Am Fam Physician. 2014;90(4):257-258
Author disclosure: No relevant financial affiliations.
A 45-year-old man presented with worsening left-sided, sharp pleuritic chest pain that began one week earlier. The pain started after a few days of dry coughing. It was initially located at the lateral chest wall, then spread to the midsubsternal area and the left axilla. The pain was associated with exertional shortness of breath and dizziness. The patient did not have fever, chills, sputum production, diaphoresis, recent travel, or cold-like symptoms. He had a history of hyperlipidemia and a hiatal hernia. He smoked one pack of cigarettes per day and was obese.
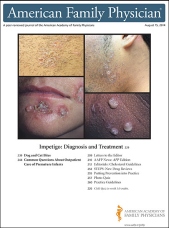
Physical examination revealed no acute distress at rest. Vital signs were unremarkable except for a pulse of 108 beats per minute. His oxygen saturation level was 94% on room air. Lungs were clear to auscultation bilaterally. There was no chest wall tenderness. Auscultation showed a regular rhythm with a third heart sound. There was no peripheral edema or tenderness in the lower extremities on palpation. Electrocardiography (ECG) was performed (see accompanying figure).

Question
Discussion
The answer is E: pulmonary embolism as a consequence of venous thromboembolism. Testing for troponin was negative, but d-dimer test results were elevated. Computed tomography angiography of the chest showed extensive bilateral thromboembolic disease with a saddle embolus. A focal cavitary lesion in the lingular segment was consistent with a pulmonary infarct. An echocardiogram revealed normal left ventricular ejection fraction, but an enlarged right ventricle with severely decreased right systolic function and moderate to severe pulmonary hypertension.
Pulmonary embolism, a manifestation of venous thromboembolism, has high mortality. Symptoms of pulmonary embolism include dyspnea, chest pain, cough, hemoptysis, tachypnea, and syncope. Symptoms may worsen with exertion. Physical examination may reveal rales, tachycardia, diaphoresis, and a third or fourth heart sound. There may not be signs of a deep venous thrombosis. Pulmonary embolism can be diagnosed with chest computed tomography angiography or a ventilation-perfusion scan.
There are no pathognomonic ECG changes for pulmonary embolism; however, the following findings are possible: sinus tachycardia, atrial fibrillation or flutter, axis deviation, right bundle branch block, ST-segment elevation or depression, T-wave inversion in the precordial leads and lead III, Q wave in leads III and aVF, and large S wave in leads I and aVL.1 This patient's ECG showed sinus tachycardia, right axis deviation, prolonged QTc, diffusely inverted T waves that are more prominent at the precordial leads, and the well-known but uncommon right heart strain pattern (prominent S wave in lead I, and Q wave and inverted T wave in lead III [S1Q3T3]). Diffuse T-wave inversion is a nonspecific change that is thought to be related to catecholamine release but with no prognostic implications.2
Typical anginal chest pain associated with acute coronary syndrome is a pressure-like pain that worsens with exertion or emotional stress and improves with rest or nitroglycerin. Pain may radiate to the jaw, neck, shoulder, or left arm. ECG changes include ST-segment elevation or depression, new Q waves, and T-wave inversion. These changes are usually localized to the leads associated with the effected section of myocardium. Elevated troponin levels are seen with cardiac muscle damage.
Gastroesophageal reflux disease can mimic angina. The pain is a squeezing or burning feeling in the substernal area, neck, or jaw. It is usually associated with dyspepsia, regurgitation, or a sour taste in the mouth, and is worse when lying down or after large meals. There are no significant ECG changes.
Pericarditis presents as sharp pleuritic chest pain that worsens with lying down and improves with sitting up or leaning forward. Physical examination may reveal a pleuritic friction rub. Typical ECG changes include diffuse ST-segment elevation or PR-segment depression caused by subepicardial atrial injury.
Pleuritis is inflammation of the pleura.3 Common causes include viral infection, infection of lung parenchyma, and autoimmune diseases. The typical presentation is sudden onset of sharp pleuritic chest pain. ECG shows sinus tachycardia.

| Condition | Characteristics | Electrocardiographic findings |
|---|---|---|
| Acute coronary syndrome | Substernal pressure-like chest pain or discomfort, worsens with exertion or emotional stress and improves with rest or nitroglycerin; pain may radiate to the jaw, neck, shoulder, or left arm | ST-segment elevation or depression, new Q waves, T-wave inversion |
| Gastroesophageal reflux disease | Squeezing or burning chest pain at the substernal area, neck, or jaw; usually associated with dyspepsia, regurgitation, or sour taste in the mouth | None |
| Pericarditis | Sharp pleuritic chest pain, worsens with lying down and improves with sitting up or leaning forward; associated with pleuritic friction rub | Diffuse ST-segment elevation or PR-segment depression |
| Pleuritis | Sharp pleuritic chest pain associated with recent viral infection, infection of lung parenchyma, or autoimmune disease | Sinus tachycardia |
| Pulmonary embolism | Sudden onset of dyspnea, chest pain, cough, hemoptysis, tachypnea, or syncope; may worsen with exertion; may be associated with signs or symptoms of deep venous thrombosis | Rhythm disturbance; T-wave inversion; signs of right heart strain, such as S1Q3T3 pattern (prominent S wave in lead I, and Q wave and inverted T wave in lead III) |