
Am Fam Physician. 2022;105(6):631-639
Patient information: See related handout on exercising your finger after an injury.
Author disclosure: No relevant financial relationships.
Finger fractures and dislocations are commonly seen in the primary care setting. Patients typically present with a deformity, swelling, and bruising with loss of function. Anteroposterior, lateral, and oblique radiography should be performed to identify fractures and distinguish uncomplicated injuries from those requiring referral. Uncomplicated distal phalanx fractures, caused by a crush injury to the end of the finger, require splinting of the distal interphalangeal joint for four to six weeks. Uncomplicated dorsal avulsion fractures (mallet finger) of the distal interphalangeal joint, caused by forced flexion against resistance, require strict splint immobilization for eight weeks. Flexor digitorum profundus fractures are caused by forceful extension of the distal interphalangeal joint when in a flexed position, resulting in an avulsion fracture at the volar base of the distal phalanx, and usually require surgery. Uncomplicated middle and proximal phalanx fractures, typically caused by a direct blow, can be treated with buddy splinting if there is minimal angulation (less than 10 degrees); however, larger angulations, displacement, and malrotation often require reduction or surgery. Dorsal proximal interphalangeal joint dislocations require reduction and buddy splinting in slight flexion with an extension-block splint. Volar proximal interphalangeal joint dislocations require reduction and splinting in full extension for four to six weeks. Distal interphalangeal joint dislocations require reduction and splinting in full extension (for volar dislocations) or 15 to 30 degrees of flexion (for dorsal dislocations) for two to three weeks. Dorsal metacarpophalangeal joint dislocations are managed with reduction and splitting, but referral to an orthopedic specialist is required if the dislocation is not easily reduced. Volar metacarpophalangeal dislocations are rare and warrant referral.
Fractures
| Type of fracture | History/evaluation | Management | Follow-up | Indications for referral | Common complications |
|---|---|---|---|---|---|
| Distal phalanx fracture | Common in crush or axial load injuries Swelling, deformity, or subungual hematoma may be noted Radiography | Splint with DIP joint in full extension for 4 to 6 weeks U-shaped padded aluminum splint, fingertip guard, or volar splint | Every 2 weeks May take 4 to 6 weeks to heal | Open fracture (consider with subungual hematoma) Angulated or difficult-to-reduce transverse fractures Nonunion Inability to flex or extend the DIP joint or loss of distal sensation | Chronic hyperesthesia or swelling Nonunion |
| Dorsal avulsion fracture or extensor tendon rupture (mallet finger) | Axial load injury while DIP joint is in extension (forceful flexion) Slight flexion at rest may be noted Radiography | Splint with DIP joint in full extension to slight hyperextension for 8 weeks Premature joint flexion can prolong recovery Dorsally padded aluminum splint, volar splint, or thermoplastic stack splint | Every 2 weeks May take 6 to 10 weeks to heal | > 30% intra-articular involvement Open fracture Inability to passively extend the joint | Extension lag (lack of full extension) |
| Flexor digitorum profundus avulsion fracture (jersey finger) | Injury caused by forceful extension of the DIP joint when in a flexed position Radiography | Expedited referral for surgery (may splint with proximal interphalangeal and DIP joints in slight flexion until surgery evaluation) DIP joint may be in slight extension at rest | Recovery may take 6 to 12 weeks Extensive hand therapy | All flexor digitorum profundus avulsion fractures require referral for surgery | Contractures of the flexor digitorum profundus (flexion deformities) |
| Middle or proximal phalanx fracture | Direct blow or axial load injury Evaluation for malrotation Radiography | Reduce if indicated Buddy taping for 3 to 4 weeks if minimally angulated Ulnar or radial gutter splint if fracture had to be reduced (Figure 5); perform postreduction radiography in splint | Repeat radiography in 7 to 10 days to evaluate for alignment Follow-up every 2 weeks May take 4 to 6 weeks to heal | Open fracture Intra-articular, oblique, spiral, and rotational fractures Malrotation | Malunion (includes malrotation and rotation) Nonunion |
DISTAL PHALANX
Distal phalanx fractures are typically the result of a crush or axial load injury (i.e., direct force to the end of the finger). Physical examination usually shows swelling, bruising, or a subungual hematoma. Radiography demonstrates the location and degree of the bony injury.
It is important to assess the patient's ability to fully flex and extend the distal interphalangeal (DIP) joint. Distal sensation should also be evaluated. The inability to flex or extend the joint, loss of distal sensation, and complex fractures warrant evaluation by an orthopedic specialist.
DORSAL AVULSION FRACTURE OR EXTENSOR TENDON RUPTURE (MALLET FINGER)
Mallet finger occurs when the DIP joint is forced to flex against resistance (Figure 15). This can cause avulsion of the extensor tendon from its attachment at the dorsal base of the distal phalanx, with or without avulsion of a bone fragment at the end of the tendon.6 Absence of a bony avulsion indicates a pure tendon rupture.
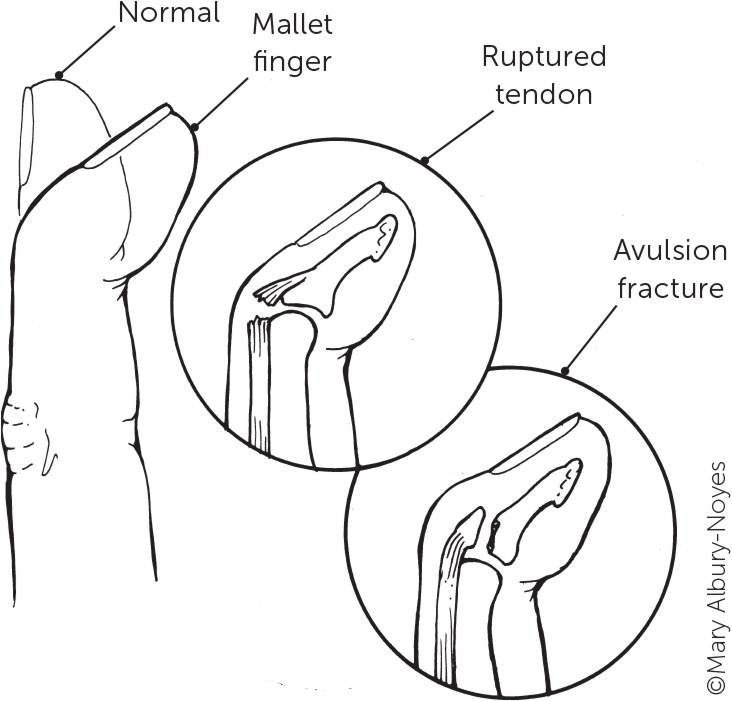
Patients with mallet finger have swelling, bruising, pain, and the inability to actively extend the DIP joint, which is typically slightly flexed due to the unopposed flexor tendon. Radiography is needed to evaluate intra-articular involvement because injuries involving greater than one-third of the joint surface require referral for possible surgical repair. Injuries in which the joint cannot be passively extended require referral to an orthopedic specialist.7
FLEXOR DIGITORUM PROFUNDUS AVULSION FRACTURE
A flexor digitorum profundus avulsion fracture (jersey finger) is typically caused by forceful extension of the DIP joint when in a flexed position (Figure 25). This forceful extension leads to an avulsion fracture at the site where the flexor digitorum profundus tendon attaches to the volar base of the distal phalanx.5 Although flexor digitorum profundus avulsion fractures can occur in any finger, they most commonly affect the ring finger.

The examination usually reveals swelling, volar-sided pain, and a slightly extended finger when at rest, and patients are usually unable to actively flex the DIP joint.12 These findings alone (regardless of radiography results) require expedited referral to an orthopedic specialist because flexor digitorum profundus avulsion fractures can benefit from surgery within seven to 10 days.
MIDDLE OR PROXIMAL PHALANX
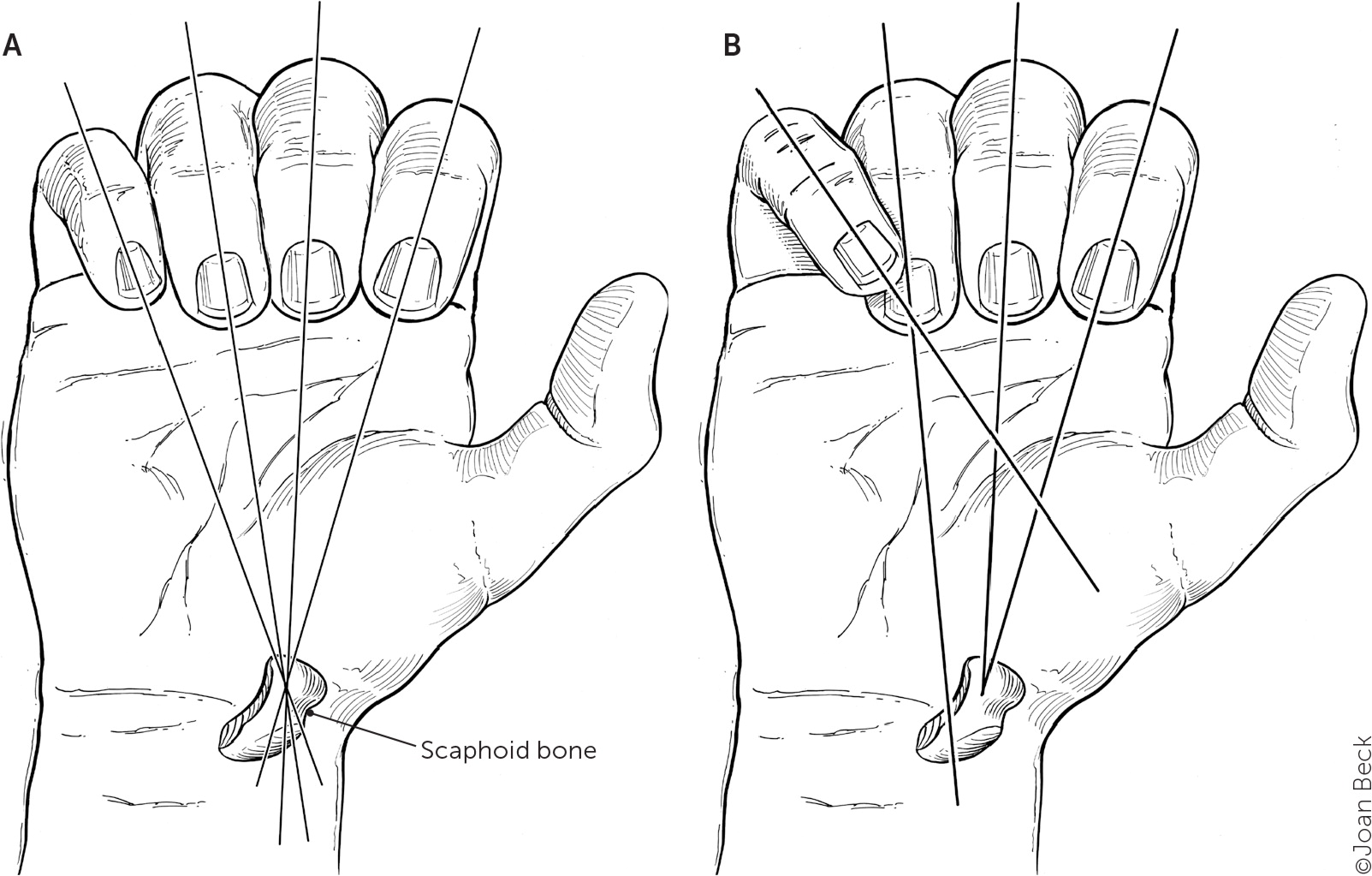
Middle or proximal phalanx fractures are typically due to a direct blow or an axial load injury. Examination reveals swelling, bruising, tenderness, and occasionally deformity. Clinicians should evaluate for malrotation by having the patient attempt to make a fist. If a phalanx is malrotated, there will be an overlap deformity when flexing the affected digit into a fist (Figure 314). Comparison to the uninjured hand can be helpful. If malrotation is present, referral for surgery is indicated.14–16
Radiography is needed to detect oblique, spiral, displaced, or rotational fractures that may not have been detected on examination and to determine if a fracture is intra- or extra-articular. Intra-articular, oblique, spiral, and rotational fractures typically require referral for surgery.14
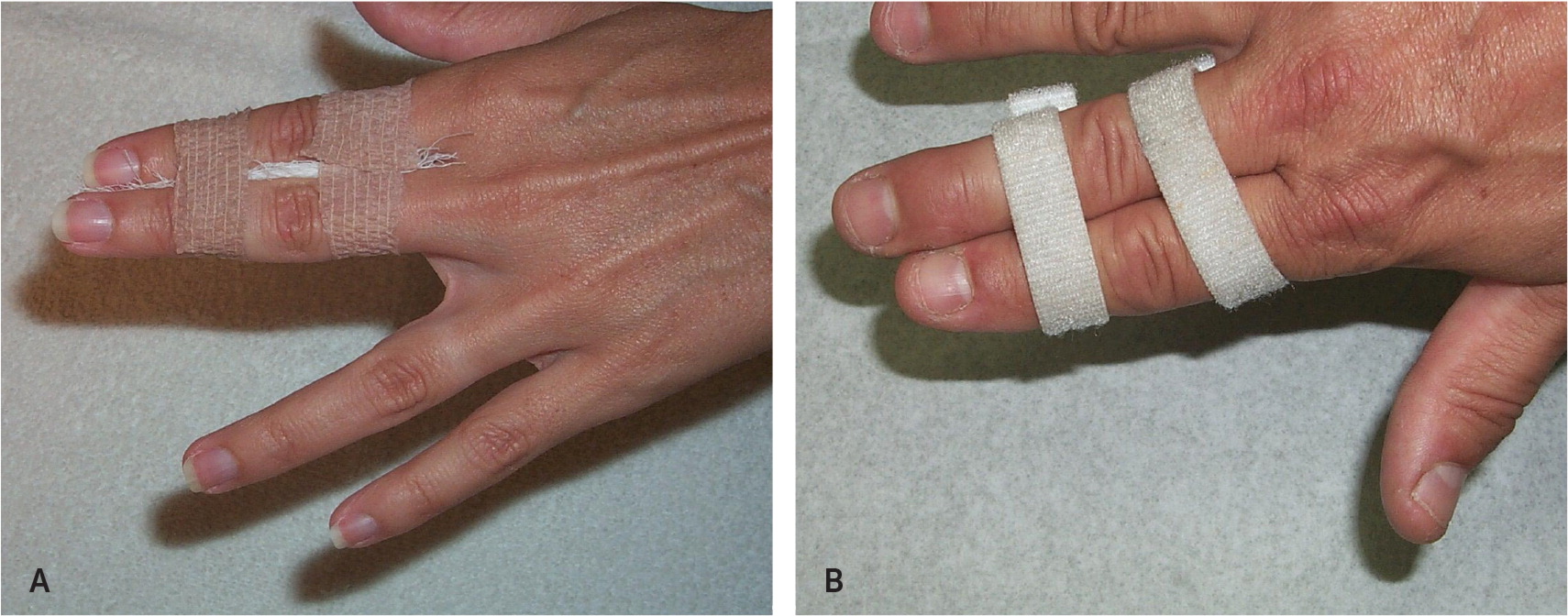
Minimally angulated (less than 10 degrees) extra-articular fractures without indications for referral can be managed in the primary care setting. Stabilization is achieved by buddy taping the fractured phalanx to the adjacent finger for three to four weeks, based on the return of comfortable function15 (Figure 45). Taping between the PIP and metacarpophalangeal (MCP) joints serves as a dynamic splint that allows free movement and prevents tendinous complications.
More severely angulated and displaced fractures can also be managed in primary care settings if the clinician is comfortable performing the reduction procedure. Reduction involves applying traction on the distal portion of the phalanx and guiding the bone back into place. Reduction commonly requires oral analgesics or a digital or hematoma block. Postreduction radiography should be performed to confirm successful realignment. Reduced fractures have a higher risk of becoming displaced or angulated during the healing process and therefore require immobilization with an ulnar or radial gutter splint, depending on the affected digit (Figure 517).

Dislocations
Finger joint dislocations are usually hyperextension injuries caused by an object striking the finger. Examination usually reveals significant tenderness, especially around the volar surface of the joint, edema, and ecchymoses. Anteroposterior, lateral, and oblique radiography is performed for the initial assessment of the injury and postreduction.2,14 Dislocations are described by the positioning of the distal phalanx relative to the proximal phalanx. Diagnosis and management recommendations for dislocations are outlined in Table 2.
| Joint involved | History/evaluation | Management | Follow-up | Indications for referral | Common complications |
|---|---|---|---|---|---|
| Distal interphalangeal | Crush injury (usually an object hits the finger causing hyperextension or hyperflexion) Evaluation for tenderness of the dorsal or volar surface Radiography | Reduce and use dorsal extension-block splint for 2 to 3 weeks | 2 to 3 weeks Start range-of-motion exercise program if no complications | Open wound Dislocation > 3 weeks old or unable to reduce Fracture involving > 30% intra-articular surface | Extensor or flexor tendon rupture Swan neck deformity Chronic hyperesthesia or edema Recurrent instability |
| Proximal inter-phalangeal | Direct blow causing hyperextension injury and usually dorsal dislocation Radiography Evaluation for central slip disruption Evaluation for tenderness of the volar plate | Reduce and buddy tape for 3 to 6 weeks Dorsal: extension-block splint at 20 to 30 degrees of flexion for 2 to 3 weeks Volar: dorsal splint in full extension for 4 to 6 weeks | Every 2 to 4 weeks depending on severity May take up to 12 to 18 months to heal | Open wound Irreducible Avulsion fracture involving > 30% intra-articular surface, complex fractures Medial or lateral dislocations | Stiffness or loss of function Boutonniere deformity (volar) Volar plate laxity or hyperextension deformity Recurrent instability |
| Metacarpophalangeal (excluding thumb) | Direct blow causing hyperextension injury and usually dorsal dislocation Radiography | Reduce and splint Dorsal: dorsal extension-block splint at 30 to 60 degrees of flexion for 7 to 10 days Lateral: dorsal extension-block splint flexed at 30 to 60 degrees for 3 weeks | Every 2 to 3 weeks until functional | Open dislocation Irreducible or complex Volar dislocation or significant lateral dislocations Avulsion fractures involving > 20% of the joint surface or > 2 mm displacement | Stiffness or loss of function Recurrent instability |
PIP JOINT: DORSAL
Finger dislocations usually involve the PIP joint, and dorsal (hyperextension) dislocations are most common. A specific injury in a dorsal dislocation is damage to the volar plate, a thick ligamentous structure on the palmar or volar surface of the PIP joint. Hyperextension can tear the volar plate, or tension applied to the volar plate can cause fracturing of the middle phalanx's proximal volar lip.14 If untreated, the volar plate shortens and thickens, resulting in a flexion deformity of the PIP joint.18
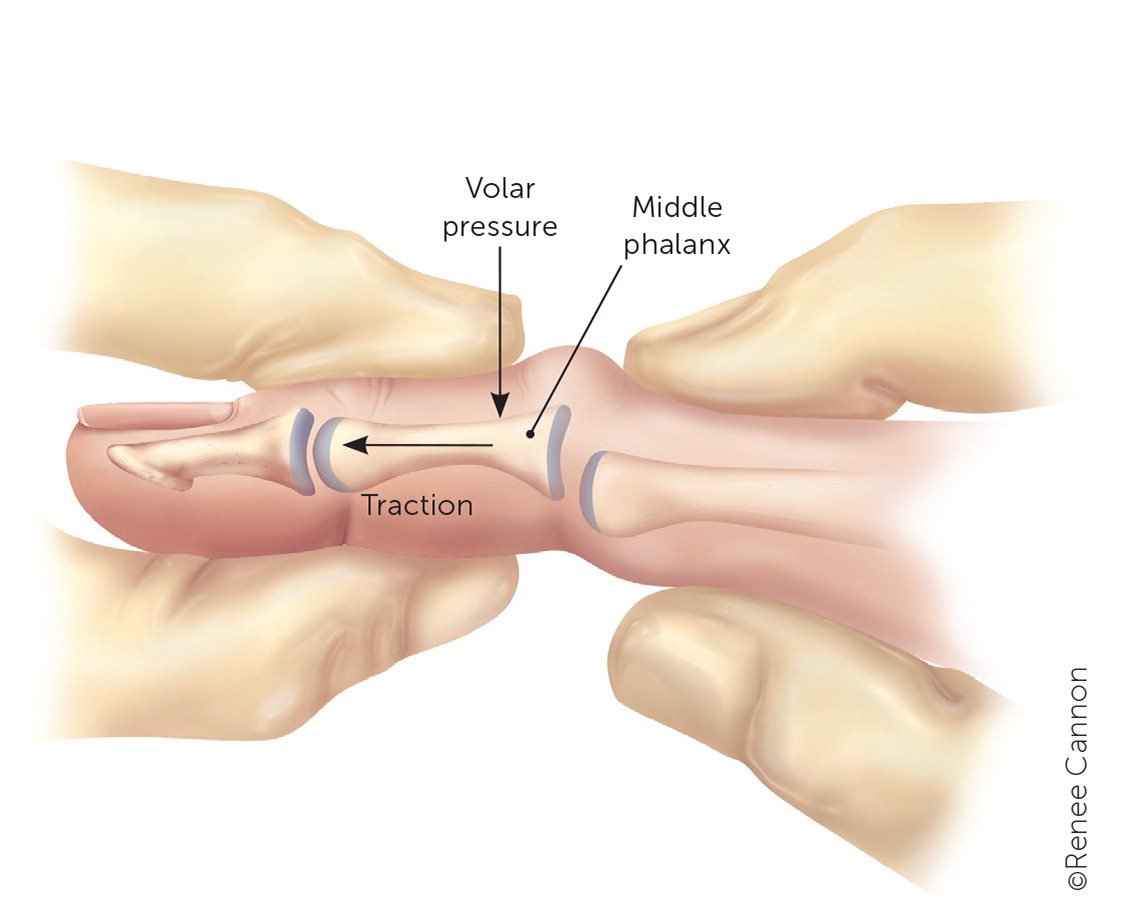
Reduction of a dorsal PIP joint dislocation involves firmly grasping the middle and proximal phalanges while applying gentle traction across the joint (Figure 619). The PIP joint is hyperextended to reapproximate the articular surface and then slowly flexed to the anatomic position. The volar plate should be palpated to ensure no tenderness is present. If a volar plate injury is suspected, splinting is recommended for four to six weeks, then advancing motion as tolerated.
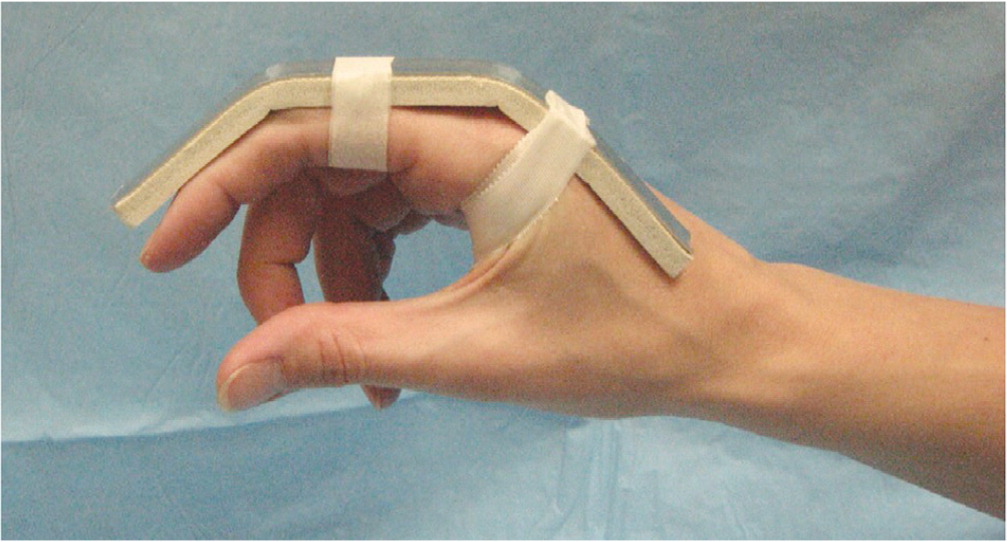
After successful reduction and radiographic confirmation, the PIP joint should be buddy taped to an adjacent finger. Dorsal dislocations should be treated using an extension-block splint, with the finger slightly flexed at 20 to 30 degrees for two to three weeks (Figure 717), then progressive flexion as tolerated. Protected early motion (within one week as allowed by pain and swelling) is encouraged after dorsal dislocations of the PIP joint.2
PIP JOINT: VOLAR
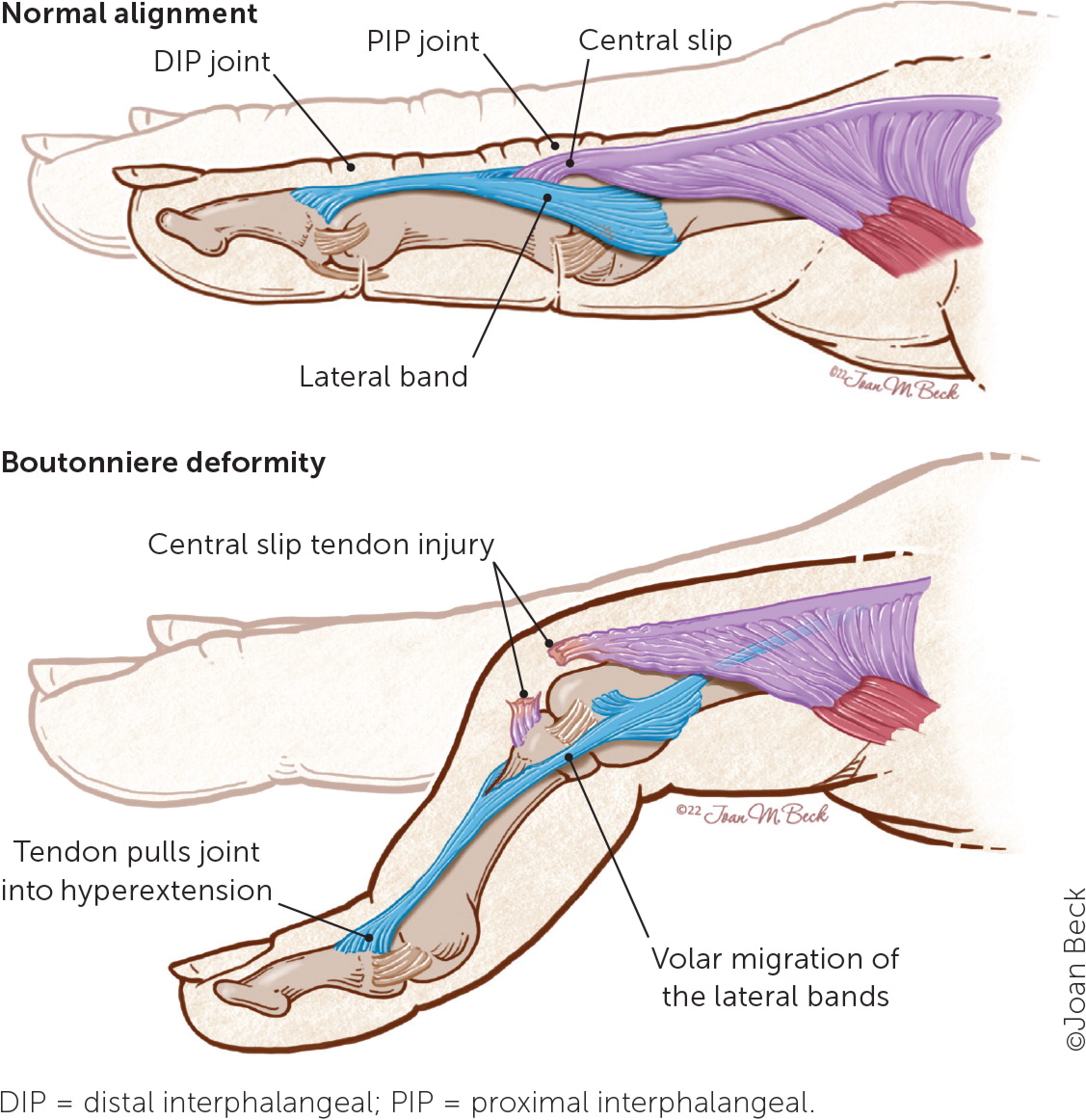
Volar dislocations are reduced in the same way as dorsal dislocations.20 Once reduction is performed, evaluation for a central slip disruption should be done by placing the PIP joint at 90 degrees on the edge of a table and asking the patient to extend the joint against resistance 21 (Figure 9). A positive result includes successful extension of the DIP joint but the inability to extend the PIP joint.

DIP JOINT
DIP joint dislocations are less common and are usually due to a crush injury in which an object (e.g., baseball) hits the finger, causing the DIP joint to hyperextend or hyperflex. Radiography is needed to determine whether a concomitant fracture is present.
Reduction of a dorsal DIP joint dislocation involves applying gentle traction, hyperextending the DIP joint, and then returning the joint to the correct anatomic position. If there is a wound (usually present over the volar surface), it is considered an open dislocation and should be treated surgically to avoid infection. Additional surgical indications include the inability to reduce the injury, prolonged dislocation, or persistent instability despite relocation.15
MCP JOINT
This section discusses MCP joint dislocations of the digits, excluding the thumb. MCP dislocations are usually due to a direct blow, causing hyperextension injury. The MCP joint can be dislocated in the dorsal (most common), volar, or lateral plane.2 Similar to the PIP joint, dorsal MCP joint dislocations can cause volar plate injuries. MCP joint dislocations are further divided into simple vs. complex dislocations, which can be determined using radiography.
Simple dislocations maintain some contact between the two articular surfaces of the MCP joint. However, complex dislocations show no continuity between the joint surfaces and can involve sesamoids or relocation of other soft tissues within the joint, making closed reduction difficult.
Simple dorsal dislocations are managed immediately with reduction and a dorsal extension-block splint set at 30 to 60 degrees of flexion for seven to 10 days, then transitioned to buddy taping and early range of motion.22 Patients with dorsal dislocations that cannot be easily reduced or have characteristics of a complex injury on plain radiography should be referred immediately to an orthopedic specialist. Volar dislocations of the MCP joint are rare and require referral to an orthopedic specialist.
Simple lateral dislocations can be managed with a dorsal extension-block splint set at 30 to 60 degrees of flexion for three weeks, followed by buddy taping for another two to three weeks. Lateral dislocations that occurred more than two weeks previously and involve greater than 20% of the joint surface or are displaced by greater than 2 mm warrant referral to an orthopedic specialist. Lateral dislocations may also result in injury to or instability of the radial collateral ligament because they usually tilt toward the ulna and should prompt surgical evaluation.
This article updates a previous article on this topic by Borchers and Best.19
Data Sources: A PubMed search was completed in Clinical Queries using the key terms finger, fracture, and dislocation. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Health-care Research and Quality evidence reports, Clinical Evidence, the Cochrane database, Essential Evidence Plus, the Institute for Clinical Systems Improvement, and DynaMed. Search dates: April 14, 2021, and March 8, 2022.
