Am Fam Physician. 2015;92(3):187-196
Patient information: See related handout on rosacea, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
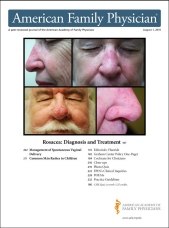
Rosacea is a chronic facial skin condition of unknown cause. It is characterized by marked involvement of the central face with transient or persistent erythema, telangiectasia, inflammatory papules and pustules, or hyperplasia of the connective tissue. Transient erythema, or flushing, is often accompanied by a feeling of warmth. It usually lasts for less than five minutes and may spread to the neck and chest. Less common findings include erythematous plaques, scaling, edema, phymatous changes (thickening of skin due to hyperplasia of sebaceous glands), and ocular symptoms. The National Rosacea Society Expert Committee defines four subtypes of rosacea (erythematotelangiectatic, papulopustular, phymatous, and ocular) and one variant (granulomatous). Treatment starts with avoidance of triggers and use of mild cleansing agents and moisturizing regimens, as well as photoprotection with wide-brimmed hats and broad-spectrum sunscreens (minimum sun protection factor of 30). For inflammatory lesions and erythema, the recommended initial treatments are topical metronidazole or azelaic acid. Once-daily brimonidine, a topical alpha-adrenergic receptor agonist, is effective in reducing erythema. Papulopustular rosacea can be treated with systemic therapy including tetracyclines, most commonly subantimicrobial-dose doxycycline. Phymatous rosacea is treated primarily with laser or light-based therapies. Ocular rosacea is managed with lid hygiene, topical cyclosporine, and topical or systemic antibiotics.
Rosacea is a chronic facial skin condition characterized by marked involvement of the central face with transient or persistent erythema, inflammatory papules or pustules, telangiectasia, or hyperplasia of the connective tissue.1,2 Transient erythema, or flushing, usually lasts less than five minutes and may spread to the neck and chest, often accompanied by a feeling of warmth. Less common findings include erythematous plaques, scaling, edema, phymatous changes (thickening of skin due to hyperplasia of sebaceous glands), and ocular symptoms. Rosacea can be associated with low self-esteem, embarrassment, and diminished quality of life. In a national survey, 65% of patients with rosacea reported symptoms of depression.3
| Clinical recommendations | Evidence rating | References |
|---|---|---|
| Mild cleansers and moisturizers, broad-spectrum sunscreens (sun protection factor [SPF] 30 or greater), and sun avoidance measures should be used to manage all cutaneous rosacea subtypes. | C | 13, 15, 16 |
| First-line therapy for mild to moderate inflammatory rosacea includes topical metronidazole (Metrolotion, Metrocream, Metrogel) or azelaic acid (Finacea). | A | 19 |
| Brimonidine (Mirvaso) can be used to treat persistent facial erythema associated with rosacea. | A | 17, 21 |
| Topical ivermectin (Soolantra) may be used for the treatment of papulopustular rosacea. | B | 18 |
| Subantimicrobial-dose doxycycline (Oracea) can be used to treat inflammatory lesions of papulopustular rosacea. | A | 19, 27 |
| Subantimicrobial-dose doxycycline in combination with topical azelaic acid or metronidazole can be used to treat moderate to severe inflammatory lesions or mild inflammatory lesions that have not responded to initial therapy. | C | 17, 26, 29 |
| Mild ocular rosacea should be treated with eyelid hygiene and topical antibiotic agents, such as metronidazole and erythromycin. | C | 30, 31 |
| Topical ophthalmic cyclosporine drops (Restasis) are more effective than artificial tears in the management of mild ocular rosacea. | B | 19 |
Subtypes
The National Rosacea Society Expert Committee defined four subtypes (Table 1) and one variant.8 Granulomatous rosacea is the sole variant with firm, indurated papules or nodules. Many dermatologists consider rosacea fulminans and perioral dermatitis as rosacea variants. Patients may experience fluctuation in symptoms and overlapping of symptoms between subtypes.9

| Classification | Characteristics |
|---|---|
| Subtype | |
| Erythematotelangiectatic | Flushing and persistent central facial erythema with or without telangiectasia |
| Papulopustular | Persistent central facial erythema with transient, central facial papules or pustules or both |
| Phymatous | Thickening skin, irregular surface nodularities and enlargement; may occur on the nose, chin, forehead, cheeks, or ears |
| Ocular | Foreign body sensation in the eye, burning or stinging, dryness, itching, ocular photosensitivity, blurred vision, telangiectasia of the sclera or other parts of the eye, or periorbital edema |
| Variant | |
| Granulomatous | Noninflammatory; hard; brown, yellow, or red cutaneous papules; or nodules of uniform size |
Pathophysiology
The etiology of rosacea is unknown but is likely multifactorial. Factors involved in the pathophysiology include the dense presence of sebaceous glands on the face, the physiology of the nerve innervation, and the vascular composition of the skin.10 Numerous triggers initiate or aggravate the clinical manifestations of rosacea, including ultraviolet light, heat, spicy foods, and alcohol (Table 2).4,11

| Trigger | Patients with rosacea who report trigger (%) |
|---|---|
| Sun exposure | 81 |
| Emotional stress | 79 |
| Hot weather | 75 |
| Wind | 57 |
| Strenuous exercise | 56 |
| Alcohol consumption | 52 |
| Cold weather | 46 |
| Spicy foods | 45 |
| Certain skin care products | 41 |
| Heated beverages | 36 |
| Certain cosmetics (comedogenic) | 27 |
| Medications (topical steroids, niacin, beta blockers) | 15 |
| Dairy products | 8 |
| Other factors | 24 |
A predilection for fair-skinned individuals of Celtic or northern European descent suggests a genetic component to rosacea.10 However, no specific gene has been identified.4 Patients with the genetic predisposition have a receptor that mediates neovascular regulation. When exposed to triggers, neuropeptide release (flushing, edema) occurs, resulting in recruitment of proinflammatory cells to the skin.10
Diagnosis
Rosacea is diagnosed based on a compatible history and physical examination12 (Table 38 ). One of the following centrofacial features is required: flushing, nontransient erythema (Figures 1A and 1B), telangiectasia (Figure 1C), or papules/pustules8 (Figures 2A and 2B). Laboratory testing is not useful.

| Presence of one or more of the following primary features: | May include one or more of the following secondary features: |
| Flushing (transient erythema) | Burning or stinging |
| Nontransient erythema | Plaque |
| Papules and pustules | Dry appearance |
| Telangiectasia | Edema |
| Ocular manifestations | |
| Peripheral location | |
| Phymatous changes |


Patients may receive a misdiagnosis of skin conditions that share similar features. Rosacea is commonly misdiagnosed as adult acne vulgaris, photodermatitis, seborrheic dermatitis, or contact dermatitis. Table 4 lists features that distinguish these conditions from rosacea. Less common mimicking conditions include systemic lupus erythematosus, atopic dermatitis, folliculitis, bromoderma, and mastocytosis.

| Condition | Distinguishing features |
|---|---|
| Acne vulgaris | Comedone formation |
| No ocular symptoms | |
| Contact dermatitis | Associated with itching and often improves over time when causative agent is removed |
| Photodermatitis | Rash appears on multiple body parts with sunlight exposure |
| Seborrheic dermatitis | Has distinct distribution pattern involving the scalp, eyebrows, and nasolabial folds |
| Systemic lupus erythematosus | Rarely has pustules |
Treatment
GENERAL MEASURES

| Central facial erythema | Phymatous | Ocular | ||||
|---|---|---|---|---|---|---|
| Without papulopustular lesions | With papulopustular lesions | |||||
| Mild to moderate | Moderate to severe | |||||
|
|
|
|
| ||
|
|
|
|
|
| |
|
|
|
|
|
| |
|
|
|
|
|
| |
|
|
|
|
|
| |
Because rosacea can be triggered by a variety of stimuli, avoidance of known triggers is recommended. To identify potential triggers, patients should be encouraged to keep a journal documenting exposures, diet, and activities that cause flare-ups.14
Properly selected skin care products improve and maintain the integrity of the stratum corneum permeability barrier and reduce skin sensitivity.15 Mild cleansing and moisturizing regimens improve patient satisfaction. Cleansers should be fragrance- and abrasive-free with a mildly acidic to neutral pH. Recommended skin cleansers include lipid-free, nonalkaline cleansers (e.g., Cetaphil) and sensitive skin synthetic detergent bars (e.g., Dove Sensitive Skin Bar).16 Patients should cleanse gently with their fingertips, avoid use of abrasive materials, and pat dry for better absorption of moisturizers. Moisturizers should contain emollients and occlusives.14
Although no individual skin care product has been well studied, some products found to improve dryness include polyhydroxy acid (Neostrata), lipid-free nonalkaline (Cetaphil), and ceramide-based formulas (Cerave).16 Patients should avoid astringents, toners, sensory stimulants, and potentially irritating ingredients.16 Photoprotection is universally recommended, including the use of wide-brimmed hats and broad-spectrum sunscreens (minimum sun protection factor [SPF] of 30).13 Dimethicone- and simethicone-based products containing titanium dioxide and zinc oxide may be better tolerated.2 Cosmetics with green or yellow tint applied to the central facial erythema may conceal redness.14
FDA-APPROVED TOPICAL THERAPIES
Topical agents are first-line therapy in the treatment of mild to moderate rosacea (Table 6).17,18 Medication therapy is based on the presence or absence of persistent central facial erythema or inflammation (e.g., papules, pustules, lesional and perilesional erythema), the severity of symptoms, and the patient's response to previous therapeutic interventions.

| Therapy | Formulation and dosage | Effectiveness | Adverse effects | Mechanism of action | Evidence | Cost* |
|---|---|---|---|---|---|---|
| Metronidazole† (Metrogel, Metrocream, Metrolotion) |
| Papules, pustules, erythema | Pruritus, stinging, irritation, dryness | Antioxidant, anti-inflammatory | RCTs |
|
| Azelaic acid† (Finacea) | 15% gel once or twice per day | Papules, pustules, erythema | Stinging, irritation, burning | Antioxidant; decreases KLK5 and cathelicidin | RCTs |
|
| Sulfacetamide/sulfur† (several brands) | 10%/5% cream and other formulations; once or twice per day | Papules, pustules, erythema | Irritation, malodorous, avoid in persons with sulfa allergy | Antibacterial | Small studies and historical precedent |
|
| Brimonidine† (Mirvaso) | 0.33% gel once per day | Erythema | Pruritus, burning, irritation, dryness, erythema; use with caution in patients with CAD or CVD | Vasoconstriction | RCTs |
|
| Ivermectin† (Soolantra) | 1% cream once per day | Papules, pustules | Burning, skin irritation | Antiparastic/anti-inflammatory | RCTs |
|
| Permethrin (Elimite) | 5% cream once per day | Papules, erythema | Irritation, burning | Antiparasitic | Limited studies |
|
| Benzoyl peroxide | 5% gel once or twice per day | Papules, pustules, erythema | Erythema, burning | Antibacterial | Limited studies |
|
| Clindamycin | 1% gel twice per day | Papules, pustules | Pruritus, burning, irritation, dryness | Antibiotic | Limited studies |
|
| Erythromycin | 2% gel twice per day | Papules, pustules | Pruritus, erythema, irritation, dryness | Antibiotic | Limited studies |
|
| Pimecrolimus (Elidel) | 1% cream twice per day | Erythema | Burning | Anti-inflammatory | Limited studies |
|
| Tretinoin |
| Papules, pustules, erythema, possibly telangiectasia | Peeling, erythema, pruritus, dryness, irritation, may exacerbate rosacea photosensitivity | Stimulates epithelial cell turnover | Limited studies |
|
| Oxymetazoline (Afrin) | 0.05% nasal solution every six hours | Erythema | Irritation, burning | Vasoconstriction | Case studies |
|
| Cyclosporine (Restasis) | 0.5% ophthalmic emulsion every 12 hours | Ocular | Hyperemia, burning, blurred vision, tearing | Immunomodulation | RCTs |
|
Five topical agents are approved by the U.S. Food and Drug Administration (FDA) for the treatment of rosacea: metronidazole 0.75% lotion (Metrolotion), 0.75% cream (Metrocream), and 1% gel (Metrogel); azelaic acid 15% gel (Finacea); sulfacetamide 10%/sulfur 5% cream, foam, lotion, or suspension; brimonidine 0.33% gel (Mirvaso); and most recently, topical ivermectin 1% cream (Soolantra).
Metronidazole. Metronidazole is hypothesized to reduce oxidative stress, and has proven effective in reducing erythema and inflammation.19 No significant difference in clinical benefit was found using different vehicles (gel, cream, or lotion) or strengths (0.75% or 1%). Adverse effects were mild, including pruritus, irritation, and dryness.14
Azelaic Acid. Azelaic acid is effective against erythema and inflammatory lesions via inhibiting production of reactive oxygen species in neutrophils.19 No difference in effectiveness was found between once- or twice-daily dosing.20 Adverse events include mild and transient burning, stinging, and irritation.19
Metronidazole vs. Azelaic Acid. Three studies assessed the effectiveness of metronidazole vs. azelaic acid. Although physician-assessed outcomes suggested that azelaic acid may be more effective than metronidazole, patient evaluations found no statistically significant differences. Azelaic acid had a higher incidence of adverse events, including dryness, stinging, scaling, itching, and burning. Symptoms were mild to moderate, and transient in both groups. Neither agent was found to be effective against telangiectasia.19
Sulfacetamide/Sulfur. FDA approval of sulfacetamide/sulfur was granted primarily based on historical use before the implementation of more rigorous standards. Studies demonstrated effectiveness, but were also characterized by high or uncertain risk of bias.17,19 Transient application site reactions occur, and some patients comment about the odor. Use of this second-line agent should be avoided in persons with sulfa allergy.
Brimonidine. Topical metronidazole, topical azelaic acid, and oral doxycycline reduce erythema related to vascular inflammation; however, they have negligible effects on background erythema caused by permanently dilated superficial vessels. Conversely, alpha-adrenergic receptor agonists promote vasoconstriction but have no effect on papulopustular rosacea. Once-daily brimonidine, a topical alpha-adrenergic receptor agonist, is effective in reducing erythema. No tachyphylaxis, rebound erythema, or aggravation of inflammatory lesions was noted. Adverse events were mild, including irritation, burning, dry skin, pruritus, and erythema.21 Oxymetazoline 0.05% nasal solution (Afrin), also an alpha-adrenergic receptor agonist, applied once daily reduces diffuse central erythema based on case reports.22
Ivermectin. Topical ivermectin was approved by the FDA in 2014 for the treatment of papulopustular rosacea.23 Two studies demonstrated effectiveness vs. placebo, and a third found that ivermectin was slightly more effective than topical metronidazole in patient- and physician-assessed outcomes and quality of life.18,23
NON–FDA-APPROVED TOPICAL THERAPIES
One study of permethrin (Elimite) vs. azelaic acid vs. metronidazole demonstrated similar effectiveness in reducing erythema and lesion counts. Two additional studies of permethrin vs. metronidazole demonstrated comparable effectiveness in reducing erythema and papules but not pustules.19
Topical retinoids have limited data to support their use. One small study suggested a reduction in papulopustular lesions. A randomized, double-blind, placebo-controlled study of combination clindamycin 1.2%/ tretinoin 0.025% gel (Veltin; Ziana) suggested benefit in the reduction of telangiectasia and erythema.17,24
Cream containing 1% extract of a flavonoid-rich plant (Chrysanthellum indicum) demonstrated effectiveness based on patient and physician assessment of rosacea severity.19
THERAPIES FOR DIFFUSE CENTRAL ERYTHEMA AND TELANGIECTASIA
Pulsed dye laser, intense pulsed light, and near infrared lasers appear to be effective in treating facial erythema and telangiectasia, although not papulopustular lesions. The cost of these modalities is significant and may not be covered by insurance. Intermittent retreatment is necessary. Adverse events include blistering, purpura, loss of pigmentation, ulceration, and scarring. Near infrared lasers have a greater risk of complications and should be reserved for prominent telangiectasias.25
SYSTEMIC THERAPIES FOR FACIAL ERYTHEMA WITH PAPULOPUSTULAR ROSACEA
Tetracycline and its derivatives have historically been used for the treatment of papulopustular and ocular rosacea. However, the only FDA-approved oral agent is modified-release doxycycline capsule, 40 mg (Oracea). Subantimicrobial-dose doxycycline at 40 mg once daily or 20 mg twice daily is recommended as initial oral therapy 26 (eTable A). Use of subantimicrobial-dose doxycycline avoids development of bacterial resistance while enhancing safety and tolerability.19,27 Adverse reactions include photosensitivity, candidal vaginitis, pill esophagitis, diarrhea, and pseudotumor cerebri. Minocycline (Minocin) has limited data to support its use and uncommon but serious complications, including autoimmune hepatitis, cutaneous hyperpigmentation, vertigo, and drug-induced eosinophilia with systemic symptoms. Patients with symptoms that do not respond to initial therapy may be prescribed antimicrobial-dose doxycycline, tetracycline, minocycline, or other antibiotics.19,26
| Therapy | Dosage | Adverse effects | Caveats | Evidence | Cost* |
|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Ampicillin, erythromycin, and clarithromycin (Biaxin), although effective against papulopustular rosacea in a few studies, are not oral agents of choice because of drug interactions, gastrointestinal intolerance, and concerns about promoting antibiotic resistance. Azithromycin (Zithromax) has greater tolerability, but use has been supported only by case reports and small studies.19,26
Oral metronidazole (Flagyl) has demonstrated similar effectiveness when compared with tetracyclines in four studies,18 but the risk of a disulfiram (Antabuse)-like reaction with alcohol (i.e., nausea, vomiting, diaphoresis, flushing of the skin, tachycardia, shortness of breath, headache, confusion, dizziness), and the rare risk of neuropathy and seizures, relegates its use to patients experiencing treatment failures or intolerance of other agents.19,26
Therapy for Phymatous Rosacea
Phymatous rosacea (Figure 3) can be disfiguring and difficult to treat. Best results are achieved when treatment is instituted early. Oral isotretinoin may be effective in reducing nasal volume in early disease (Table 5); however, recurrence is likely after discontinuation, and mucinous and fibrotic changes are unresponsive.26,28 Surgical techniques including laser- or light-based therapies (pulsed dye laser, intense pulsed light, carbon dioxide laser), electrosurgery, dermabrasion, tangential excision, electroscalpel, loop cautery, and scissor sculpting are effective in correcting or minimizing phymatous changes and may be life-changing.25,26

Therapy for Ocular Rosacea
More than 50% of patients with cutaneous rosacea have ocular symptoms that may include tearing, foreign body sensation, itching, photophobia, and blurred vision. Ophthalmology consultation is recommended because complications (e.g., corneal ulcerations, scleritis, episcleritis, iritis, persistent hordeola and chalazia) may occur.30 Blepharitis, recurrent hordeola, chalazia, and telangiectasias can affect the lid margin (Figure 4). Mild symptoms can be managed with artificial tears, warm compresses, and cleansing the eyelashes with baby shampoo.30 Long-term consumption of omega-3 fatty acids may improve meibomian-gland dysfunction.31 Topical ophthalmic cyclosporine drops (Restasis) demonstrate statistically significant improvement in common signs and symptoms compared with artificial tears.19 Topical metronidazole and erythromycin may be useful for eyelid symptoms. Patients may be treated with systemic therapy using tetracyclines or azithromycin.

Data Sources: We searched the Cochrane Database of Systematic Reviews, PubMed, Medline, and Essential Evidence Plus using keywords rosacea, rosacea and pathophysiology, rosacea and treatment outcome, rosacea and evidence-based medicine, rosacea and drug therapy, and rosacea and dermatological agents. The search included reviews, meta-analyses, randomized controlled trials, consensus guidelines, and clinical trials. Search dates: June 2014 and April 30, 2015.
editor's note: Additional photos of various subtypes of acne rosacea are available at https://www.aafp.org/afp/2009/0901/p461.html.