
Am Fam Physician. 2020;101(5):275-285
Related FPM article: Point-of-Care Ultrasound: A Practical Guide for Primary Care
Related letter: Formal Training in POCUS Can Positively Impact Family Medicine Practices
Author disclosure: No relevant financial affiliations.
Point-of-care ultrasonography (POCUS) is performed by a physician at the bedside and is standard practice in obstetric, emergency, and musculoskeletal medicine. When compared with formal sonography, POCUS is equivalent in screening for abdominal aortic aneurysm and as accurate in diagnosing deep venous thrombosis. POCUS has high accuracy for diagnosing pneumonia and detecting acute decompensated heart failure but is less accurate than computed tomography for identifying pulmonary embolism. POCUS confirmation of intrauterine pregnancy rules out an ectopic pregnancy. In the third trimester of high-risk pregnancies, umbilical artery Doppler ultrasonography can improve perinatal outcomes. Musculoskeletal POCUS is used to diagnose and guide treatment of many joint and soft tissue conditions. It is as accurate as magnetic resonance imaging in the diagnosis of complete rotator cuff tears. Ultrasound guidance improves outcomes in the placement of central venous catheters and fluid drainage from body cavities and lumbar punctures. Ultrasonography can reduce the use of CT for diagnosis of appendicitis; however, negative scan results do not rule out disease. POCUS can accurately diagnose and rule out gallbladder pathology, and is effective for diagnosing urolithiasis. Focused cardiac ultrasonography can detect pericardial effusion and decreased systolic function, but is less accurate than lung ultrasonography at diagnosing acute heart failure. Limited evidence demonstrates a benefit of diagnosing testicular and gynecologic conditions. The American College of Emergency Physicians, the American Institute of Ultrasound in Medicine, the Society for Academic Emergency Medicine, the American College of Radiology, and others offer POCUS training. Training standards for POCUS have been defined for residency programs but are less established for credentialing.
Point-of-care ultrasonography (POCUS) is an evolving outpatient, inpatient, and urgent care diagnostic tool. Diagnostic timing decreases, and accuracy increases when POCUS augments the clinical examination and procedures. The use of POCUS in primary care is increasing because it reduces cost, radiation exposure, and imaging delays, and increases patient satisfaction. POCUS is also useful in resource-limited settings. The instruction of POCUS is increasing in family medicine residency programs, and resources for practicing physicians exist. However, widespread POCUS use is limited by the training burden required to gain and maintain skills. This article summarizes the strongest evidence for the effectiveness of POCUS in specific clinical conditions.
Clinical Conditions with Strong, Consistent Evidence Supporting Use of POCUS
ABDOMINAL AORTIC ANEURYSM SCREENING
One-time abdominal aortic aneurysm (AAA) screening is recommended for men 65 to 75 years of age who smoked at least 100 cigarettes during their lifetime, with consideration for screening men who never smoked.1 Screening reduces aneurysm rupture mortality by 34% (number needed to screen = 311 to prevent one death).2 In a 2012 study, only 31% of eligible patients were screened and most used more costly or radiation-intense imaging.3
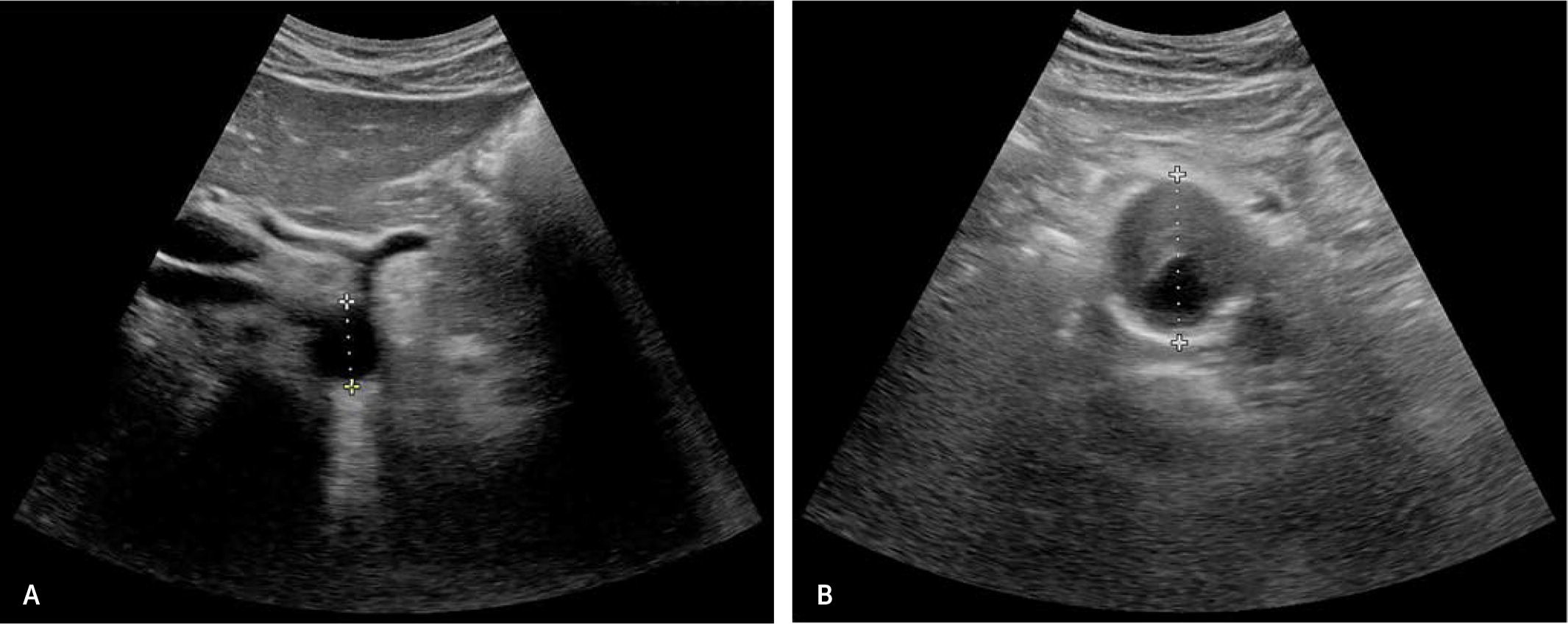
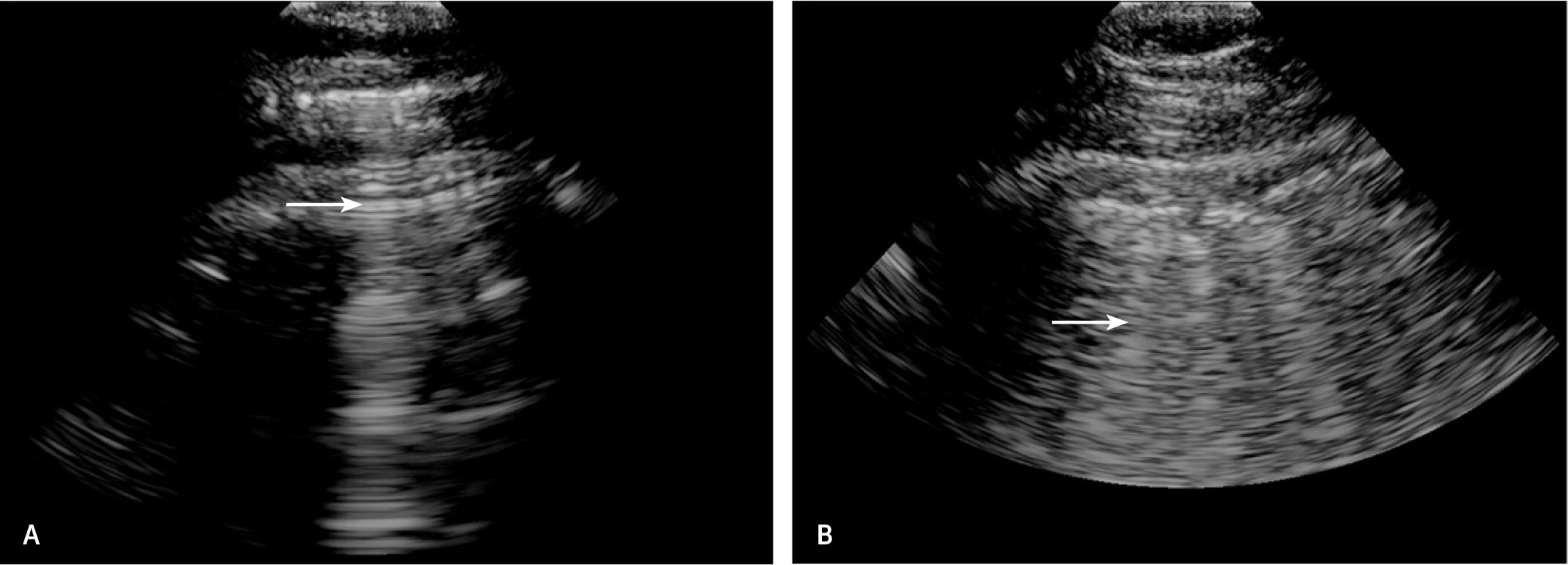
Two studies with 80 and 45 participants yielded 100% sensitivity and specificity for AAA screening with POCUS in primary care.4,5 A meta-analysis of seven emergency department POC ultrasound studies demonstrated 99% sensitivity and 98% specificity for AAA diagnosis.6 In another trial, a medical student identified 15 of 16 aneurysms in 57 patients after three hours of training; and the missed aneurysm was an inconclusive study.7 In a large study of primary care AAA screening with 25 hours of physician training, scans were completed in an average of four minutes but showed a 21% false-positive rate; however, misdiagnosed scans showed abnormalities such as aortic ectasia or luminal thrombus.8 Figure 1 shows POCUS scans of a normal abdominal aorta and an abdominal aortic aneurysm.
DEEP VENOUS THROMBOSIS
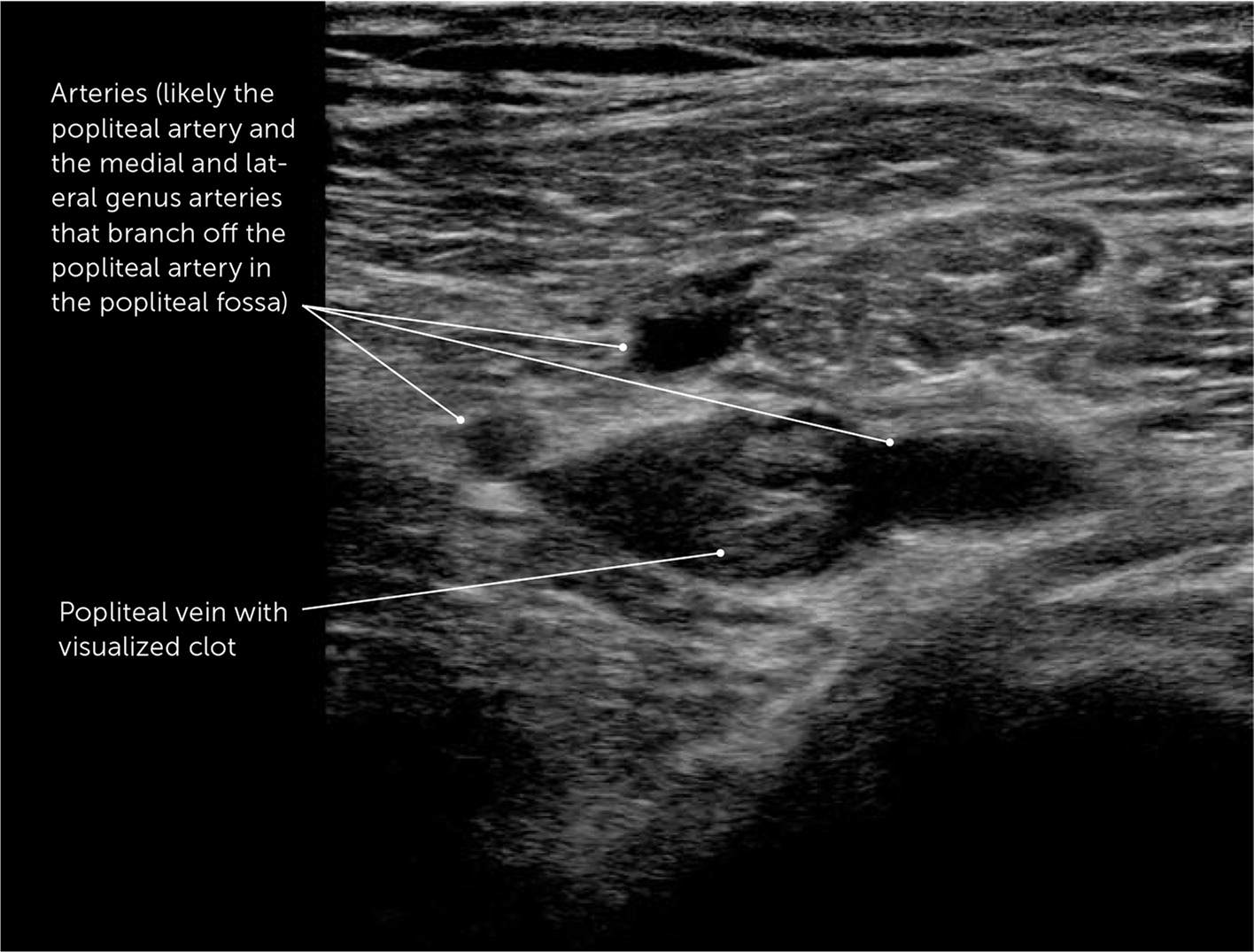
Proximal compression leg ultrasonography accurately diagnoses deep venous thrombosis (DVT).9 Emergency department POCUS of common femoral and popliteal veins have 96% sensitivity and 97% specificity for detecting DVT.9 After two hours of training, primary care physicians diagnosed DVT with 90% sensitivity and 97% specificity.10 When examinations are repeated, diagnostic accuracy approaches 100%.11 Figure 2 shows a DVT diagnosed using POCUS.
PROCEDURAL GUIDANCE
POCUS is used for guidance in many procedures and has become the standard of care for some procedures (Table 1).12–17 In central venous catheter placement, ultrasound guidance reduces complications, arterial puncture, and time to completion, and improves success.12,13 Ultrasound guidance of thoracentesis and paracentesis reduces the rate of dry taps but not the number of passes or incidence of pneumothorax.14,15 Ultrasound guidance reduces bleeding (number needed to treat [NNT] = 391),15 and prevents failure in paracentesis (NNT = 12) and reduces traumatic lumbar puncture (NNT = 7).16 For superficial skin abscess drainage, ultrasound guidance reduces treatment failure (NNT = 9).17
| Procedure | Evidence | Patients |
|---|---|---|
| Femoral central line | Only significant improvement was an increased likelihood of success with first attempt (NNT = 3)13 | 224 |
| Internal jugular central line | Reduced complication rate (NNT = 11), improved success rate (NNT = 10), reduced arterial puncture (NNT = 17), and reduced other complications (NNT = 67) while reducing time for the procedure by 30 minutes12 | 4,340 |
| Lumbar puncture | Prevent failed procedure (NNT = 12); prevented traumatic procedure (NNT = 7)16 | 957 |
| Paracentesis | Reduction of bleeding (NNT = 391)15 | 69,859 |
| Skin and soft tissue abscess incision and drainage | Reduction in failure rate of abscess drainage (NNT = 9)17 | 239 |
| Subclavian central line | Only significant improvement was reduced arterial puncture (NNT = 22)13 | 499 |
| Thoracentesis | Lower risk of dry tap with ultrasonography (odds ratio = 0.11) but no reduction in number of passes or in pneumothorax14 | 208 |
Numerous musculoskeletal procedures are performed with POCUS guidance, including joint and soft tissue aspiration, injections, and nerve blocks. Ultrasonography is becoming a standard of care for some interventions.18 Ultrasound guidance reduces procedural pain scores by an average of −0.5 to −2 on a 10-point scale for subacromial, bicep tendon sheath, glenohumeral, and knee joint injections.19,20 Ultrasound guidance during knee arthrocentesis reduces pain by more than 50%.21 In nerve blocks, ultrasound guidance reduces the number of inadequate blocks (NNT = 9), paresthesia (NNT = 11), and vascular puncture (NNT = 14).22 Table 2 summarizes the benefits of ultrasound guidance in musculoskeletal procedures.19–23
| Procedure | NNT to prevent missing target | Patient outcome |
|---|---|---|
| Biceps tendon sheath injection | 2 | Average pain score improvement of 1.9 out of 10 and function improvement of 1.1 out of 1019 |
| Carpal tunnel injection | Not reported | Average reduction of 0.5 points in 11-point symptom severity score and no difference in function or electrodiagnostic results23 |
| Glenohumeral joint injection | 5 | Average pain score improvement of 0.6 out of 10 and no functional difference in adhesive capsulitis19 |
| Knee arthrocentesis | 7 | Average procedural pain score reduction of 2.2 out of 1021 |
| Knee injection | 6 | 26% increase in responders with at least 50% pain reduction20 |
| Nerve blocks | NA | Prevent inadequate block (NNT = 9), prevent paresthesia around block (NNT = 11), prevent vascular puncture (NNT = 14)22 |
| Subacromial injection | 20 | Average pain score improvement of 1.5 out of 10 at six weeks and functional benefit at six weeks (NNT = 3)19 |
RESPIRATORY DISTRESS
The bedside lung ultrasound in emergency (BLUE) protocol was developed to categorize findings in acute respiratory distress24,25 (eTable A). In lung ultrasonography, A lines are artifacts running parallel to pleura in healthy lung tissue (Figure 3A), whereas B lines are comet-tail artifacts found perpendicular to pleura from subpleural edema24 (Figure 3B). Ultrasound findings are combined with clinical evaluation; unilateral B lines with fever and cough correlate with pneumonia, and bilateral A lines with wheezing suggest obstructive airway disease given that lung parenchyma is normal in bronchial obstruction.24 POCUS of the lung is more sensitive than plain radiography in diagnosing other conditions, such as pleural effusion (94% sensitivity) and pulmonary contusion (92% sensitivity).26,27 POCUS of the lung decreases emergency department diagnostic time by two hours on average compared with standard radiography, computed tomography (CT), or echocardiography.25
| Diagnosis | Lung ultrasound findings | Sensitivity | Specificity | Positive likelihood ratio | Negative likelihood ratio |
|---|---|---|---|---|---|
| Asthma or chronic obstructive pulmonary disease | A lines (healthy lung) | 87% | 96% | 22 | 0.14 |
| Fluid overload | B lines | 88% | 96% | 22 | 0.12 |
| Pneumonia | One of the following findings: B lines with no lung sliding* B lines in one lung only Visualized area of consolidated lung | 88% | 92% | 10 | 0.13 |
| Pneumothorax | A lines with no lung sliding* and a possible focal area of lung consolidation | 88% | 100% | 4,600 | 0.12 |
| Pulmonary embolism | A lines (normal lung) with diagnosed deep venous thrombosis | 40% | 99.9% | 345 | 0.60 |
Although lung ultrasonography is less accurate than CT angiography for diagnosis of pulmonary embolism, POCUS can be valuable if CT is unavailable or contraindicated. A healthy lung ultrasound has a negative likelihood ratio (LR–) of 0.18, compared with a LR– of 0.36 for a low-probability ventilation-perfusion scan and a LR– of 0.11 for a negative CT angiogram.28,29 With a moderate-risk Wells score, a negative lung ultrasound reduces pulmonary embolism probability from 16% to 5% and a positive lung ultrasound increases pulmonary embolism probability to 55%.28
ROTATOR CUFF TEAR
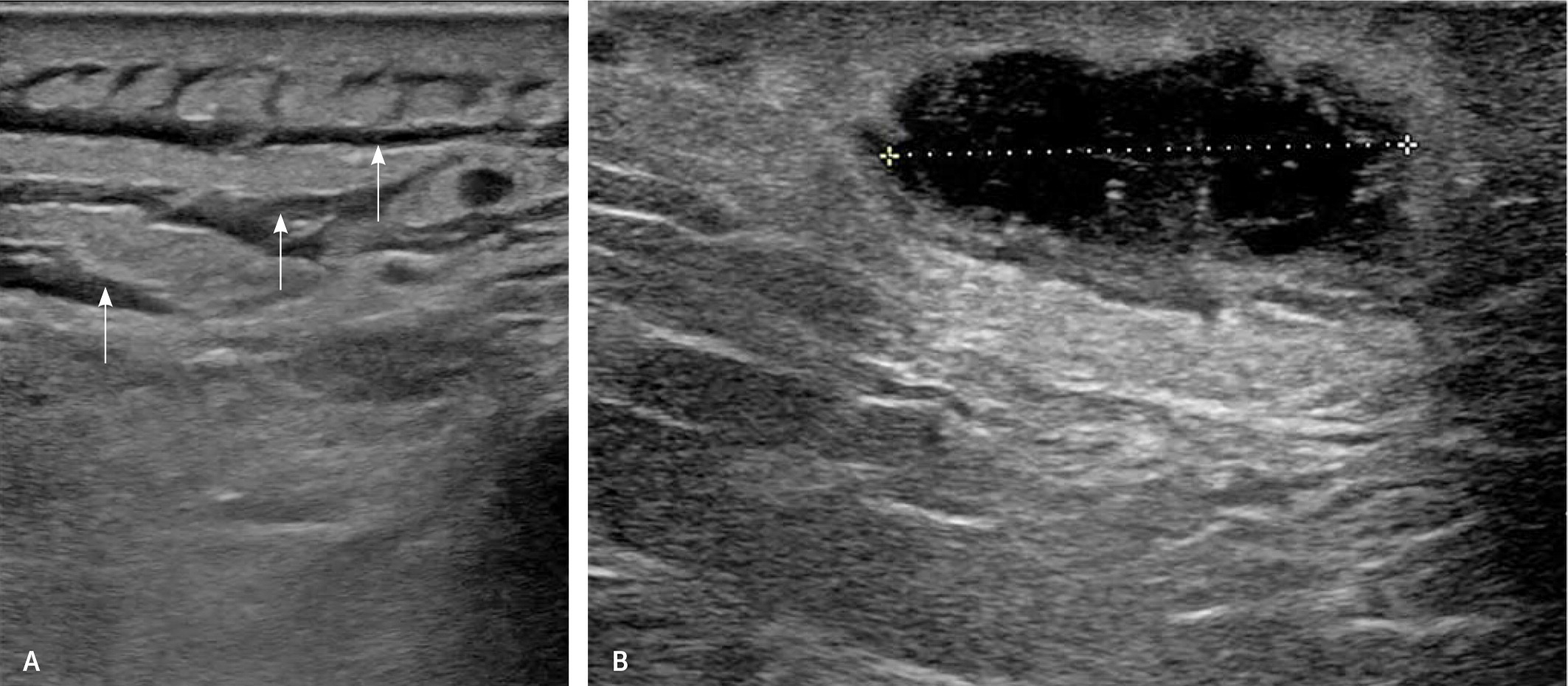
A Cochrane review of 20 studies of POCUS and formal sonography involving 1,147 shoulders demonstrated ultrasonography can diagnose full-thickness rotator cuff tears with equivalent accuracy to magnetic resonance imaging (MRI).30 For partial-thickness rotator cuff tears and subacromial conditions, ultrasonography is less accurate than MRI.30,31 Table 3 describes the accuracy of ultrasonography for shoulder conditions.30–33 Figure 4 shows a POCUS scan of a complete rotator cuff tear.34
| Condition | Musculoskeletal ultrasonography | MRI | ||
|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Calcifying tendinitis | 100% | 85% to 98% | 98% | 96% |
| Full thickness rotator cuff tear | 92%* | 93% | 94%* | 93% |
| Partial thickness rotator cuff tear | 52% | 93% | 74% | 93% |
| Subacromial bursitis | 79% to 81% | 94% to 98% | Not reported, higher than ultrasonography | |

SKIN AND SOFT TISSUE INFECTIONS
Without imaging, differentiating cellulitis from an abscess can be difficult because clinical examinations can be incorrect in up to 22% of cases, delaying resolution and increasing risk.35 A systematic review showed that POCUS reduces the failure-to-diagnose rate because negative scan results have a LR– of 0.05 for abscess.36 POCUS also decreases inappropriate incision and drainage of cellulitis without abscess by up to 20% compared with clinical examinations.36 One study demonstrated 86% sensitivity for diagnosing abscess with POCUS, compared with 77% for CT.37 Ultrasonography also effectively rules out foreign bodies that can delay healing. In a small study, a normal POCUS scan had a 96% negative predictive value for subcutaneous foreign bodies.38 Figure 5 shows POCUS scans of cellulitis and abscess.
Clinical Conditions with Moderate Evidence Supporting Use of POCUS
APPENDICITIS
POCUS has been studied to reduce CT imaging in suspected appendicitis. The pooled sensitivity of POCUS for appendicitis is 91% when performed by surgeons and physicians who work in the emergency department.39 A meta-analysis of POCUS performed by emergency department physicians showed 84% sensitivity and 91% specificity, with higher accuracy in children. 40 Ultrasonography can confirm appendicitis; however, a negative ultrasound does not rule out disease because perforated appendicitis is often missed because of findings including loculated fluid collections, dilated bowel, appendicoliths, and increased liver echogenicity.41 In children, a negative ultrasound with a low-risk clinical decision score sufficiently rules out appendicitis.42
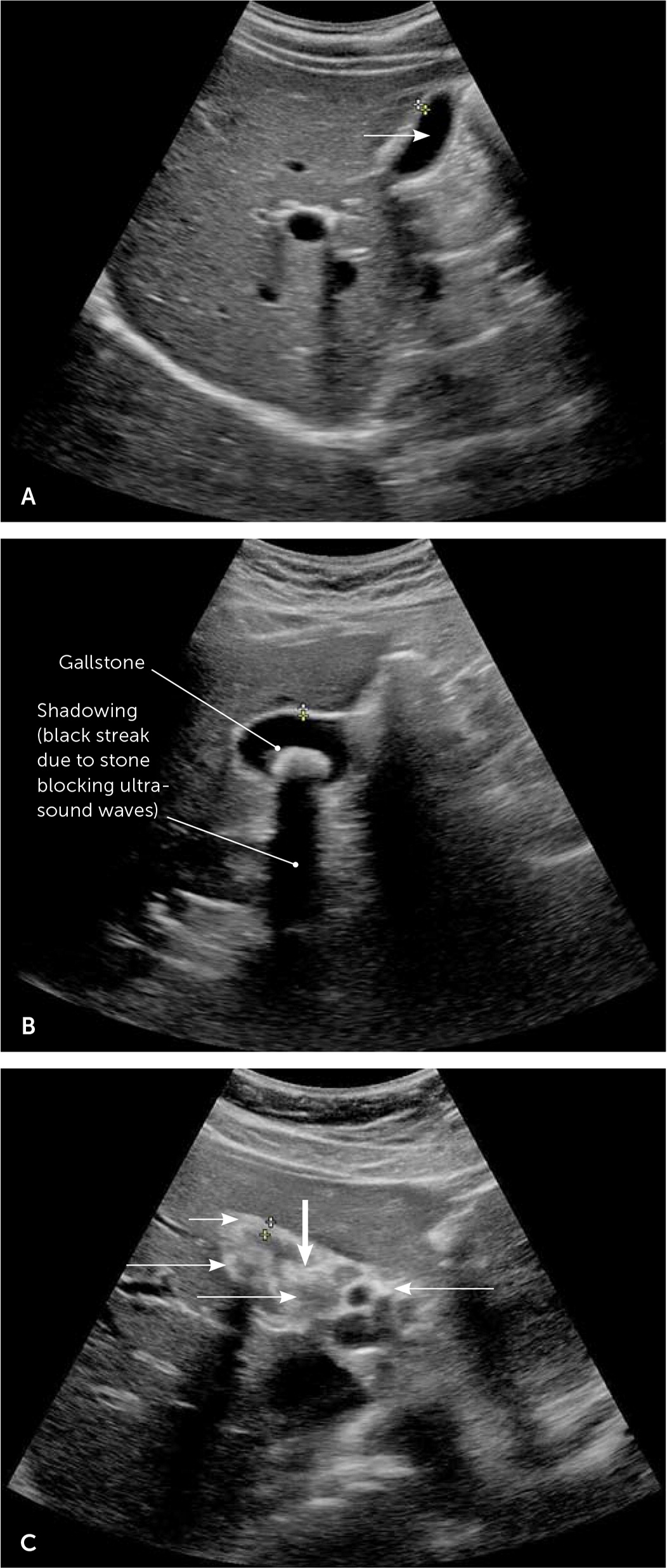
BILIARY COLIC
Biliary ultrasonography aids cholecystitis diagnosis in suspected biliary colic. POCUS has 90% sensitivity and 88% specificity compared with CT or surgical findings.43 In comparison, CT has 92% sensitivity.44 Diagnostic accuracy is nearly 100% when gallstones are found with gallbladder wall thickening and pericholecystic fluid or sludge (Table 4).45 POCUS is highly accurate at diagnosing gallstones; however, cholecystitis occurs without stones in 14% of cases.46 Figure 6 shows biliary POCUS findings.
| Sensitivity | Specificity | |
|---|---|---|
| Individual findings | ||
| Gallstones | 84% | 49% |
| Gallbladder wall thickening | 54% | 92% |
| Pericholecystic fluid | 23% | 98% |
| Sludge in gall bladder | 23% | 91% |
| Common bile duct dilation | 21% | 88% |
| Combinations of findings | ||
| Gallstones and gallbladder wall thickening | 54% | 93% |
| Gallstones and sludge and gallbladder wall thickening | 23% | 100% |
| Gallstones and common bile duct dilation and gallbladder wall thickening | 16% | 99% |
| Gallstones and pericholecystic fluid and gallbladder wall thickening | 16% | 100% |
BOWEL PERFORATION
Free abdominal air can create ultrasound artifacts, including anterior echogenic lines, and internal echoes within fluid and resonance artifacts. In one study, POCUS had 92% sensitivity in the detection of free air compared with 78% for upright chest radiography; both had 53% specificity.47
DECREASED CARDIAC EJECTION FRACTION
Focused cardiac ultrasound sensitivity for decreased cardiac ejection fraction varies from 74% to 94%.48 In most studies, cardiac ultrasonography is less sensitive for the diagnosis of acute decompensated heart failure than the 88% sensitivity of lung ultrasonography.49 Yet, evidence supports the use of focused cardiac ultrasonography for gross cardiac function estimation. A study of 50 patients admitted for acute decompensated heart failure showed that residents found ejection fraction in less than 40% of patients with 94% sensitivity and specificity.50 In another study, emergency medicine residents missed decreased systolic function one-half of the time.51 E-point septal separation (EPSS) is the measurement of the minimal separation of the anterior mitral valve leaflet and the ventricular septum, which corresponds to ejection fraction. In a study with 80 patients, EPSS diagnosed ejection fraction at 30% or less with 100% sensitivity but only 44% positive predictive value, attributed to false positives.52
ELEVATED INTRACRANIAL PRESSURE
Optic nerve sheath diameter measured with POCUS enables noninvasive detection of elevated intracranial pressure, with 90% sensitivity and 85% specificity.53
INTERNAL BLEEDING IN TRAUMA
The focused assessment with sonography for trauma (FAST) examination represents one of the first POCUS protocols and has replaced diagnostic peritoneal lavage (DPL) for detection of internal bleeding. A Cochrane review found 74% sensitivity and 96% specificity for thoracoabdominal bleeding.54
OBSTETRIC AND GYNECOLOGIC CONDITIONS
Ultrasonography is standard in pregnancy management. Many obstetric parameters, such as first-trimester dating, amniotic fluid levels, fetal position, and antepartum testing, are defined with ultrasonography. Ultrasonography is required to diagnose placental abnormalities. Visualization of intrauterine pregnancy rules out ectopic pregnancy with a LR– of 0.08.55
A Cochrane review found that screening the umbilical artery with Doppler ultrasonography reduces the risk of perinatal death (number needed to screen = 203) when performed during the third trimester in a high-risk pregnancy attributed to diabetes mellitus, hypertensive disorders, or other issues increasing perinatal mortality risk.56 The review could not define which intervention or protocol triggered by an abnormal Doppler study is the preferred method to reduce mortality. Recent evidence verifies ultrasound screening at 36 weeks of gestation is effective in determining breech presentation.57
POCUS is used to evaluate pelvic pain and vaginal bleeding in women; however, accuracy has not been studied. POCUS effectively evaluates intrauterine device placement, but accuracy has not been assessed.58
PERICARDIAL EFFUSION
Focused cardiac ultrasonography includes limited cardiac views and specific measurements to obtain functional information on the dynamic heart. Focused cardiac ultrasonography is most effective in detecting pericardial effusion, with 100% sensitivity in one study.59 Reproducibility of focused cardiac ultrasonography was questioned by another study demonstrating that residents in emergency medicine miss pericardial effusion one-half of the time.51 Demonstration of effusion and tamponade can be lifesaving despite limitations.
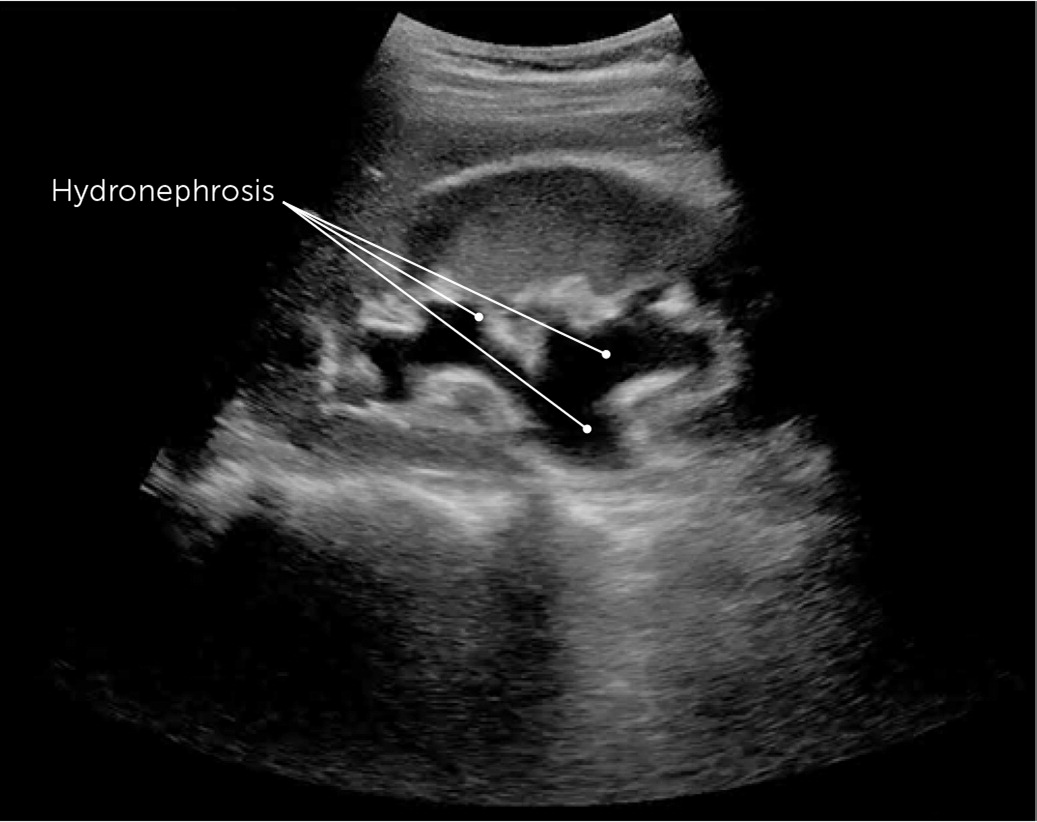
RENAL COLIC
POCUS can identify urolithiasis and hydronephrosis with 70% sensitivity and 75% specificity in suspected renal colic. Finding at least moderate hydronephrosis increases specificity to 94%.60 Hydronephrosis identification is improved with increased physician ultrasound experience.61 A large multicenter trial showed that the emergency department POCUS evaluation of suspected urolithiasis produced equivalent clinical outcomes to CT evaluation.62 Figure 7 shows hydronephrosis attributed to urolithiasis on renal ultrasonography.
RETINAL DETACHMENT
Retinal detachment can be diagnosed with 97% sensitivity, but 83% specificity because retinal detachment can be confused with a benign vitreal detachment in older adults.63
Clinical Conditions with Limited Evidence Supporting Use of POCUS
SCROTAL PAIN
A study with 36 patients showed that a POCUS examination of acute scrotal pain identified testicular torsion with 95% sensitivity and 94% specificity.64
MUSCULOSKELETAL CONDITIONS OUTSIDE THE SHOULDER
Ultrasonography is often used to diagnose musculoskeletal conditions because of its ability to localize patient conditions and perform a dynamic assessment, but data comparing musculoskeletal ultrasonography to other radiologic modalities is limited. Most studies are small and compare ultrasonography to clinical examination findings, but the evidence is emerging for soft tissue structures.65 A systematic review found plantar fascial thickness of 4 mm or greater on ultrasonography is diagnostic for plantar fasciitis.66 In a study of 45 patients, complete and partial distal biceps tendon tears were diagnosed using POCUS with 95% sensitivity compared with surgical findings.67
FRACTURE
Ultrasonography is less accurate than plain radiography for extremity fractures but is useful when radiography is unavailable.68 POCUS can diagnose extremity fractures with 85% sensitivity and 73% specificity compared with plain radiography.69 A small study suggests POCUS diagnoses rib fractures with 63% sensitivity, with feasibility limited by pain.70
Training and Competency
POCUS is being integrated into medical school and residency curricula. The American Academy of Family Physicians recommends ultrasound guidelines emphasizing a faculty champion with curricula including didactics, hands-on learning, and assessment.71 These guidelines recommend 150 to 300 reviewed scans for general competency, 25 to 50 scans for any specific examination, and five to 10 scans for ultrasound procedural guidance, and are based on emergency medicine requirements.71 For musculoskeletal applications, the American Institute of Ultrasound in Medicine recommends 50 diagnostic and 50 ultrasound-guided procedures.18
For credentialed physicians, POCUS accreditation is less clear. Numerous instructional resources teaching ultrasound skills are available, including many that are free (Table 571,72). Certificate programs for nonmusculoskeletal POCUS are offered by the American College of Chest Physicians and the Alliance for Physician Certification and Advancement. The American Institute of Ultrasound in Medicine and the American College of Radiology offer accreditations in musculoskeletal ultrasonography.18,71,72 The American Board of Family Medicine does not currently recognize certification in POCUS, so credentialing decisions are deferred to privileging hospitals.71 The American Institute of Ultrasound in Medicine recommends 50 procedures annually and dedicated continuing medical education for physicians to maintain ultrasound skills.18 No other organizations have specific recommendations for maintaining privileges.
| Resource | Cost | Comments |
|---|---|---|
| 5 Min Sono http://5minsono.com/ | Free | Collection of short videos demonstrating examinations; podcast |
| American College of Emergency Physicians Sonoguide https://www.acep.org/sonoguide/introduction.html | Free | Web-based curriculum of test-based descriptions with photos and videos; referenced by Ultrasound Ninja curriculum |
| American Institute of Ultrasound in Medicine https://www.aium.org | Prices vary by course and continuing medical education credits | Collection of continuing medical education materials for ultrasound certification; credentialing program recommending 50 credits in each body area |
| European Society of Musculoskeletal Radiology https://www.essr.org | Free | Webinars for radiology topics; not focused solely on ultrasonography |
| Massachusetts General Hospital Emergency Ultrasound Educational Website https://sites.google.com/site/mghedus/home | Free | Free video tutorials on emergency ultrasound topics |
| Point-of-Care Ultrasound Certification Academy https://pocus.org/ | $125 for fundamental certification, $150 for each of 10 clinical area certificates, $625 for emergency medicine certification with seven clinical areas | Certification programs including examination and certificate |
| Society for Academic Emergency Medicine https://www.saem.org/education/saem-online-academic-resources/topics/ultrasound | Varies by membership level | Faculty performing and teaching emergency ultrasonography; includes modules for physicians at different levels of experience |
| SonoSpot: Topics in Bedside Ultrasound http://sonospot.com/ | Free | Tutorials with verbal descriptions for probe placements and photos; short videos of ultrasound images showing expected results |
| Ultrasound Ninja http://www.ultrasoundninja.com/ | Free | Emergency medicine ultrasound program; curriculum consisting of podcasts and references for each curricular element; free e-book |
| Virtual Transthoracic Echocardiography Website http://pie.med.utoronto.ca/TTE/index.htm | Free | Tutorial for performing transthoracic echocardiography |
Editor's Note: Dr. Arnold is the medical editing fellow for AFP.
Data Sources: A PubMed search was completed using the key terms point-of-care ultrasound, focused cardiac ultrasound, ultrasound credentialing, musculoskeletal ultrasound, and bedside ultrasound. After the significant injuries and diagnoses were identified, searches were performed for each modality. The searches included systemic reviews, meta-analyses, randomized controlled trials, and review articles. Also searched were the Cochrane database, Essential Evidence Plus, and Clinical Evidence. Also, references in these resources were searched. Search dates: January to March 2019, June 2019, and December 2019.
The views expressed in this article are those of the authors' and do not reflect the official policy or position of the Department of the Army, Department of the Navy, Department of the Air Force, Uniformed Services University of the Health Sciences, Department of Defense, or the U.S. government.
