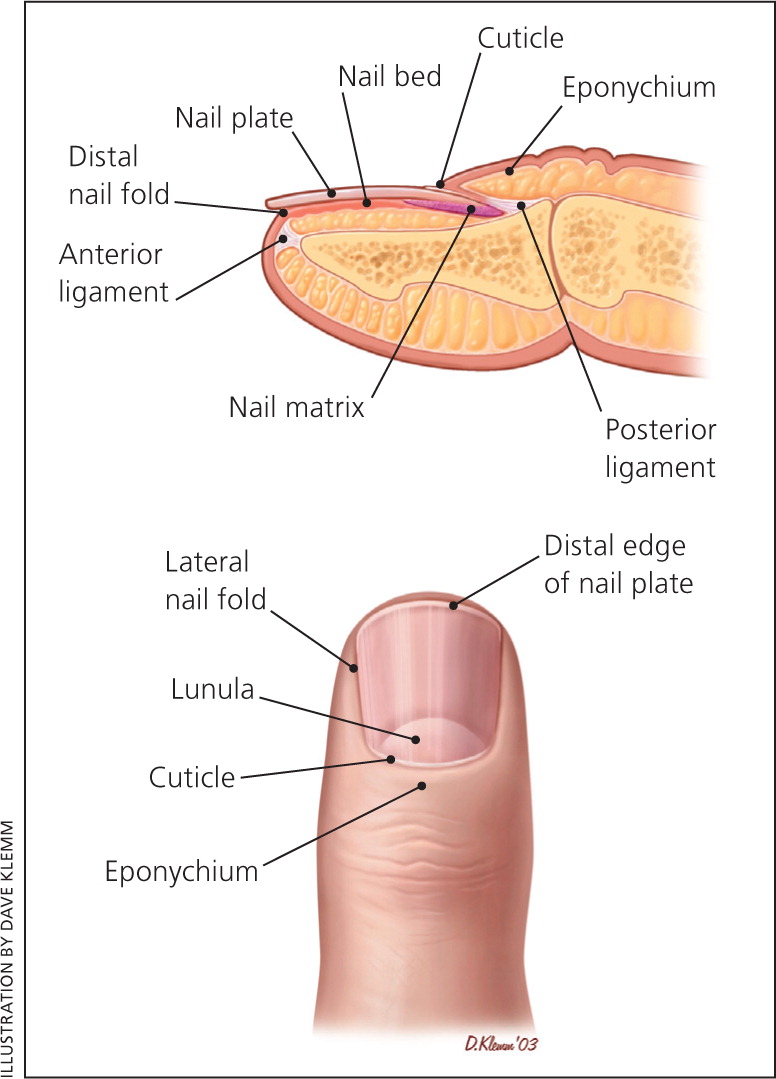
Figure 1 illustrates normal nail anatomy. The nail matrix, located at the proximal nail bed, creates the hard keratinous nail plate. The distal nail matrix is responsible for laying down the deeper layers of the nail plate, whereas the proximal nail matrix creates the superficial layers. Therefore, the nail problem will reflect the location of nail matrix disruption. Disruption of the proximal nail matrix may lead to superficial nail pitting, whereas interruption of the distal nail matrix may cause deeper nail ridging. The nail is bound to the underlying skin proximally by the eponychium, distally by the anterior ligament and the distal nail fold, and on the sides by the lateral nail folds. Disruption in the attachment of the nail plate to the underlying skin may predispose patients to localized infections. Because nails grow slowly (six months to replace the fingernail, and 12 to 18 months to replace the toenail), a nail plate abnormality may reflect an illness that occurred several months prior.16
Local Nail Abnormalities
DYSTROPHIC NAILS (SELF-INDUCED)
Dystrophic nails (Figure 2) can be caused by repeated manipulation of the nail plate (e.g., manicures/pedicures, biting, rubbing). Repeated longitudinal scraping or manipulation can lead to changes of the cuticle and the nail plate, such as the cuticle becoming pushed back, splitting or indentation in the midline of the nail (median nail dystrophy), or inflammation or thickening of the proximal nail fold.

LEUKONYCHIA
Leukonychia (Figure 3) is an abnormal keratinization of the underlying nail matrix resulting in a white discoloration of the nail plate.17 These nonuniform white lines may affect part or all of the nail plate and can occur in a single or multiple nails. This condition is common in healthy adults and children and is of no clinical significance.1

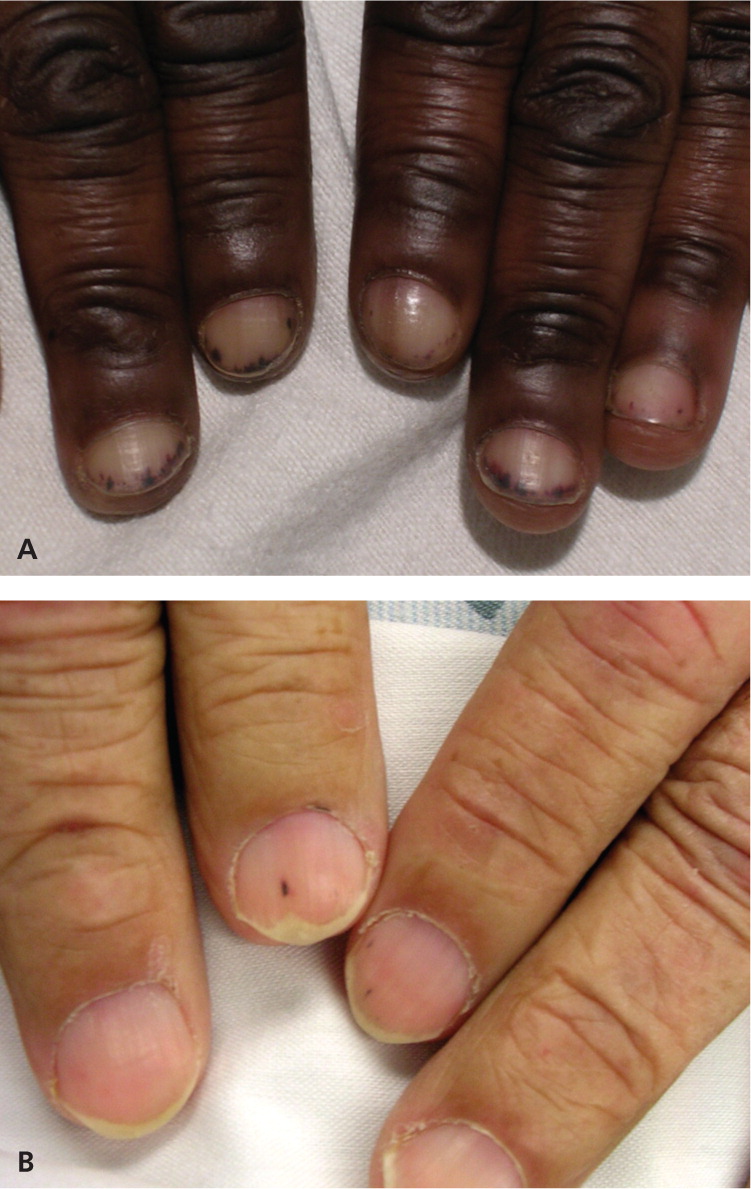
LONGITUDINAL MELANONYCHIA

Vertical nail bands must be differentiated from subungual melanomas, which account for 50 percent of melanomas in persons with dark skin.1 Distinguishing features that increase the likelihood of melanoma include a family history of melanoma, sudden change in the appearance of the bands, involvement of a single nail, band width of more than 3 mm, pigment changes extending onto the cuticle and nail fold (Hutchinson sign), and disruption of the nail plate.18 Vertical nail bands are uncommon in persons with lighter skin.12 Any concern for melanoma should prompt evaluation with a punch biopsy.
ONYCHOMYCOSIS
Onychomycosis encompasses fungal, yeast, and nondermatophytic mold infections of the nail, and predominantly occurs in the distal and lateral portion of the toenails (Figure 5). Onychomycosis can be classified based on the location of the nail bed involved. Distal subungual onychomycosis is the most common form, with dermatophyte spread in the palmar or plantar skin. In patients with proximal subungual onychomycosis, fungal elements appear in the deeper layers of the nail plate; this is more common in immunocompromised patients. White superficial onychomycosis is found in the toenails where fungi colonize the surface of the nail plate. Candidal onychomycosis is rare and may be a sign of underlying immunosuppression.16

Onychomycosis constitutes 50 percent of nail conditions and occurs in more than 10 percent of the population worldwide.19 Infected nails exhibit a white-yellow discoloration and excessive keratinaceous buildup underneath the nail plate. Diagnosis can be made through potassium hydroxide testing of scrapings. If this examination is negative for onychomycosis, a nail culture or nail plate biopsy should be performed.17 Risk factors for this condition include older age, tinea pedis, swimming, psoriasis, and immunodeficiency.20
The infection associated with onychomycosis is embedded within the nail, making it difficult for medications to penetrate. Topical therapies are ineffective. Oral terbinafine (Lamisil) has been shown to be an effective long-term therapy against fungal infections and has fewer side effects than some alternative oral agents.2 Terbinafine has also been shown to be a safe and effective treatment in high-risk patients, such as those with diabetes mellitus or human immunodeficiency virus infection.3 Oral itraconazole (Sporanox) may be a more effective agent for onychomycosis caused by yeast or nondermatophytic molds.3,21 Oral fluconazole (Diflucan) has also been shown to be an effective treatment for onychomycosis infections.4 The beneficial effects of oral medications may not be apparent for 12 to 18 months. The reported long-term recurrence rates of onychomycosis range from 20 to 50 percent.22
PARONYCHIA
Paronychia, which can be acute or chronic, (Figure 6A and 6B) is an inflammatory reaction caused by bacterial invasion of the folds of tissue surrounding the nail.7 It is characterized by the rapid onset of erythema, edema, and tenderness at the proximal and lateral nail folds, usually following trauma.6 Most cases are caused by mixed flora. Staphylococcus aureus and Streptococcus pyogenes are the most common aerobic bacteria associated with paronychia, whereas anaerobic isolates include Bacteroides, Fusobacterium nucleatum, and grampositive cocci.5 Noninfectious causes of paronychia include excessive moisture, contact irritants, and trauma.6 Psoriasis, Reiter syndrome, and herpetic whitlow should be part of the differential diagnosis of recurrent cases.
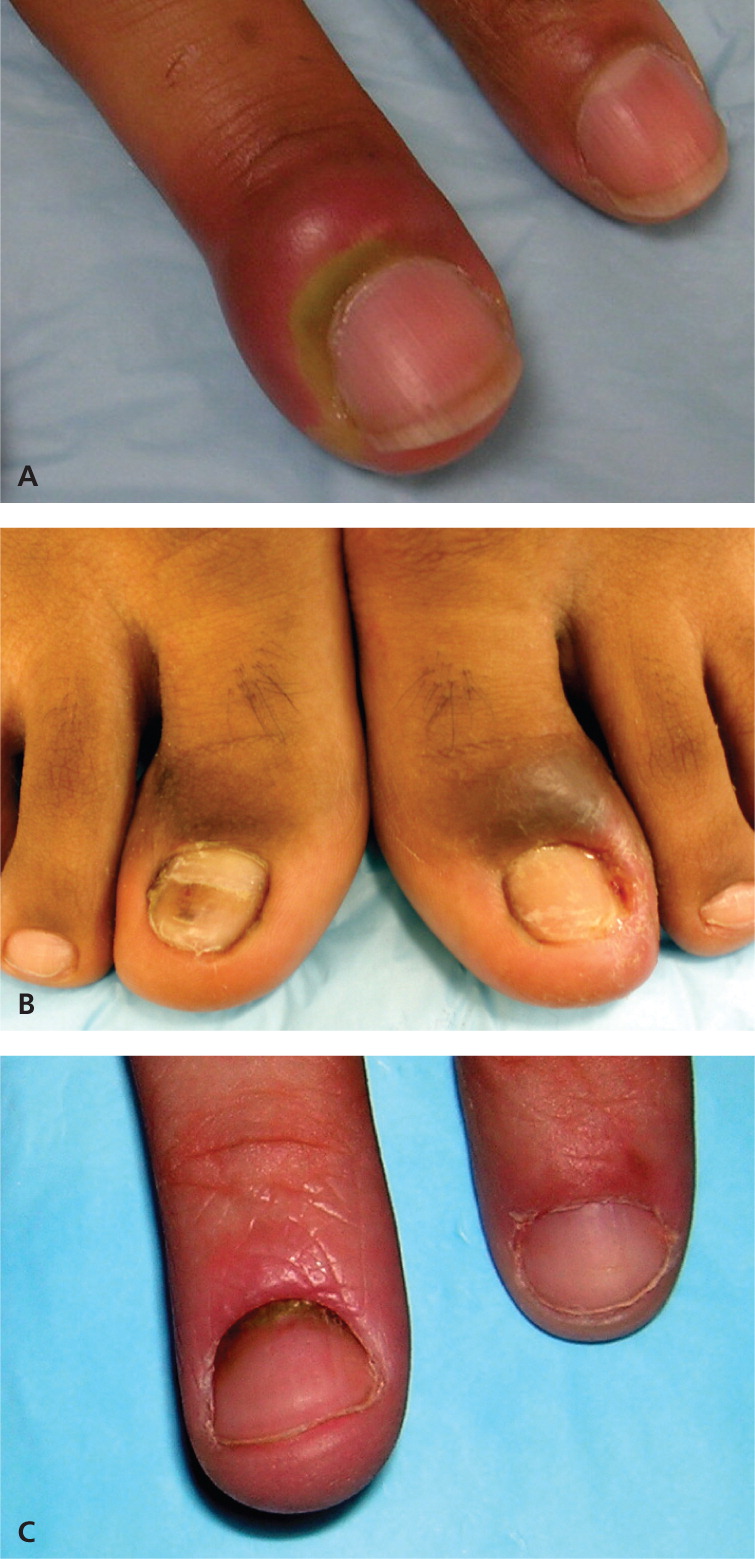
Oral antibiotics may be used for severe infections in which an abscess has not developed. Coverage for methicillinresistant S. aureus should be considered in high-prevalence areas, and coverage for anaerobic bacteria should be considered when exposure to oral flora is suspected.5–7,23 If an abscess is present, surgical drainage is indicated.6
The clinical manifestations of chronic paronychia are similar to those of acute paronychia; however, chronic cases last for more than six weeks. Because of constant infection, the cuticle may separate from the nail plate, forming a space for invasion of various microbes, including bacteria and fungi.23 Patients who are immunosuppressed or who have a systemic illness, such as diabetes or human immunodeficiency virus, are at increased risk of chronic paronychia.6,7 Treatment includes avoiding exposure to contact irritants and appropriate management of the underlying infection. A broad-spectrum topical antifungal, such as ketoconazole, can be used to treat the superinfection and prevent recurrence when a fungus, such as Candida albicans, is suspected.7
Paronychia associated with a pseudomonal infection shares many of the same characteristics of acute and chronic paronychia; however, pseudomonal paronychia commonly leads to a green discoloration (Figure 6C). Pseudomonal superinfection is typically caused by repeated minor trauma to the nail apparatus in a chronically wet environment.6,7 Persons at risk of this condition include bartenders, dishwashers, and habitual nail-biters. Therapy for pseudomonal superinfection should include topical neomycin.
SQUAMOUS CELL CARCINOMA
Squamous cell carcinoma of the nail (Figure 7) can present as a proliferating, erythematous mass that disrupts normal nail morphology. It is commonly mistaken for a verrucous lesion, amelanotic melanoma, or another chronic noninflammatory nail process. Despite the difference in origin, squamous cell carcinoma (originating in the skin) is often mistaken for onychomycosis (originating in the nail plate). Squamous cell carcinoma should be suspected if treatment is ineffective, and a biopsy can confirm the diagnosis. Treatment options include Mohs surgery or amputation.8

SUBUNGUAL HEMATOMA
Subungual hematomas (Figure 8) are painful, dark red to black discolorations caused by bleeding in the underlying vascular nail bed as a result of trauma. If no nail bed laceration is suspected, treatment consists of drilling a hole through the nail into the hematoma to relieve the pressure.24 This procedure involves puncturing the nail with a hot metal wire (i.e., an electrocautery device) or a carbon-dioxide laser. It is important to avoid the lunula and its associated nail matrix during this procedure.24,25

Systemic Nail Abnormalities
BEAU LINES
Beau lines (Figure 9) are horizontal grooves on the nail plate and generally involve most or all of the nails. They reflect an interruption of nail bed mitosis caused by severe illness, pemphigus, high fever, or chemotherapy.1 Beau lines also occur in patients with Raynaud disease. Treatment is aimed at the underlying etiology.

CLUBBING
Clubbing involves thickening of the nail bed's soft tissue, particularly in the proximal end (Figure 10A). This condition usually affects all of the fingernails and rarely occurs in a single digit. Clubbing can be clinically diagnosed with an examination showing Schamroth sign1 (Figure 10B; absence of the diamond-shaped opening that normally appears when the digits are opposed). Lovibond angle (Figure 10C; the angle that forms between the nail plate and the soft tissue of the distal digit) is diagnostic of clubbing if it is greater than 180 degrees.10
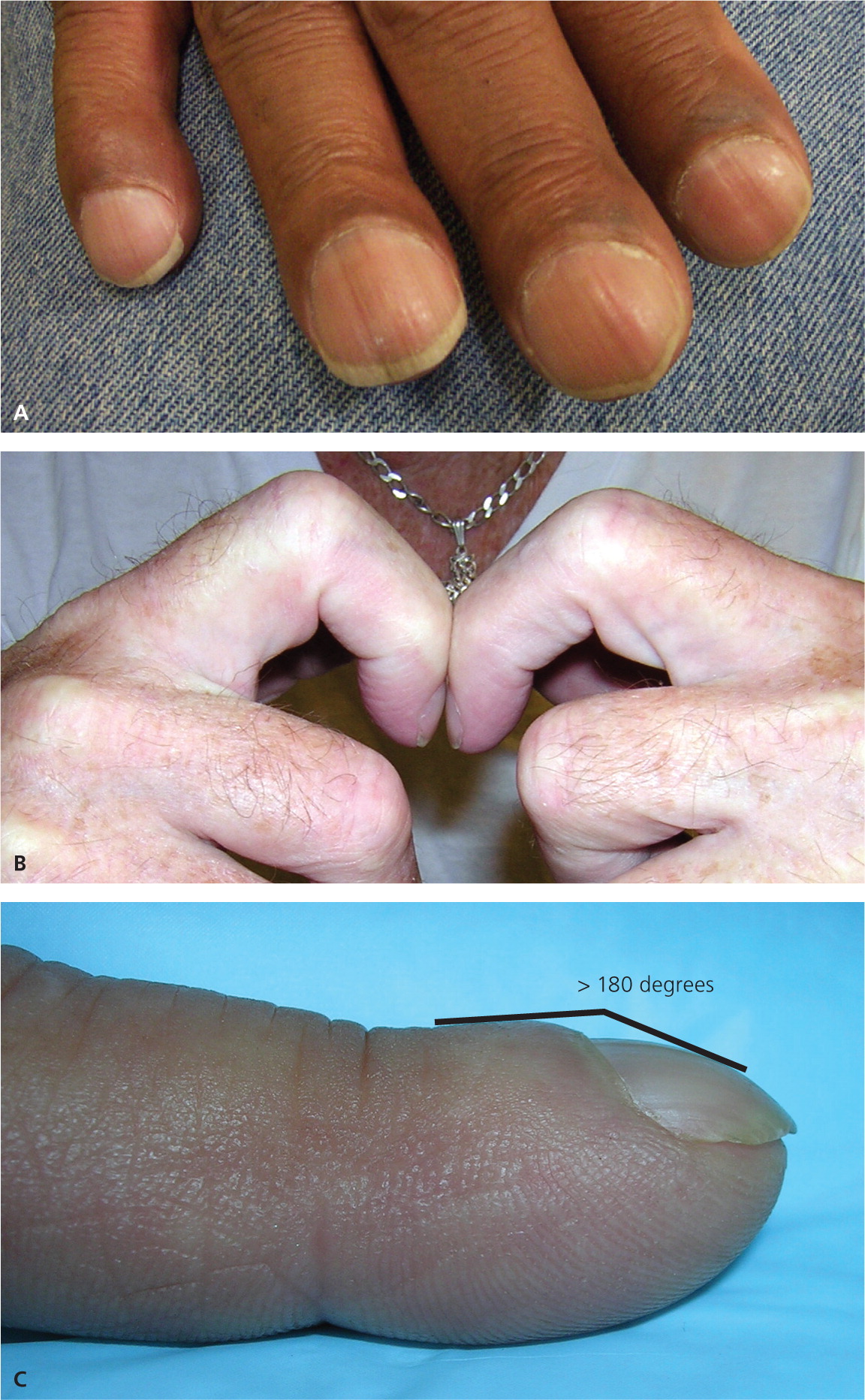
The pathogenesis of clubbing is thought to be secondary to altered vasculature. It is theorized that the thickening of the soft tissue develops from increased blood flow within the microvasculature, instead of within the larger capillaries.10 Clubbing can be a sign of numerous underlying diseases, such as cirrhosis, chronic obstructive pulmonary disease, or celiac sprue.
KOILONYCHIA

MEES LINES
Mees lines are transverse white lines that may extend the complete width of the nail plate. The lines can occur on a single digit or multiple digits. Mees lines migrate toward the distal end of the nail plate over time because the abnormality is in the nail plate and not the nail bed. The differential diagnosis for Mees lines is narrow, and it is thought to be caused primarily by arsenic poisoning.1 Other heavy metal poisonings and renal failure also may result in Mees lines.11 The timing of the poisoning can be estimated based on the rate of nail plate growth.1
MUEHRCKE LINES
Muehrcke lines (Figure 12) are pairs of transverse white lines caused by localized pathology (e.g., edema from hypoalbuminemia) within the nail bed. Because they originate in the nail bed and not the nail plate, the lines do not migrate distally as the nail grows. The nail bed has abnormal vascular architecture that can be visualized microscopically.1 The lines disappear when pressure is applied to the nail plate because the abnormal blood supply is compressed. If the lines are caused by hypoalbuminemia, the nail findings improve as the underlying condition improves.12

PINCER NAIL
Pincer nail (Figure 13) is a transverse overcurvature of the nail plate and may be inherited or acquired. The exact etiology is unknown, but the condition has been associated with beta-blocker use, psoriasis, onychomycosis, tumors of the nail apparatus, systemic lupus erythematosus, Kawasaki disease, and malignancy.13 If pincer nail is associated with medication use, the nail plate returns to normal after cessation of the medication.14 Surgical treatment modalities include nail bed cutting with or without splinting.26

SPLINTER HEMORRHAGE
Splinter hemorrhages (Figure 14) are red-brown, longitudinal lines occurring in the nail bed (not the nail plate) that develop secondary to leaky capillaries.1 When pressure is applied to the nail, they do not disappear because the lines are caused by blood that has leaked out of the vasculature.10 Splinter hemorrhages historically have been associated with endocarditis, typically appearing in the midportion of the nail. However, only 15 percent of patients with endocarditis have them,1 and other causes of proximal nail bed splinter hemorrhages should be considered. Many causes of the condition have been identified. The most common cause is trauma, which often leads to distal nail bed splinter hemorrhages. Systemic causes include endocarditis; psoriasis; renal, pulmonary, and endocrine disease; and systemic skin conditions.15
Data Sources: A PubMed search was completed in Clinical Queries using the key terms nail abnormalities, onychomycosis, paronychia, and clubbing. The search included meta-analyses and reviews. The Database of Abstracts of Reviews of Effects and UpToDate were also searched. Search dates: January through March 2011.
