
Am Fam Physician. 2018;98(8):486-494
Patient information: See related handout on high blood pressure in children.
Author disclosure: No relevant financial affiliations.
High blood pressure in children and adolescents is a growing health problem that is often overlooked. Children should be screened for elevated blood pressure annually beginning at three years of age or at every visit if risk factors are present. In children younger than 13 years, elevated blood pressure is defined as blood pressure in the 90th percentile or higher for age, height, and sex, and hypertension is defined as blood pressure in the 95th percentile or higher. In adolescents 13 years and older, elevated blood pressure is defined as blood pressure of 120 to 129 mm Hg systolic and less than 80 mm Hg diastolic, and hypertension is defined as blood pressure of 130/80 mm Hg or higher. Ambulatory blood pressure monitoring should be performed to confirm hypertension in children and adolescents. Primary hypertension is now the most common cause of hypertension in children and adolescents. A history and physical examination and targeted screening tests should be done to evaluate for underlying medical disorders, and children and adolescents with hypertension should be screened for comorbid cardiovascular diseases, including diabetes mellitus and hyperlipidemia. Hypertension in children is initially treated with lifestyle changes such as weight loss if overweight or obese, a healthy diet, and regular exercise. Children with symptomatic hypertension (e.g., headaches, cognitive changes), stage 2 hypertension without a modifiable factor such as obesity, evidence of left ventricular hypertrophy on echocardiography, any stage of hypertension associated with chronic kidney disease or diabetes, or persistent hypertension despite a trial of lifestyle modifications require antihypertensive medications and should be evaluated for cardiovascular damage with echocardiography. Angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, calcium channel blockers, and thiazide diuretics are effective, safe, and well-tolerated in children.
High blood pressure in children and adolescents is a growing health problem, along with the worldwide epidemics of obesity and physical inactivity. The combined prevalence of elevated blood pressure and hypertension in children is around 6%, or 3% for each.1,2 The combined prevalence increases by nearly five times, to around 30%, in adolescents who are obese.2 High blood pressure in childhood is correlated with higher blood pressure and risk of cardiovascular disease (CVD) in adulthood, and this relationship strengthens with age.3 Primary hypertension in children is associated with other risk factors for CVD, including hyperlipidemia and insulin resistance.4 Children also experience target organ damage from hypertension, including left ventricular hypertrophy and pathologic vascular changes (i.e., carotid intima-media thickness).5,6
WHAT IS NEW ON THIS TOPIC
Normal and elevated blood pressures for children one to 12 years of age are based on the normative distribution of blood pressures in healthy children of normal weight and should be interpreted on the basis of sex, age, and height. For adolescents 13 years and older, elevated blood pressure is now defined by the absolute value of 120 to 129 mm Hg systolic and < 80 mm Hg diastolic, and hypertension as ≥ 130/80 mm Hg.
Primary hypertension, rather than secondary hypertension, now accounts for most cases of childhood hypertension.
When available, ambulatory blood pressure monitoring is recommended to help clarify the diagnosis in children who have had elevated blood pressure readings for one year or more, or earlier if it is necessary to confirm the diagnosis of hypertension.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Children should have blood pressure measured annually beginning at three years of age. Measurement should occur at every health care encounter in children who are obese; who have known kidney disease, aortic arch obstruction, coarctation, or diabetes mellitus; or who are taking a medication known to increase blood pressure. | C | 8 |
| When available, ambulatory blood pressure monitoring should be used to confirm hypertension in children and adolescents. | C | 8, 11, 12, 25, 26 |
| All children and adolescents with hypertension should be screened for hyperlipidemia and underlying renal disease via urinalysis and electrolyte, blood urea nitrogen, and creatinine testing. | C | 8, 11 |
| Children younger than six years with hypertension, and children and adolescents with abnormal renal function or urinalysis results should undergo renal ultrasonography. | C | 8 |
| Obese children and adolescents with hypertension should be evaluated for diabetes mellitus and fatty liver. | C | 8, 11 |
| All children with elevated blood pressure or hypertension should make therapeutic lifestyle changes (e.g., lose weight if overweight or obese; get regular physical activity; eat a healthy diet low in salt; avoid smoking and alcohol intake; reduce stress). | C | 8, 29–34 |
| Children with symptomatic hypertension, stage 2 hypertension without a modifiable factor such as obesity, evidence of left ventricular hypertrophy on echocardiography, any stage of hypertension associated with chronic kidney disease or diabetes, or persistent hypertension despite a trial of lifestyle modifications require antihypertensive medications. | C | 8 |
Despite the increasing prevalence and potential risks of hypertension in children, the diagnosis is often overlooked.7 One study revealed that only 26% of children with high blood pressure consistent with hypertension documented in an electronic medical record were subsequently diagnosed as having hypertension.1
In 2017, the American Academy of Pediatrics (AAP) updated its clinical practice guideline for the screening and management of high blood pressure in children and adolescents.8,9 A 2018 study has already demonstrated a significant increase in hypertension diagnoses using the updated guideline. In a cohort of at-risk youth 10 to 18 years of age with comorbid diabetes and obesity, the prevalence of hypertension was 13% using the new guideline, compared with 8% using the old guideline. Furthermore, use of the new guideline demonstrated increased sensitivity in identification of hypertensive end organ damage.10 An understanding of current guidelines on the diagnosis and treatment of hypertension in children is needed to combat this increasingly common condition.
Definition of Hypertension
Normal and elevated blood pressure values for children one to 12 years of age are based on the normative distribution of blood pressure in healthy children of normal weight and should be interpreted based on age, height, and sex. The AAP guideline includes suggested screening thresholds and percentile-based diagnostic tables (view these tables).8 Absolute blood pressure values are used beginning at 13 years of age. For these adolescents, elevated blood pressure is defined as a blood pressure of 120 to 129 mm Hg systolic and less than 80 mm Hg diastolic, and hypertension is defined as blood pressure of 130/80 mm Hg or higher (Table 1).8
| For children aged 1–13 y | For children aged ≥ 13 y |
|---|---|
| Normal BP: < 90th percentile | Normal BP: < 120/< 80 mm Hg |
| Elevated BP: ≥ 90th percentile to < 95th percentile or 120/80 mm Hg to < 95th percentile (whichever is lower) | Elevated BP: 120/< 80 to 129/< 80 mm Hg |
| Stage 1 HTN: ≥ 95th percentile to < 95th percentile + 12 mm Hg, or 130/80 to 139/89 mm Hg (whichever is lower) | Stage 1 HTN: 130/80 to 139/89 mm Hg |
| Stage 2 HTN: ≥ 95th percentile + 12 mm Hg, or ≥ 140/90 mm Hg (whichever is lower) | Stage 2 HTN: ≥ 140/90 mm Hg |
Hypertension in children and adolescents is further characterized as primary (essential) or secondary. Secondary hypertension has an underlying cause that is identifiable and may be treated (Table 28,11,12), whereas primary hypertension is a diagnosis of exclusion when an underlying disorder cannot be found.11,12 Although secondary hypertension was previously more common in children, primary hypertension now accounts for most cases of childhood hypertension.13
| Etiology | Findings | ||
|---|---|---|---|
| History | Physical examination | Laboratory and other studies | |
| Coarctation of aorta | None | Diminished femoral pulses Heart murmur Lower blood pressure in legs than in arms Possible difference in blood pressure between right and left arms | Abnormal echocardiogram findings |
| Cushing syndrome | Family history of endocrinopathy | Acne, hirsutism, striae Moon facies Truncal obesity | Elevated cortisol levels |
| Drug-induced | Illicit substances: amphetamines, anabolic steroids, cocaine, phencyclidine Over-the-counter medications and supplements: caffeine, diet pills, Ephedra, performance-enhancing drugs, decongestants Prescription medications: oral contraceptives, steroids, sympathomimetics/stimulants | Acne, hirsutism, striae (anabolic steroid use) Sweating Tachycardia | Abnormal urine drug screen; normalization of blood pressure when the drug is discontinued |
| Hyperthyroidism | Family history of thyroid disorder Heat intolerance Rash, sweating, pallor | Ophthalmopathy Tachycardia Thyromegaly Weight loss | Suppressed thyroid-stimulating hormone |
| Mineralocorticoid excess (congenital adrenal hyperplasia, aldosterone-secreting tumors) | Family history of endocrinopathy | Ambiguous genitalia Muscle weakness | Elevated plasma aldosterone levels, hypokalemia, low plasma renin activity |
| Obstructive sleep apnea | Family history of sleep apnea Snoring or disordered sleep | Adenotonsillar hypertrophy | Abnormal polysomnogram |
| Pheochromocytoma | Flushing, pallor, palpitations, sweating | Tachycardia | Elevated levels of plasma and urine catecholamines |
| Primary hypertension | Adolescent age Diet high in fat and salt Family history of essential hypertension or early cardiovascular disease Limited physical activity | Acanthosis nigricans (because associated with diabetes mellitus) Obesity | Hyperlipidemia Impaired glucose tolerance or type 2 diabetes |
| Renal artery stenosis | Prior umbilical artery catheterization | Abdominal bruit | Abnormal renovascular imaging |
| Renal parenchymal disease | Enuresis Family history of renal disease Fatigue Recurrent urinary tract infections | Abdominal mass Edema Gross hematuria Growth retardation | Abnormal blood urea nitrogen, creatinine, urinalysis or urine culture Abnormal renal ultrasonography Anemia |
| Rheumatologic disorder | Family history of autoimmune disease Fatigue Joint pain Rash | Friction rub Joint swelling Malar rash | Abnormal autoimmune laboratory tests, elevated markers of inflammation |
Risk Factors
Increasing body mass index, obesity, and abdominal circumference are correlated with increased hypertension rates in children and adolescents.14 Other chronic conditions that are correlated with childhood hypertension include disordered sleep (i.e., obstructive sleep apnea, disorders of primary snoring, sleep fragmentation), and chronic kidney disease.15,16 Race and ethnicity are linked to hypertension risk, with Hispanic and black children at greater risk.17 Family history of hypertension or CVD, male sex, low birth weight, and maternal smoking during pregnancy are additional risk factors, whereas children who were breastfed have a reduced risk of hypertension.14,17–19
Diagnosis
MEASUREMENT AND DETECTION OF ELEVATED BLOOD PRESSURE
In 2013, the U.S. Preventive Services Task Force and the American Academy of Family Physicians cited insufficient evidence to recommend screening for high blood pressure in average-risk children.20,21 Based primarily on expert opinion, the 2017 AAP guidelines recommend measuring blood pressure annually beginning at three years of age, and the 2016 European Society of Hypertension guidelines recommend screening every two years beginning at three years of age.8,11 Measurements should occur at every health care encounter in children and adolescents with risk factors (i.e., those who are obese; who have known kidney disease, aortic arch obstruction, coarctation, or diabetes mellitus; or who are taking a medication known to increase blood pressure).8,11 Blood pressure should be measured in children younger than three years only if they have risk factors for hypertension, which includes the same risk factors as older children in addition to prematurity, a family history of congenital renal disease, a history of organ or bone marrow transplant, malignancy, elevated intracranial pressure, and systemic illnesses known to increase blood pressure.8
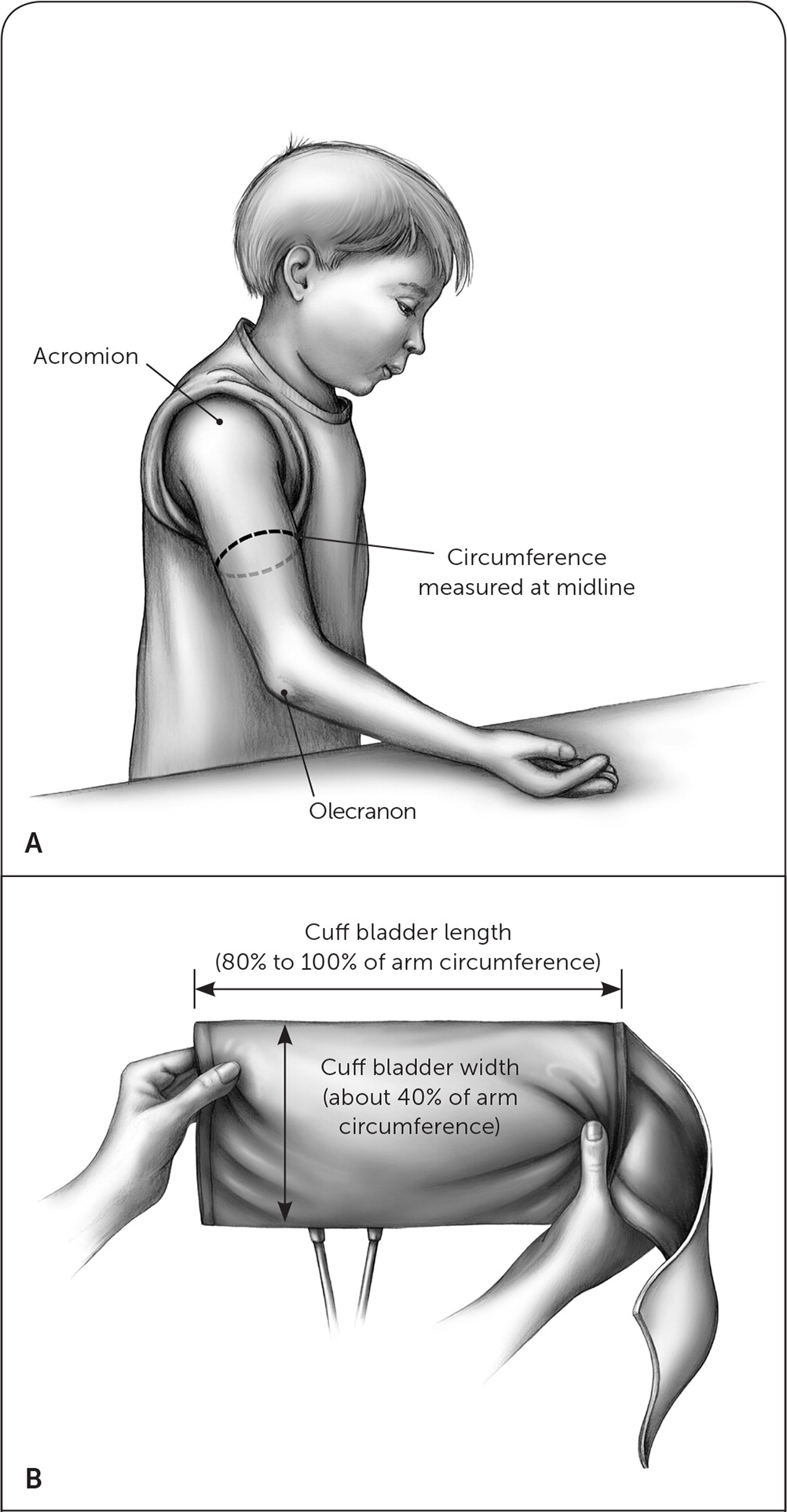
Obtaining an accurate blood pressure measurement in children and adolescents can be challenging given the variance of blood pressure with cuff size, anxiety level, caffeine intake, time of day, and patient positioning. For the most accurate reading, the patient should be sitting quietly for at least three to five minutes with his or her back supported, and feet uncrossed and flat on the floor.22 An appropriate-sized cuff should be used, with an inflatable bladder width that is at least 40% of the arm circumference and bladder length that is 80% to 100% of the arm circumference. Arm circumference is measured at a point midway between the acromion and the olecranon (Figure 123). Blood pressure should be measured with the arm supported at the level of the heart. The right arm should be used because coarctation of aorta may lead to falsely low readings in the left arm. Physicians who care for children and adolescent patients must have access to cuffs of varying sizes to ensure an appropriate fit.
An initial blood pressure measurement can be performed using auscultation or an oscillometric (automatic) device. Oscillometric devices have been found to overestimate both systolic and diastolic blood pressure. Regardless of the initial method used, an initial elevated blood pressure reading should be followed with at least two additional auscultatory measurements to improve accuracy.24,25 The auscultative values should then be averaged to determine the blood pressure classification for the visit.8
Although recognition of elevated blood pressure in adolescents 13 years and older has been simplified by alignment with adult values, it can be challenging to determine which children younger than 13 years require further evaluation and repeated blood pressure measurements. Electronic health records can aid in the identification of high blood pressure by using decision support tools that flag abnormal results. Once an elevated blood pressure reading has been confirmed during an office visit, the next steps in patient management are largely dependent on the stage and degree of elevation (Figure 2).8
Ambulatory blood pressure monitoring in children and adolescents has been found to be more accurate than blood pressure measurement in a clinic, and has a prominent role in the updated AAP guidelines.8,26 Ambulatory blood pressure monitoring refers to a specific validated device that assesses blood pressure every 20 to 30 minutes around the clock. Home blood pressure cuffs and wrist monitors are not well validated in children and should not be used. When available, ambulatory blood pressure monitoring is recommended to help clarify the diagnosis in children who have had elevated blood pressure readings for one year or more, or earlier if it is necessary to confirm the diagnosis of hypertension.8,11,12,25,26 Because of the complexity of interpreting blood pressure values in children and the need for specialized equipment in different sizes, subspecialist consultation is typically needed for ambulatory blood pressure monitoring in this population.
Following the diagnosis of elevated blood pressure or hypertension, a careful history and physical examination can help determine if the child has primary or secondary hypertension. Very young children, children or adolescents with normal weight and no family history of hypertension, and children and adolescents with signs and symptoms suggesting an additional underlying systemic disorder require a more extensive evaluation for secondary hypertension. In addition, children or adolescents with a blood pressure of 30 mm Hg or more above the 95th percentile or adolescents with a blood pressure greater than 180/120 mm Hg should be referred for emergency care.8
HISTORY
A medical history, including birth history; growth and development; and screening for previous urologic, renal, cardiac, endocrine, or neurologic diseases, should be done. Because many drugs can increase blood pressure, physicians should review any prescription and over-the-counter medications and supplements, performance-enhancing drugs, and illicit substances the patient may be using. Disordered sleep is associated with hypertension, and thus a sleep history should be completed. Patients should be screened for a family history of hypertension, other CVD risk factors, and familial renal or endocrine syndromes. Physical activity, diet, smoking status, and alcohol intake should also be explored.8 Older children and adolescents should be asked about abuse, bullying, body perception, depression, and anxiety, which have been found to be risk factors for elevated blood pressure.8,27 A complete review of systems may suggest an underlying medical disorder or reveal symptoms that can be associated with acute severe hypertension, such as headache, vomiting, or altered mental status.
PHYSICAL EXAMINATION
Although physical examination findings are normal in most children with hypertension, any abnormalities that are found may help with diagnosing a secondary cause. The body mass index percentile should be calculated because obesity is associated with primary hypertension, and poor growth may indicate an underlying chronic illness. If blood pressure is persistently elevated, it should be measured in both arms while the child is in a seated position and in a leg while in a prone position. Blood pressure should be roughly equal in both arms and is normally 10 to 20 mm Hg higher in the legs. If there is a significant difference in blood pressure between the right and left arms, blood pressure in the leg is lower than in the arm, there is a heart murmur, or femoral pulses are diminished, then the child may have coarctation of aorta. An abdominal bruit may indicate renovascular disease, and ambiguous genitalia or proximal muscle weakness can be associated with a mineralocorticoid excess.8 The remainder of the examination should look for physical findings associated with other underlying conditions that cause hypertension.
DIAGNOSTIC TESTING
Initial tests are performed to evaluate for an underlying etiology, identify other CVD risk factors, and detect target organ damage. All children and adolescents with hyper-tension should be screened for hyperlipidemia and underlying renal disease via urinalysis and electrolyte, blood urea nitrogen, and creatinine testing.8,11 Children younger than six years with hypertension and children and adolescents with abnormal renal function or urinalysis results should undergo renal ultrasonography.8 Children and adolescents who are obese should be evaluated for diabetes and fatty liver.8,11
An extensive evaluation for secondary causes of hypertension is not necessary in children six years and older who are overweight or obese, have a family history of hypertension, and/or have normal comprehensive history and physical examination findings.8,28 If there is a high degree of suspicion that the child has secondary hypertension, further targeted workup may be indicated, typically in conjunction with subspecialist consultation (pediatric nephrology or cardiology, based on availability and suspected underlying etiology).
Children with persistently elevated blood pressure despite nonpharmacologic measures, stage 2 hypertension without a modifiable underlying factor, or comorbid diabetes or chronic kidney disease should be evaluated for cardiovascular damage with echocardiography.8
| Test | Purpose | Target population |
|---|---|---|
| Bilateral upper arm and single leg blood pressure measurement | Rule out coarctation of aorta | All children and adolescents |
| Chemistry panel, including electrolytes, blood urea nitrogen, and creatinine; urinalysis | Assess for underlying renal disease | All children and adolescents |
| Lipid profile | Assess for an additional cardiovascular disease risk factor | All children and adolescents |
| Drug screening | Rule out underlying substances contributing to or causing elevated blood pressure | Children and adolescents with history suggestive of substance use |
| Echocardiography (consider annually) | Assess for cardiac target organ damage | Children and adolescents in whom pharmacologic therapy is being considered |
| Fasting glucose or A1C level; aspartate/alanine transaminase levels | Assess for diabetes mellitus and fatty liver as additional cardiovascular risk factors | Children and adolescents who are obese |
| Polysomnography | Rule out obstructive sleep apnea | Children and adolescents with history suggestive of a sleep disorder |
| Renal ultrasonography, complete blood count | Assess for underlying renal disease | Children younger than six years and children and adolescents with abnormal renal function or urinalysis findings |
Treatment
For children and adolescents, the blood pressure goal is less than the 90th percentile for age, height, and sex for patients younger than 13 years, or less than 130/80 mm Hg for those 13 years and older.8
LIFESTYLE MODIFICATIONS
All children with elevated blood pressure or hypertension should make therapeutic lifestyle changes (Table 4) to lower blood pressure and reduce the risk of developing additional CVD risk factors.8,29–34 Weight loss should be encouraged for children who are overweight or obese, and those who are obese should be referred for comprehensive, intensive, family-oriented behavioral intervention programs.8 There is no evidence-based guideline to recommend a specific length for a lifestyle modification trial, but various research studies suggest a period of three to six months is sufficient to determine likely effectiveness.8
| Lifestyle modification | Recommendations |
|---|---|
| Weight reduction if overweight or obese | Focus on a multifaceted approach emphasizing changes to diet and increased physical activity; refer for comprehensive, intensive intervention if patient is obese |
| Regular physical activity | 30 to 60 minutes of moderate to vigorous physical activity at least three to five days per week |
| Healthy diet | The Dietary Approaches to Stop Hypertension diet, which emphasizes increased fresh fruits and vegetables, fiber, and low-fat dairy, and decreased sodium intake |
| Avoidance of substance use | Avoid smoking and excessive alcohol intake |
| Stress reduction | Breathing awareness meditation and yoga may help lower blood pressure |
| Family-based interventions | Involving the family in counseling on diet and exercise to make changes for the entire household has been shown to improve success |
Regular, sustained physical activity is most effective at lowering blood pressure, and children and adolescents should engage in 30 to 60 minutes of moderate to vigorous physical activity at least three to five days per week.8,29 One study demonstrated that exercising for 60 minutes three times per week over three months leads to an average seven-point decrease in systolic blood pressure and a 12% decrease in the rate of hypertension among prepubertal children who are obese.29 Children with elevated blood pressure, stage 1 hypertension without end organ damage, or controlled stage 2 hypertension are eligible for participation in competitive sports.35
Multiple aspects of the Dietary Approaches to Stop Hypertension (DASH) diet have been associated with lower blood pressure in children and adolescents.30,31 Children with hypertension should be counseled on striving for a diet high in fresh fruits and vegetables, fiber, and low-fat dairy in addition to a reduction in sodium intake.8,11
There are scant but growing data that complementary medicine techniques for stress reduction (e.g., breathing awareness meditation, yoga) may decrease blood pressure in children and adolescents.32 Tobacco and alcohol use should be avoided in all children, and this is of particular importance in children with hypertension because smoking increases the risk of CVD, and excess alcohol intake has been found to raise blood pressure in adolescents.33,34
PHARMACOLOGIC THERAPY
Children with symptomatic hypertension (e.g., headaches, cognitive changes), stage 2 hypertension without a modifiable factor such as obesity, evidence of left ventricular hypertrophy on echocardiography, any stage of hypertension associated with chronic kidney disease or diabetes, or persistent hypertension despite a trial of lifestyle modifications require antihypertensive medications.8 There is no consensus on the best initial antihypertensive medication to use in children, and there have been no clinical trials of hypertension treatment in children that measured patient-oriented, long-term outcomes.
Angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, calcium channel blockers, and thiazide diuretics are effective, safe, and well tolerated in children.8,11 Beta blockers are no longer considered first-line therapy for hypertension treatment in children.8 An angiotensin-converting enzyme inhibitor or angiotensin receptor blocker is recommended as the initial agent for children with hypertension and chronic kidney disease, proteinuria, or diabetes. Because black children may be less responsive to angiotensin-converting enzyme inhibitors, a higher starting dose or a different class of medication may be considered initially for these children.36 Calcium channel blockers or hydrochlorothiazide may be chosen for an adolescent female who is at risk of pregnancy to avoid potential fetal risks from other medication classes. Children should be started on the lowest recommended dosage of antihypertensive medications, and it may be titrated up every two to four weeks until the blood pressure goal is achieved. If the goal is not achieved with the maximal dose of a single medication, a second medication with complementary action should be added.8 For more information on the pharmacologic options for hypertension in children, see eTable A and eTable B.
| Drug | Age | Initial dose | Maximal dose | Dosing interval | Formulations |
|---|---|---|---|---|---|
| ACE inhibitors | |||||
| |||||
| Benazepril | ≥ 6 y* | 0.2 mg/kg per d (up to 10 mg per d) | 0.6 mg/kg per d (up to 40 mg per d) | Daily | Tablet: 5, 10, 20, 40 mg (generic) Extemporaneous liquid: 2 mg/mL |
| Captopril | Infants | 0.05 mg/kg per dose | 6 mg/kg per d | Daily to 4 times a day | Tablet: 12.5, 25, 50, 100 mg (generic) Extemporaneous liquid: 1 mg/mL |
| Children | 0.5 mg/kg per dose | 6 mg/kg per d | Three times a day | ||
| Enalapril | ≥ 1 mo* | 0.08 mg/kg per d (up to 5 mg per d) | 0.6 mg/kg per d (up to 40 mg per d) | Daily to twice a day | Tablet: 2.5, 5, 10, 20 mg (generic) Solution: 1 mg/mL |
| Fosinopril | ≥ 6 y | Daily | Tablet: 10, 20, 40 mg (generic) | ||
| < 50 kg | 0.1 mg/kg per d (up to 5 mg per d) | 40 mg per d | |||
| ≥ 50 kg* | 5 mg per d | 40 mg per d | |||
| Lisinopril | ≥ 6 y* | 0.07 mg/kg per d (up to 5 mg per d) | 0.6 mg/kg per d (up to 40 mg per d) | Daily | Tablet: 2.5, 5, 10, 20, 30, 40 mg (generic) Solution: 1 mg/mL |
| Ramipril | NA | 1.6 mg/m2 per d | 6 mg/m2 per d | Daily | Capsule: 1.25, 2.5, 5, 10 mg (generic) |
| Quinapril | NA | 5 mg per d | 80 mg per d | Daily | Tablet: 5, 10, 20, 40 mg (generic) |
| ARBs | |||||
| |||||
| Candesartan | 1–5 y* | 0.02 mg/kg per d (up to 4 mg per d) | 0.4 mg/kg per d (up to 16 mg per d) | Daily to twice a day | Tablet: 4, 8, 16, 32 mg Extemporaneous liquid: 1 mg/mL |
| ≥ 6 y* | |||||
| < 50 kg | 4 mg per d | 16 mg per d | |||
| ≥ 50 kg | 8 mg per d | 32 mg per d | |||
| Irbesartan | 6–12 y | 75 mg per d | 150 mg per d | Daily | Tablet: 75, 150, 300 mg (generic) |
| ≥ 13 | 150 mg per d | 300 mg per d | |||
| Losartan | ≥ 6 y* | 0.7 mg/kg (up to 50 mg) | 1.4 mg/kg (up to 100 mg) | Daily | Tablet: 25, 50, 100 mg (generic) Extemporaneous liquid: 2.5 mg/mL |
| Olmesartan | ≥ 6 y* | NA | NA | Daily | Tablet: 5, 20, 40 mg Extemporaneous liquid: 2 mg/mL |
| < 35 kg | 10 mg | 20 mg | |||
| ≥ 35 kg | 20 mg | 40 mg | |||
| Valsartan | ≥ 6 y* | 1.3 mg/kg (up to 40 mg) | 2.7 mg/kg (up to 160 mg) | Daily | Tablet: 40, 80, 160, 320 mg (generic) Extemporaneous liquid: 4 mg/mL |
| Thiazide diuretics | |||||
| |||||
| Chlorthalidone | Child | 0.3 mg/kg | 2 mg/kg per d (50 mg) | Daily | Tablet: 25, 50, 100 mg (generic) |
| Chlorothiazide | Child* | 10 mg/kg per d | 20 mg/kg per d (up to 375 mg per d) | Daily to twice a day | Tablet: 250, 500 mg (generic) Suspension: 250/5 mL Extemporaneous liquid: 1 mg/mL |
| Hydrochlorothiazide | Child* | 1 mg/kg per d | 2 mg/kg per d (up to 37.5 mg per d) | Daily to twice a day | Tablet: 12.5, 25, 50 mg |
| Calcium channel blockers | |||||
| |||||
| Amlodipine | 1–5 y | 0.1 mg/kg | 0.6 mg/kg (up to 5 mg per d) | Daily | Tablet: 2.5, 5, 10 mg Extemporaneous liquid: 1 mg/mL |
| ≥ 6 y* | 2.5 mg | 10 mg | |||
| Felodipine | ≥ 6 y | 2.5 mg | 10 mg | Daily | Tablet (extended release): 2.5, 5, 10 mg (generic) |
| Isradipine | Child | 0.05–0.1 mg/kg | 0.6 mg/kg (up to 10 mg per d) | Capsule: twice daily to 3 times a day; extended releasetablet: daily | Capsule: 2.5, 5 mg Extended-release tablet: 5, 10 mg |
| Nifedipine extended release | Child | 0.2–0.5 mg/kg per d | 3 mg/kg per d (up to 120 mg per d) | Daily to twice a day | Tablet (extended-release): 30, 60, 90 mg (generic) |
| Drug | Initial dose | Maximal dose | Dosing interval |
|---|---|---|---|
| Beta blockers | |||
| Metoprolol, extended release (age > six years) | 1 mg per kg per day | 2 mg per kg per day or 200 mg per day | Daily |
| Propranolol | 1 to 2 mg per kg per day | 4 mg per kg per day or 640 mg per day | Two or three times per day |
| Central alpha-agonist | |||
| Clonidine (age ≥ 12 years) | 0.1 mg two times per day | 2.4 mg per day | Two times per day |
| Vasodilators | |||
| Hydralazine | 0.75 mg per kg per day in divided doses | 7.5 mg per kg per day or 200 mg per day | Two to four times per day |
| Minoxidil | |||
| Age < 12 years | 0.2 mg per kg per day | 50 mg per day | Daily to two times per day |
| Age ≥ 12 years | 5 mg per day | 100 mg per day | |
This article updates previous articles on this topic by Luma and Spiotta,23 and by Riley and Bluhm.37
Data Sources: We began with an initial evidence summary that included relevant POEMs, Cochrane reviews, evidence-based guidelines, and other items from Essential Evidence. A PubMed search was then done using the key terms primary hypertension, secondary hypertension, prehypertension, children, pediatrics, and adolescents. Articles referenced in the 2017 AAP Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents were reviewed. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality evidence reports, the National Guideline Clearinghouse database, and UpToDate. Search dates: August to November 2017, and February and July 2018.
