
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2024;109(4):324-332
Related Letter to the Editor: Doxy PEP and Anal Cancer Screening for Men Who Have Sex With Men
Related Editorial: Implementing HIV PrEP in Routine Practice
Author disclosure: No relevant financial relationships.
Men who have sex with men (MSM) is an inclusive term used to refer to phenotypic males who have insertive or receptive sex (penile-anal or penile-oral) with other phenotypic males, including people who are transgender or have other gender identities. MSM may report their sexual orientation as homosexual, bisexual, heterosexual, or something else, but this stated sexual orientation may not align with their sexual attraction or behaviors. Several health conditions disproportionately affect MSM compared with age-matched heterosexual men, including HIV infection, anal cancer, syphilis, and depression. Clinicians should use culturally sensitive questions to obtain a comprehensive sexual history and assess sexual risk. MSM should receive regular screening for HIV, hepatitis B and C, gonorrhea, chlamydia, and syphilis. Vaccinations for hepatitis A and B and human papillomavirus should be offered. MSM may benefit from preexposure prophylaxis to prevent HIV infection, postexposure prophylaxis to reduce the risk of HIV transmission, and counseling on safer sexual practices. Screening for anal cancer associated with human papillomavirus may be performed by digital anal rectal examination, although the optimal screening strategy has yet to be determined. Clinicians should also consider more frequent screenings for mental health issues in the MSM population because the rates of depression, suicide, substance use, and other psychosocial issues are higher than those of the general population.
Men who have sex with men (MSM) is an inclusive term used to refer to phenotypic males who have insertive or receptive sex (penile-anal or penile-oral) with other phenotypic males, including people who are transgender or have other gender identities. MSM is a term more commonly used in research settings, and most patients will use different language to describe their sexual orientation and behaviors. MSM comprise an estimated 3.8% to 6.4% of the U.S. population; however, this is likely underreported.1 Patients may report their sexual orientation as homosexual, bisexual, heterosexual, or something else, but this stated sexual orientation may not align with their sexual attraction or behaviors.2
Sexually transmitted infections (STIs) that disproportionately affect MSM include HIV, anal cancer associated with human papillomavirus (HPV), and syphilis.3–5 MSM also experience disparities in terms of mental health and suicide risk,6 access to health care,7 and self-reported physical and mental health.8 This review aims to update the primary care physician with recommendations and guidelines relevant to the preventive care of MSM (Table 17,9–14).
| Term | Definition | Term | Definition |
|---|---|---|---|
| Sexuality Sexual identity Sexual orientation Bisexual Gay Heterosexual Pansexual | A person's sexual behavior, values, needs, preferences, and preferred modes of expression A person's action of claiming through recognition, acceptance, or self-labeling their sexual orientation as it relates to the self A person's self-identified sexual and romantic attractions; distinctly separate from a person's gender identity and expression Emotionally/sexually attracted to men and women Emotionally/sexually attracted to other men; it can also be a broader term for people attracted to people of the same sex or gender identity as themselves Emotionally/sexually attracted to someone of the opposite gender (e.g., a man attracted to a woman) Emotionally/sexually attracted to people of all gender identities, not necessarily related to a specific gender identity | Gender Cisgender Transgender Gender expression Gender identity Sexual minority Sexualized drug use Chemsex | Overall feelings and attitudes a society associates with a person's biological sex A person whose gender identity and gender expression are consistent with their sex assigned at birth A person whose gender identity or gender expression differs from their sex assigned at birth A person's appearance, behavior, or characteristics as defined in society as normative for masculine or feminine A person's basic sense of being a man, woman, or other gender A person whose emotional/sexual attraction, orientation, or characteristics differ from those of a heterosexual person The use of any illicit substance before or during sexual intercourse Use of specific illicit substances planned before or during sex to prolong, facilitate, sustain, or intensify the encounter; can involve more than two participants |
Communication
Discussing sexual orientation and gender identity with patients can improve the physician-patient relationship and lead to better care.11 Table 2 outlines supportive ways to inquire about sex partners and sexual orientation, practices, preferences, and risk.12,14,15 Materials and questionnaires that are sensitive to the needs of this population can be found on the Centers for Disease Control and Prevention (CDC) website15 and in the Joint Commission LGBT Field Guide.11
| Topic | Examples |
|---|---|
| Introduction of questions | “I ask questions about sexual history of all my patients at least once a year; are you ok if we begin?” “It is common for people to change their sexual behavior over time.” “This conversation may help guide recommendations to help you stay healthy, including the prevention of sexually transmitted infections.” |
| Sexual orientation | “What are the typical genders of your preferred sex partners?” “Who do you find yourself sexually attracted to?” |
| Sex partners | “Is your sex partner a long-term partner? Are you both monogamous?” “Do you know if your sex partners are having sex with other people?” |
| Sexual activity | “Have you been sexually active in the past year?” “How many different sex partners have you had in the past 2 months? The past 12 months?” |
| Sexual risk | “Have you ever had a sexually transmitted infection like HIV, gonorrhea, syphilis, herpes, or chlamydia? If so, did you receive treatment?” “Have you ever been exposed to any of those diseases that you knew about?” “Do you use condoms when you have sex? How often?” “Do you use alcohol or drugs when you have sex? How often?” “Do you have any concerns about staying safe sexually?” |
| Counseling | “Are you interested in discussing strategies to reduce your risk of sexually transmitted infections?” “Would you like more education about sexually transmitted infections and how to prevent them?” |
Obtaining a comprehensive sexual history is critical to providing optimal care. This history can be obtained through direct questioning from the physician or other health care professionals. It can also be obtained from standard intake forms in the electronic health record or via printouts provided to the patient.12 Consider regular assessments of clinic signage, patient questionnaire wording, and staff training that could contribute to a negative experience for MSM.7 The Joint Commission provides guidance to establish a safe and welcoming environment for sexual and gender minority patients.11
General Health Care
Standard preventive care recommendations include routine laboratory work, immunizations, and screenings for cancer, depression, hypertension, tobacco use, and unhealthy alcohol use.16 Additional care for MSM may include offering supplementary immunizations and STI screening, updating sexual history and risk profile, offering preexposure prophylaxis (PrEP) and counseling on postexposure prophylaxis options for HIV prevention, identifying candidates for anal cancer screening, updating mental health screenings, and reviewing the patient's social determinants of health.
IMMUNIZATIONS
| Immunization | Recommended age | Recommended dosing* |
|---|---|---|
| Hepatitis A | All individuals 18 years and younger All MSM 19 years and older if not previously vaccinated |
Two-dose series at least 6 months apart |
| Hepatitis B | All individuals 18 to 59 years of age All MSM 60 years and older if not previously vaccinated |
Two- or three-dose series depending on formulation available† |
| Human papillomavirus | All individuals 26 years and younger For MSM 27 to 45 years of age, clinicians should use shared clinical decision-making |
Complete two- or three-dose series depending on age and HIV status: 15 years or older at initial vaccination: three doses, the second being 1 to 2 months later, and the third being 6 months later 9 to 14 years of age at initial vaccination and received one dose at least 5 months before: one additional dose 9 to 14 years of age at initial vaccination and received two doses at least 5 months apart: series complete; no additional dose needed regardless of age |
| Meningococcal serotypes A, C, W, Y | MSM when it has been more than 5 years since completion of primary series [corrected] | One booster dose† |
| Meningococcal serotype B | MSM when it has been more than 1 year since completion of primary series | One booster dose† |
ACIP recommends the hepatitis A vaccine series for all MSM older than 19 years who have not previously received it.19 For MSM older than 60 years, the hepatitis B vaccine should be offered as a two- or three-dose series.20 ACIP recommends the HPV vaccine for all patients through age 26 years, with an emphasis on immunization before the patient's first sexual activity. HPV can cause anal, oropharyngeal, and penile cancer, which can be prevented by vaccination.21 Due to the reduced effectiveness in older patients (due to prior exposure to the HPV strains in the vaccine), the ACIP recommends shared clinical decision-making regarding HPV vaccination for MSM between 27 and 45 years of age.22
STI Prevention
Strategies to help MSM reduce the risk of STIs include discussion about PrEP, education about condom use and the risk associated with douching before receptive anal sex, and frequent testing for STIs (Table 47,14,23–30). Rates of consistent condom use, defined as proper use at every sexual encounter, are relatively low in the United States; a recent review of data collected by the CDC found that only 28% of MSM with HIV infection, and 29% of MSM without HIV infection, reported consistent condom use from 2012 through 2017.31 Obstacles to consistent condom use include physical discomfort, lack of knowledge about HIV and other STIs, substance misuse, psychological factors, and environmental factors (availability and affordability of condoms).32 Approximately 29% to 52% of MSM practice douching in preparation for receptive anal sex, which may increase the risk of STIs by injuring the rectal mucosa.33
| Screening topic | Centers for Disease Control and Prevention recommendation | U.S. Preventive Services Task Force recommendation* |
|---|---|---|
| Behavioral counseling for risk reduction | No recommendation | Recommended for all sexually active adolescents and for adults who are at increased risk for sexually transmitted infections (grade B) |
| Genital herpes | Type-specific serologic tests can be considered if infection status is unknown for MSM with previously undiagnosed genital tract infection | Routine serologic screening for genital herpes simplex virus infection in asymptomatic adolescents and adults is not recommended (grade D) |
| Gonorrhea and chlamydia | Screen sexually active MSM at least annually at sites of contact (urethra, rectum, oropharynx [gonorrhea only]) regardless of condom use; screen every 3 to 6 months if at increased risk | Current evidence is insufficient to assess the balance of benefits and harms of screening for chlamydia and gonorrhea in men (grade I) |
| Hepatitis B | Screen those with behavioral exposures to hepatitis B; test for surface antigen, core antibody, and surface antibody | Screen adolescents and adults at increased risk for infection (grade B) |
| Hepatitis C | Screen all adults 18 years and older at least once | Screen adults 18 to 79 years of age (grade B) |
| HIV | Screen sexually active MSM at least annually if HIV status is unknown or negative and the patient or their sex partner(s) have had more than one sex partner since most recent HIV test | Screen adolescents and adults 15 to 65 years of age; younger adolescents and older adults who are at increased risk of infection should also be screened (grade A) |
| Human papillomavirus | Screen with a digital anal rectal examination; data are insufficient to recommend for or against routine anal cancer screening with anal cytology | Recommendation in progress; draft research plan published December 2022 |
| Syphilis | Screen sexually active MSM at least annually | Screen asymptomatic, nonpregnant adolescents and adults who are at increased risk (grade A) |
HIV
According to the CDC, MSM accounted for 68% of new HIV cases in the United States in 2020.3 Although there was a 17% reduction in total new cases in 2020 during the COVID-19 pandemic, this decrease in identified cases was likely due to decreased access to clinical care and shortages of HIV testing supplies.3 Multiple organizations, including the World Health Organization, CDC, and U.S. Preventive Services Task Force, recommend screening MSM for HIV at regular intervals with a fourth-generation immunoassay (enzyme-linked immunosorbent assay with p24 antigen and HIV antibodies).3,7,29
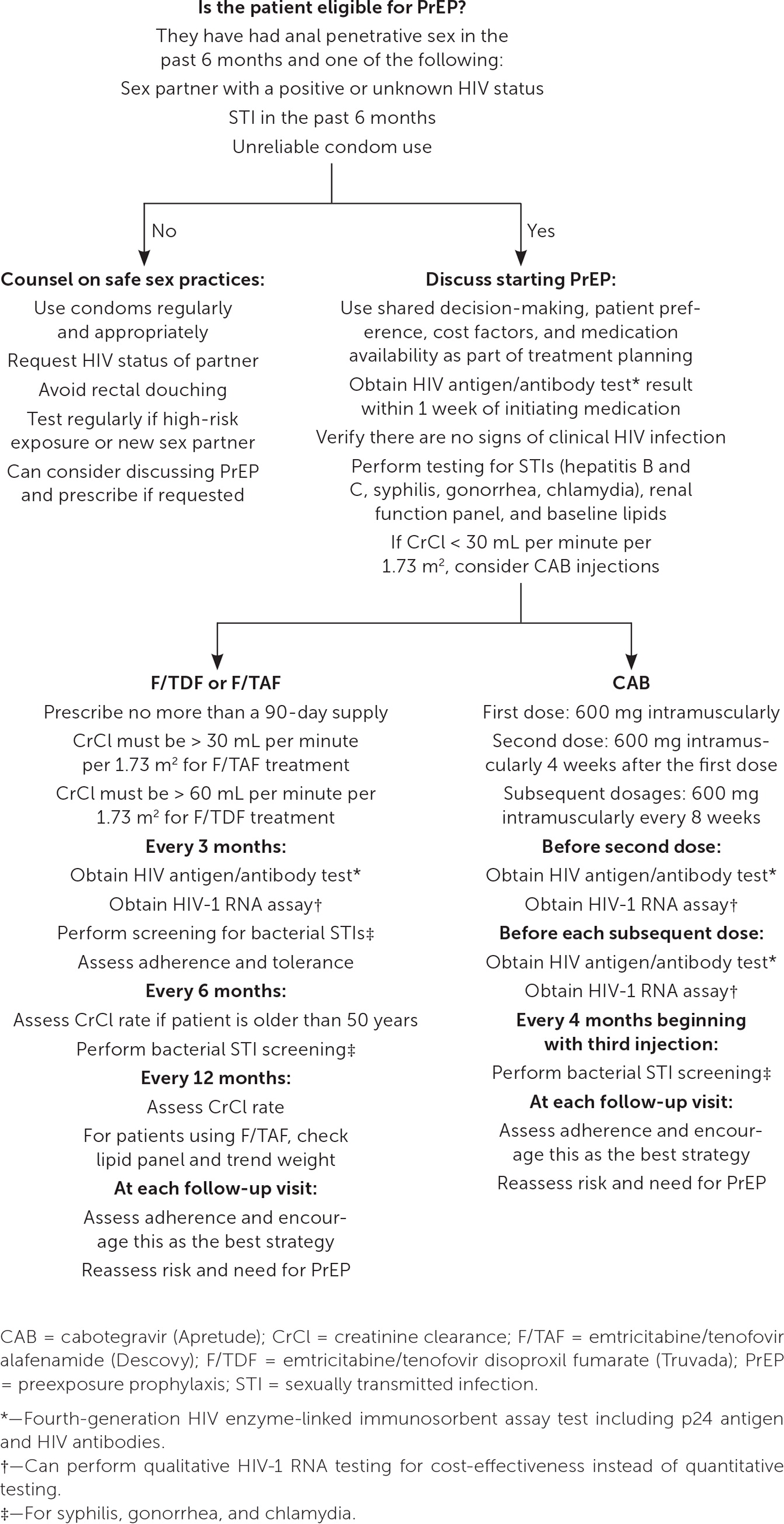
PrEP is recommended for MSM at increased risk of HIV infection34 (Figure 134–36). Approximately 34% of sexually active MSM in the United States are eligible for PrEP; however, only 25% of those eligible have been prescribed medication.37 Oral emtricitabine/tenofovir disoproxil fumarate (Truvada), emtricitabine/tenofovir alafenamide (Descovy), and injectable cabotegravir (Apretude) are acceptable for PrEP.35,38 PrEP should be offered to MSM who have high-risk sexual exposure, defined as sex within the past 6 months with a partner who has HIV infection with an unknown or detectable viral load, a personal history of bacterial STI in the past 6 months, or a history of inconsistent condom use with a partner whose HIV status is unknown.34,36 On-demand dosing, commonly prescribed as the “2-1-1” method (two pills 2 to 24 hours before intercourse, one pill 24 hours after the initial dose, and one pill 48 hours after the initial dose), can be offered; however, this dosing method is neither approved by the U.S. Food and Drug Administration nor endorsed by the CDC.34
Postexposure prophylaxis can be offered after a sexual encounter with a partner whose HIV status is positive or unknown. It should be initiated within 72 hours. Oral emtricitabine/tenofovir disoproxil fumarate taken once daily with raltegravir (Isentress) or dolutegravir (Tivicay) for 28 days is the recommended treatment course.39 The National Clinician Consultation Center provides physicians with direct access to infectious disease specialists and resources for patients who may not be able to afford these medications.39
OTHER SEXUALLY TRANSMITTED INFECTIONS
MSM are currently the group at highest risk for syphilis in the United States, and the estimated prevalence of the infection in this group is 5% to 10%.5,40 One-third of MSM with syphilis have no symptoms. Syphilis infection in MSM is associated with coinfection with HIV (likely due to higher-risk sexual behaviors).5 Reported barriers to syphilis testing include sociodemographic factors, depression, unwillingness to disclose sexual behavior, and health insurance status.5
The CDC recommends that MSM be tested for urethral and rectal infections of chlamydia and gonorrhea each year if there is exposure at these sites. Annual testing should also include the oropharynx for gonorrhea but not for chlamydia, because the number of such infections at this site is low.30 If a patient is on PrEP and considered high risk, the testing interval should increase to every 3 to 6 months.30
Mpox has been more prevalent in the gay and bisexual population, with total U.S. estimates of more than 30,000 cases since its resurgence in 2022.45 The peak incidence was in August 2022 and has since remained low.45 Two vaccines are available on a limited basis for patients with high-risk exposure.45,46
Anal Cancer Screening
Anal cancer incidence has been increasing since 1970 and is estimated to be 1.9 new cases per 100,000 people per year.47 MSM (particularly those who participate in anal receptive sex) are at increased risk, and MSM with HIV infection have the highest risk.48 HPV infection is the most common cause of anal cancer as well as its precursor, high-grade squamous intraepithelial lesions (HSIL), also known as anal intraepithelial neoplasia.49
The Anal Cancer HSIL Outcomes Research (ANCHOR) study evaluated the effectiveness and safety of treating HSIL vs. active monitoring without treatment in preventing the progression to anal cancer in people with HIV; it found that treatment of HSIL reduced the rate of progression by 57%.50 This study may impact future screening and treatment recommendations.
Screening guidelines for MSM differ based on HIV status. Several organizations have screening recommendations for people with HIV who are MSM (Table 551–54), although most are based on expert opinion or low-quality data. Based on expert opinion with limited data, the International Anal Neoplasia Society additionally recommends that MSM who test negative for HIV have a digital anal rectal examination every 2 to 5 years starting at 50 years of age.55 Abnormal findings on examination include hard, irregular lumps or ulcerations; small granular changes causing localized thickening of tissue; and any palpable areas that are not reducible. Such findings should prompt a high-resolution anoscopy performed by an experienced physician or a colorectal surgery referral.55
| Organization | Current recommendation |
|---|---|
| American Society of Colon and Rectal Surgeons | Anal cytology may be considered in high-risk populations, including MSM and patients with HIV infection High-resolution anoscopy can be used for screening in high-risk populations if performed by clinicians with appropriate training* |
| Infectious Diseases Society of America and HIV Medicine Association | Annual digital anal rectal examination Anal Pap test for patients with HIV who have a history of receptive anal intercourse and anyone with genital warts (if access to appropriate referral for follow-up, including high-resolution anoscopy, is available) |
| New York State Department of Health AIDS Institute | Baseline and yearly inquiries about anal symptoms, visual inspection of perianal region, digital anal rectal examination, and annual Pap test for all HIV-positive MSM 35 years and older |
| U.S. Department of Health and Human Services Office of Infectious Disease and HIV/AIDS Policy | No national recommendations for standardized anal cancer screening Annual digital anal rectal examination |
Other screening modalities include anal Papanicolaou test with cytologic testing and high-resolution anoscopy, but both methods rely on clinician experience.56
Mental Health and Psychosocial Issues
MSM are more likely to experience victimization, threats of violence, social isolation, intimate partner violence, homelessness, poverty, and increased perceived stressors compared with age-matched heterosexual men. According to recent global meta-analyses, the pooled prevalence of depression in MSM with HIV infection was 43% to 47% and was significantly higher than that of MSM without HIV (odds ratio = 1.46).57,58 One study concluded that in the United States, the prevalence of depression among MSM varied from 17.2% to 33%.6,57 A younger age at first sexual encounter, homelessness, and substance misuse are associated with the highest rates of suicide attempts in the MSM population.59 Other factors associated with an increased risk of suicidality include bullying, parental abuse, and victimization.59 More frequent screening for depression in MSM is reasonable.57–59
A minority of MSM use illicit substances to enhance their sexual experience; this practice is known as chemsex. Physicians should periodically screen MSM for chemsex participation and offer risk reduction counseling.13 Chemsex has been associated with increased rates of depression, anxiety, and other substance use in the MSM population.60 Motivational interviewing and cognitive behavior therapy techniques may reduce high-risk alcohol use among MSM.61
This article updates previous articles on this topic by Knight and Jarrett14 and Knight.62
Data Sources: A PubMed search was completed in Clinical Queries using the key terms men who have sex with men, men having sex with men, preventive care, and primary care. The search included meta-analyses, randomized controlled trials, large clinical trials, and systematic reviews. The Agency for Healthcare Research and Quality Effective Healthcare Reports, the Cochrane database, DynaMed, and Essential Evidence Plus were also searched. Whenever possible, if studies used race and/or gender and/or sexual orientation as patient categories, but did not define how these categories were assigned, they were not included in our final review. If studies that used these categories were determined to be essential and therefore included, limitations were explicitly stated in the manuscript. Search dates: February 2 to 6, 2023, and February 14, 2024.
