
Am Fam Physician. 2024;110(3):228-229
Author disclosure: No relevant financial relationships.
Rates of hepatitis C virus (HCV) infection have increased steadily in the United States since 2010 and are highest among people 20 to 39 years of age. As a result, rates of HCV infection during pregnancy increased by approximately 10-fold from 2000 to 2019 and by 20% from 2016 to 2020.1 The Centers for Disease Control and Prevention recommendations for testing infants perinatally exposed to HCV are designed to identify and manage cases early, prevent progression of the disease and future liver complications, and reduce the risk of further transmission. Universal testing for HCV infection is recommended for all pregnant people during each pregnancy, preferably early in the prenatal period. Antenatal counseling should emphasize the importance of follow-up testing for infants and ensure appropriate care if infection is confirmed.1
Professional societies recommend testing perinatally exposed infants at or after 18 months of age with an HCV antibody test, followed by a nucleic acid test (NAT) for HCV RNA when the antibody test is reactive. Persistence of passively transferred maternal antibody from the infected birthing parent to the infant prevents the use of an antibody test before 18 months of age.1 However, approximately 70% of children exposed perinatally are not tested using the strategy of HCV antibody testing at or after 18 months of age, resulting in loss to follow-up.2–4 This could be due to lack of awareness of perinatal exposure, prolonged time before HCV testing, lack of regular well-child care, and changes in primary care physicians before 18 months of age.
The Centers for Disease Control and Prevention now recommends that all infants and children born to people with HCV infection be tested with a NAT for HCV RNA at 2 to 6 months of age.1 Highly sensitive and specific NATs for HCV RNA detection are available starting at 2 months of age, and more children attend well-child visits at 2 to 6 months of age than at 18 months or older. Therefore, NATs for HCV RNA at 2 to 6 months of age will identify more children with perinatal HCV transmission who are eligible for curative treatment beginning at 3 years of age.1
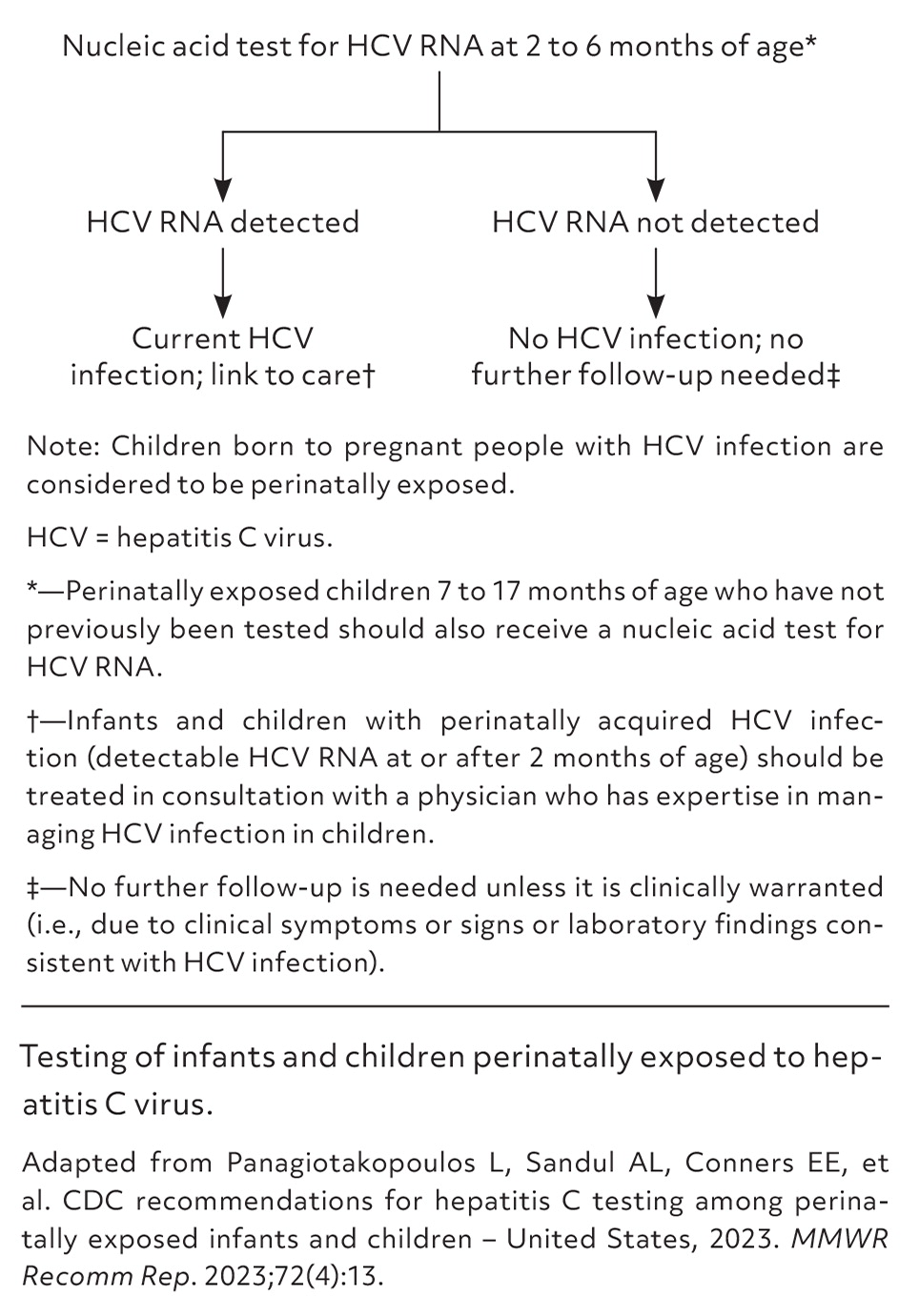
Standard clinical practice of testing with a NAT for HCV RNA should be performed at or after 2 months of age (Table 1).1 Because current NAT tests are highly sensitive, testing for HCV RNA at 2 to 6 months of age is sufficient; detectable HCV RNA confirms perinatal HCV transmission, and undetectable HCV RNA rules out transmission.1 When HCV RNA is not detected, no further follow-up is required (Figure 1).1
| All infants and children born to pregnant people with current or probable HCV infection should be tested for infection. |
| A pregnant person is considered to have current HCV infection when HCV RNA is detected at any time during pregnancy. If HCV RNA test results are not available, a pregnant person is considered to have probable HCV infection during pregnancy when HCV antibody test results are reactive.* |
| Perinatally exposed infants should receive a NAT for HCV RNA at 2 to 6 months of age to identify those who might develop chronic HCV infection. |
| Infants with detectable HCV RNA should be treated in consultation with a physician who has expertise in managing HCV infection in children. |
| Infants with undetectable HCV RNA do not require further follow-up unless it is clinically warranted (i.e., due to clinical symptoms or signs or laboratory findings consistent with HCV infection). |
| Infants and children 7 to 17 months of age who have not previously been tested should receive a NAT for HCV RNA. |
| Children 18 months of age and older who have not previously been tested should receive an HCV antibody test with reflex to HCV RNA.† |
Perinatal HCV testing identifies children who are at risk of developing complications from chronic HCV infection, including elevated alanine transaminase levels and slowly progressive hepatic fibrosis indicating histologic injury. Although development of advanced liver disease is uncommon until much later in life among perinatally infected children, progression to advanced fibrosis and cirrhosis during adolescence can occur.5,6 Spontaneous clearance (i.e., resolution of the infection without treatment) occurs in at least 20% to 40%, and as much as two-thirds, of children with perinatally acquired HCV infection by 5 years of age; however, many children will remain infected and benefit from treatment.1,7,8
Approximately 6% to 7% of perinatally exposed children acquire perinatal HCV infection.1 Although curative direct-acting antiviral therapy is approved by the U.S. Food and Drug Administration for children at 3 years of age and older, more than one-half of perinatally infected children are not tested or linked to care.2–4 It is critical for physicians to follow guidelines for timely detection and appropriate management of HCV infection among perinatally exposed infants. Early identification and intervention can significantly improve outcomes.
Infants and children with perinatally acquired HCV infection should be managed in consultation with a physician who has expertise in managing HCV infection in children to provide appropriate screenings, preventive services, interventions, and regular follow-up. To confirm chronic HCV infection, children with positive test results at 2 to 6 months of age should be retested with a NAT for HCV RNA before initiation of direct-acting antiviral therapy, which can be started as early as 3 years of age.
Centers for Disease Control and Prevention testing recommendations focus on an earlier infant age range (2 to 6 months) due to increasing rates of childhood HCV infection, high rates of loss to follow-up among perinatally exposed infants and children, and the increased effectiveness of NATs for HCV RNA detection in young infants.1 Testing beginning at 2 months of age allows for earlier linkage to care, appropriate evaluation, and the opportunity to provide life-saving treatment. Family physicians are uniquely positioned to provide continuity of care and ensure curative treatment with direct-acting antiviral drugs for infants, children, and birth parents with HCV infection.
