
Medicare's physician payment rate is again slated to drop absent congressional action. But primary care physicians may find financial relief in other policies.
Fam Pract Manag. 2025;32(1):28-34
Author disclosures: no relevant financial relationships.

The new year brings many predictable annual traditions, such as the ball dropping in Times Square and your gym suddenly being overcrowded the first few weeks of January. It also brings new coding and payment changes from Medicare and CPT. While there are positive aspects for primary care, this year's news is much like last year's1 — complicated and part of a much larger story. The 2025 Medicare Physician Fee Schedule (MPFS) again includes a cut to physician payment that is mandated by budget neutrality requirements. At press time, Congress is yet again discussing ways to stave off the cut. This seemingly annual two-step is part of the broader tension between what the Centers for Medicare & Medicaid Services (CMS) would like to accomplish — including strengthening primary care — and the statutory and budgetary limits on its abilities to pursue those priorities.
In its public comments on the 2025 MPFS proposed rule,2 the AAFP explicitly noted its “concerns for the long-term sustainability of Medicare and the physicians who make the program possible,” and reiterated those concerns3 when the final rule was released. The AAFP also joined other physician organizations4 to encourage congressional leaders to fix Medicare physician payment in a more lasting way.
Specific concerns that are beyond the authority of CMS to address in the MPFS rule include the following:
The outdated budget neutrality requirement that applies exclusively to the MPFS, which causes physician payment to lag behind other Medicare spending,
Lack of an inflationary update to account for the increased expense of running a practice, which results in an ongoing loss of independent physician practices,
Beneficiary cost-sharing requirements that hinder patients' ability to consistently engage with their primary care physician,
Inadequate data and information flow that continues to hamper family physicians' ability to deliver high-quality, comprehensive, and coordinated care to patients.
Addressing these foundational Medicare physician payment and communication issues will require congressional action. However, there are still glimmers of hope in the 2025 MPFS final rule, including expanded use of code G2211 and a new set of advanced primary care management codes that build on lessons learned in the Center for Medicare and Medication Innovation (CMMI) primary care models.
KEY POINTS
As Congress discusses whether to temporarily stave off yet another mandated cut in Medicare physician pay rates, the AAFP and other organizations continue to advocate for a more lasting solution.
Medicare is providing some boosts for primary care, including expanded use of visit complexity code G2211 and a new set of codes for advanced primary care management.
New telemedicine codes, as well as new codes for vaccines and monoclonal antibodies, are among the CPT updates relevant to family physicians.
MEDICARE PAYMENT POLICY CHANGES
We start our updates with the 2025 Medicare conversion factor, perhaps best described using the famous words of Yogi Berra: “It's like déjà vu all over again.” As noted earlier, the conversion factor, the amount Medicare pays per relative value unit (RVU), is scheduled for a cut and the bill Congress passed last year to stave off that cut is set to expire. The good news is, at press time, there are bills in the U.S. House of Representatives that would alleviate the impact of the decrease. But no one knows if or when Congress will act on them. For now, expect to see a 2025 conversion factor of $32.35, a decrease of $0.94 (or just under 3%) from the 2024 conversion factor. This article will be updated if that changes.
Now on to some other Medicare items of note, including those glimmers of hope.
Expansion of HCPCS code G2211. CMS previously prohibited clinicians from reporting visit complexity add-on code G2211 when they reported the base office/outpatient evaluation and management (E/M) code with modifier 25 for any reason. Following AAFP advocacy, the agency will now allow G2211 when clinicians report the E/M code with modifier 25 on the same day as an annual wellness visit, vaccine administration, or any Medicare Part B preventive service, including the Initial Preventive Physical Examination.
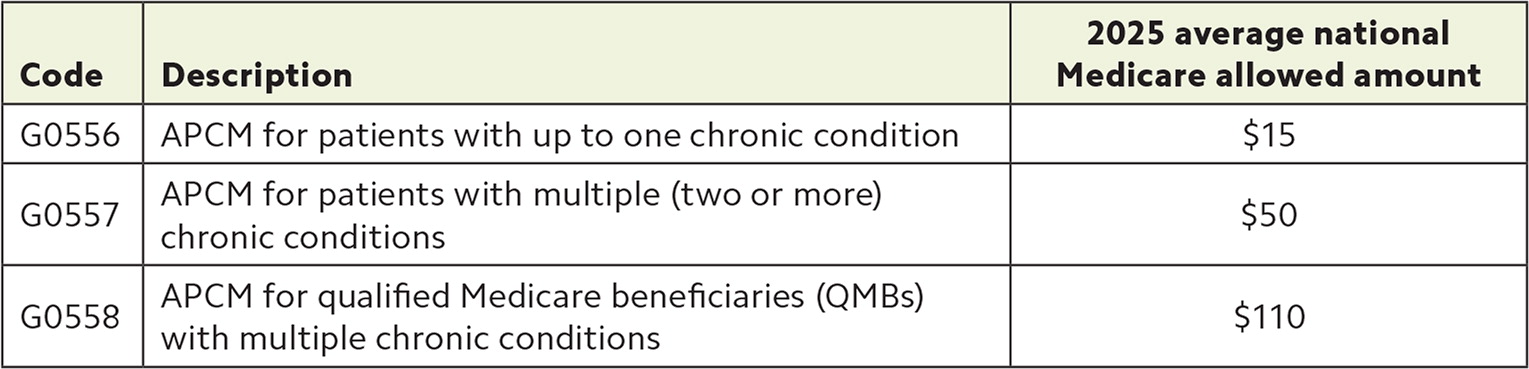
Advanced primary care management. CMS finalized three new codes that correspond to three levels of advanced primary care management (APCM) services. These are monthly codes intended to recognize the resources associated with providing advanced primary care to Medicare beneficiaries. CMS expects APCM to be provided by clinicians who are or will be responsible for the patient's primary care and serve as the focal point for all the patient's health care services. While APCM codes are not explicitly restricted to any specialty, CMS believes the codes will be primarily used by primary care specialties.
APCM codes incorporate elements of several existing care management codes (including chronic, principal, and transitional care management) into a bundle of services. But the APCM codes are applicable to a broader patient population and do not have many of the other codes' burdensome documentation requirements, such as time-based thresholds.
Practices have some flexibility in how they satisfy most APCM service elements (see below), but the “performance measurement” element requires either participation in one of these Medicare payment programs — Primary Care First, Making Care Primary, Medicare Shared Savings Program (MSSP), or Realizing Equity, Access, and Community Health — or use of the Value in Primary Care MIPS Value Pathways (MVP) reporting option.
Physicians should note a few other things about APCM services:
They are designated as “care management” services, and auxiliary staff can provide them under the general supervision of the billing clinician.
They are subject to beneficiary cost-sharing, with some exceptions. Qualified Medicare beneficiaries are not subject to cost-sharing for any covered Part A or B services, including APCM.5
Patients do not need to receive all service elements each month. However, practices must maintain the ability to provide all services to each beneficiary every month.
Only one clinician may report APCM services for a Medicare beneficiary in a given month. The clinician reporting the APCM services may not separately report individual services included in the APCM bundle for that patient that month.
ADVANCED PRIMARY CARE MANAGEMENT CODES AND SERVICES
Medicare will start paying for advanced primary care management (APCM) in 2025 when clinicians report the following codes for providing the following services.
APCM codes
The new codes account for three levels of APCM.
APCM service elements
For details on each of the following requirements, see the CMS website.
- Patient consent (they may be subject to cost-sharing) (Editor's note: for a consent form template, see this FPM Quick Tips blog post.)
- Initiating visit for new patients
- 24/7 access to a member of the care team and continuity of care
- Comprehensive care management
- Patient-centered comprehensive care plan
- Management and coordination of care transitions
- Care coordination (practitioner, home, and community-based care)
- Enhanced communication (e.g., portal messaging, interprofessional referrals)
- Population-level management (identify care gaps and risk-stratify practice panel)
- Performance measurement
Services included in APCM
Clinicians cannot bill separately for the following services if they are already billing for APCM for that patient.
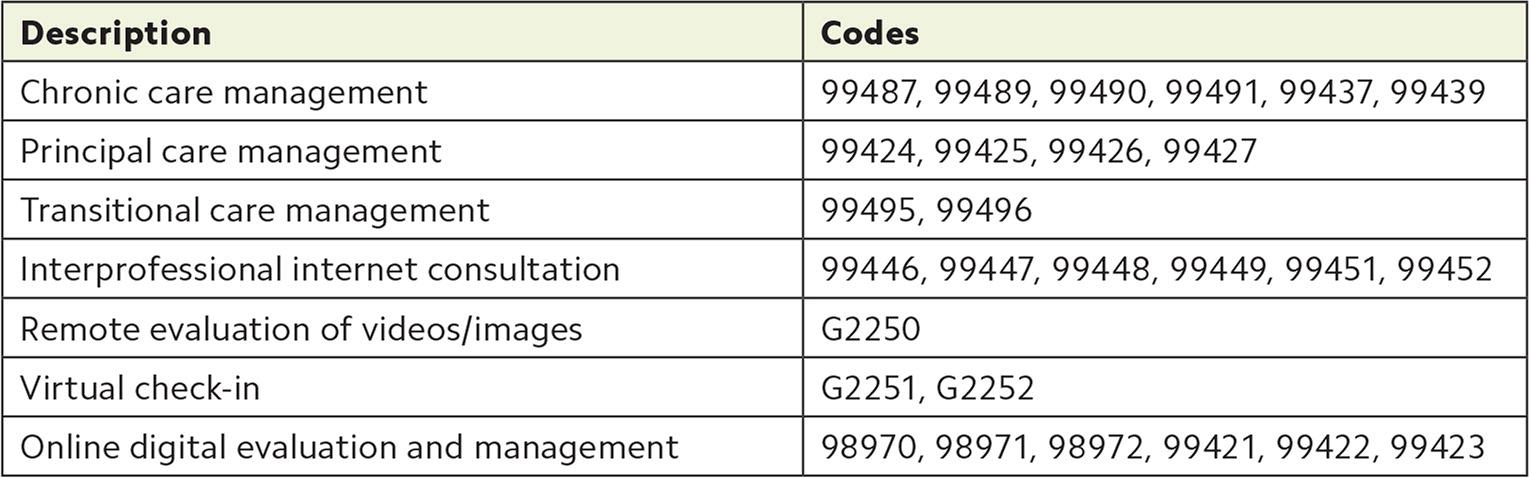
Telehealth. Absent congressional action, Medicare telehealth limitations in place prior to the COVID-19 public health emergency go back into effect for most services performed on or after Jan. 1, 2025 (update: a spending bill passed at the end of December extended the telehealth flexibilites until March 31, 2025). These include geographic and originating site restrictions (i.e., telehealth will once again be limited to patients in rural areas, and patients will not be able to receive telehealth services from their homes). Telehealth provided to diagnose and treat mental health and substance use disorders are not subject to these restrictions.
The American Medical Association's CPT Editorial Panel has adopted a new telemedicine code set but Medicare is only adopting one of the new codes, 98016, to replace the virtual check-in code G2012. Otherwise, review the Medicare Covered Telehealth Services List to see which HCPCS codes to use.6
Medicare preventive services. Medicare is expanding coverage of hepatitis B vaccines. Patients who have not previously completed the hepatitis B vaccination series or whose vaccination history is unknown will be eligible for hepatitis B shots without cost-sharing.
Medicare is also changing coverage of colorectal cancer (CRC) screenings to reflect updated clinical guidelines by removing coverage of the barium enema, adding coverage of computed tomography colonography, and adding Medicare-covered blood-based biomarking CRC screening tests to the definition of “complete CRC screening.”
CPT CODING UPDATES
There are 420 new CPT codes, deletions, and revisions in the 2025 code set. The largest proportion of new codes (37%) are in the Proprietary Laboratory Analyses section, mostly for novel genetic testing. Emerging medical services account for about 30% of new codes. A smaller number of changes will impact family physicians.
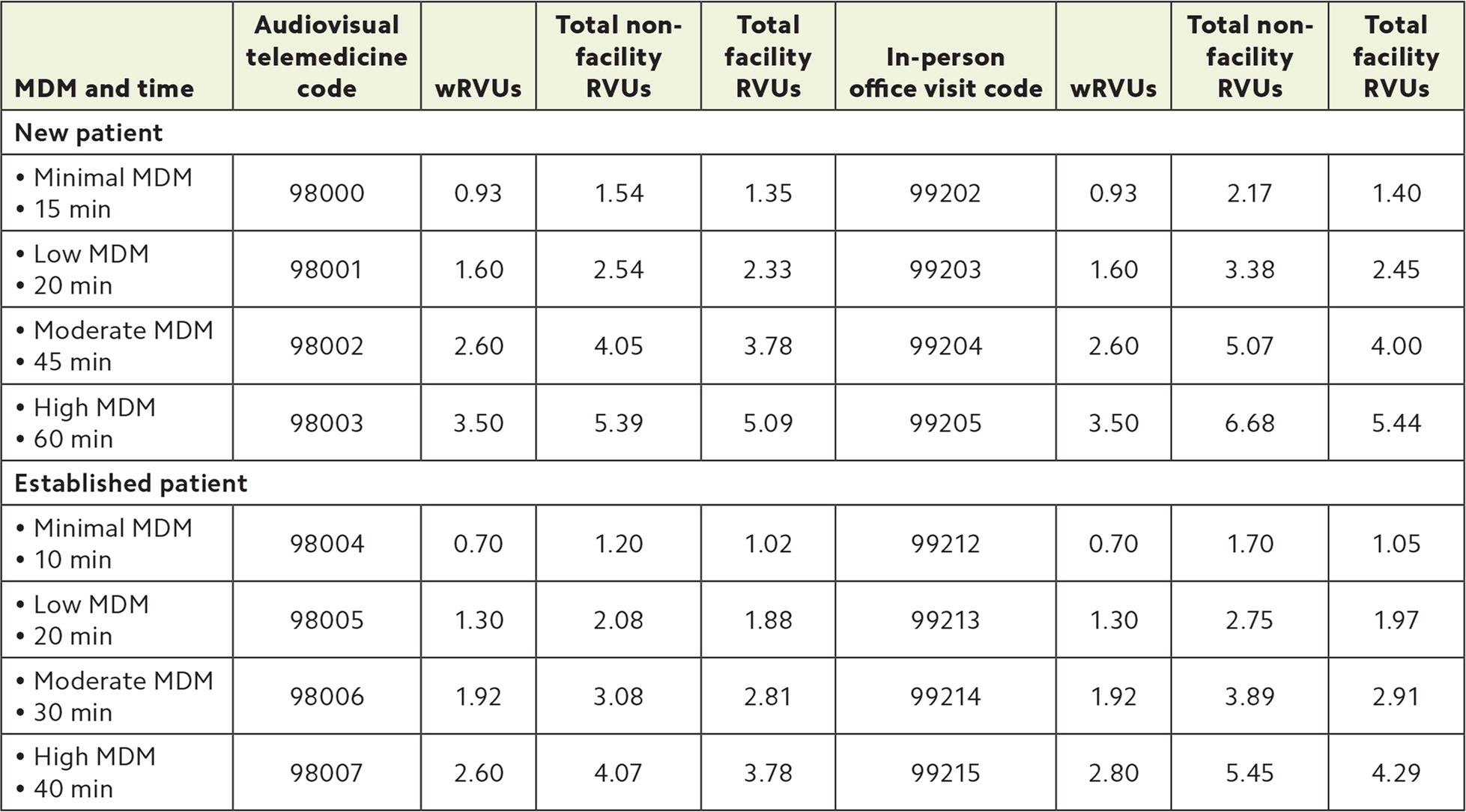
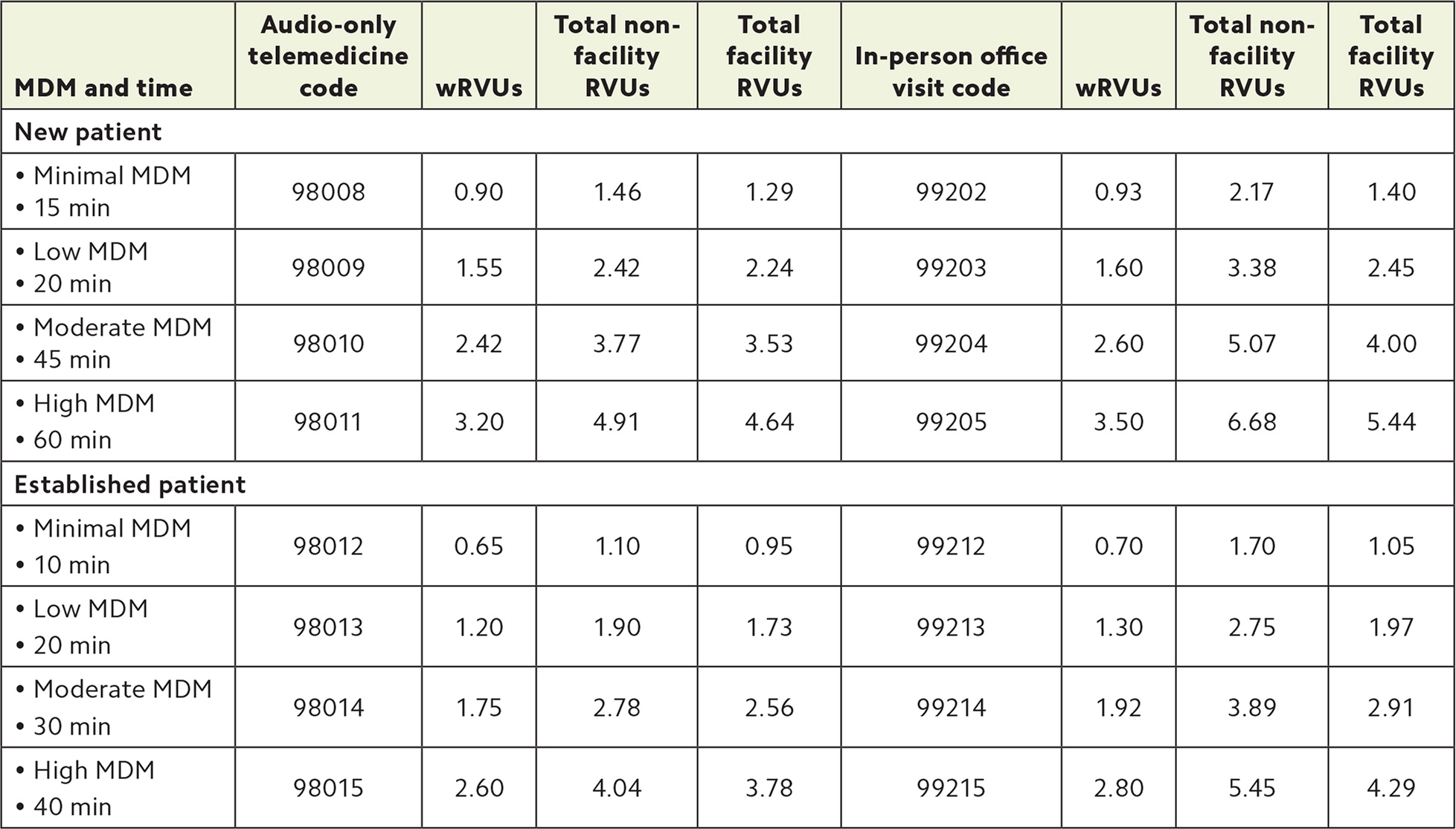
Telemedicine E/M services. CPT is adding a new set of 17 codes to report audiovisual and audio-only telemedicine E/M (see “New CPT telemedicine E/M codes”). The new audio-only codes replace telephone E/M codes 99441-99443, which CPT has deleted. CPT defines telemedicine services as synchronous, real-time interactive encounters between a physician or other qualified health care professional (QHP) and a patient using audio-only or audiovisual communication. (Asynchronous services, such as portal messaging, should still be reported with online digital E/M codes 99421-99423.) As mentioned, Medicare is only adopting one of these codes thus far, and private payers will likely vary in their use, so check with them individually.
The new telemedicine codes are used in lieu of an in-person service, when medically appropriate, and they mirror existing office/outpatient E/M codes for new and established patients in that you select the code level based on either medical decision making (MDM) or total time on the day of the encounter. All require at least 10 minutes of medical discussion for time-based billing.
For telemedicine services that involve only 5–10 minutes of medical discussion, CPT established a new “virtual check-in” code, 98016. Virtual check-ins can be audiovisual or audio-only, but are limited to established patients and intended to evaluate whether the patient needs a more extensive visit. The patient must initiate the service, and it cannot be related to a visit within the previous seven days nor lead to an E/M service in the next 24 hours or soonest available appointment.
Telemedicine services that must be provided via audiovisual technology are listed with the five-pointed star symbol in CPT 2025, while those that may be provided via audio-only are listed with the speaker symbol. They can also be found in Appendix P and Appendix T, respectively. CPT instructs clinicians to append modifiers 95 (audiovisual) or 93 (audio-only) for telehealth, but payers vary on their use of these modifiers.
NEW CPT TELEMEDICINE E/M CODES
Audiovisual telemedicine vs. in-person equivalent
Requirements for medical decision making (MDM) and total time are the same. Work relative value units (wRVUs) are the same except for high-level MDM for established patients.
Audio-only telemedicine vs. in-person equivalent
Unlike most audiovisual telemedicine codes, audio-only telemedicine codes carry fewer wRVUs than their corresponding in-person office visit codes.
Vaccines/toxoids. Updates CPT made in late 2023 for COVID-19 vaccines are appearing for the first time in the CPT code set in 2025 due to publication timing. Report COVID-19 vaccine administration using code 90480. This code is used for all ages and includes both the administration and counseling. For the other vaccine administration codes (90460, 90461, and 90471-90474), CPT instructs clinicians not to report them with COVID-19 vaccine product codes unless they give both a COVID-19 vaccine product and at least one other vaccine/toxoid product on the same day.
There are only six product codes for COVID-19 vaccines (91304, 91318, 91319, 91320, 91321, and 91322). These codes describe the product only and are reported in conjunction with administration code 90480. Other vaccine code changes include three new influenza vaccine codes (90695, 90637, and 90638) that differ based on type and dosage, a new 21-valent pneumococcal conjugate vaccine code (90684), and a new pentavalent meningococcal vaccine code (90624).
Immune globulins and monoclonal antibodies immunizations. Also appearing for the first time in CPT are administration codes approved to accompany product codes for seasonal respiratory syncytial virus (RSV) prevention with monoclonal antibodies. CPT 96380 is for administration with counseling, and 96381 is for administration without counseling (the product codes are 90380 for 0.5 mL dose and 90381 for 1 mL). Antibody treatments are not technically vaccines, and the product and administration codes are different than those used to report RSV vaccines for patients 60 and older or pregnant.7
CPT releases new vaccine/toxoid/immunoglobulin product codes April 1, July 1, and Oct. 1 of each year with corresponding effective dates of July 1, Oct. 1, and Jan. 1. Practice staff should set reminders to review the AMA website for the latest updates.
Remote therapeutic monitoring and AI-augmented analysis. CPT made editorial revisions for remote therapeutic monitoring (RTM), updating code 98975 to include digital therapeutic intervention, while revising codes 98976-98978 to include device supply for data access or data transmissions to support RTM of patients.
CPT established seven new codes for services driven by augmented/artificial intelligence (AI). The codes are for AI-augmented data analysis in electrocardiogram measurements (0902T and 0932T), medical chest imagining (0877T-0880T), and image-guided prostate biopsy (0898T).
Genetic counseling. CPT deleted code 96040 for genetic counseling services and replaced it with 96041. A genetic counselor must provide the service, and the duration requirement changed from face-to-face time to total time on the day of the encounter. Genetic counseling services provided by a physician or other QHP are still reported using the appropriate E/M code.
Education and training for patient self-management. These services (CPT 98960-98962) are provided by nonphysician QHPs to teach patients how to effectively self-manage illness/disease or delay disease comorbidity in conjunction with the patient's professional health care team. CPT revised the introduction to this family of codes to require a standardized curriculum consistent with guidelines or standards established or recognized by a health care professional society or other appropriate source. The changes are not applicable to clinical staff, only QHPs such as dietitians, therapists, social workers, and speech-language pathologists.
Updated language. The CPT Editorial Panel standardized language to describe clinical staff members who work under the supervision of a physician or other QHP. The new term is “Nonphysician qualified health care professional.” The change does not affect code usage but results in many codes being considered revised for 2025 (and therefore accompanied by the ▲ symbol).
MEDICARE QUALITY PAYMENT PROGRAM (QPP) AND OTHER EFFORTS TO BOOST PRIMARY CARE
CMS made relatively few changes to the QPP for the 2025 performance year. Finalized policies of note include the following:
Maintaining the performance threshold of 75 points.
Maintaining the quality performance category data completeness threshold of 75%.
Establishing an Alternative Payment Model (APM) Performance Pathway (APP) Plus quality measure set. The new measure set will phase in measures from the Universal Foundation measure set. APP Plus will be optional for eligible clinicians, groups, and APM entities that participate in MIPS APMs. It will be required for MSSP accountable care organizations (ACOs).
Adding six new episode-based cost measures — chronic kidney disease, end-stage renal disease, kidney transplant management, prostate cancer, rheumatoid arthritis, and respiratory infection hospitalization.
Removing improvement activity weighting. Participants that report an MVP or those with the small, rural, non-patient facing, or health professional shortage area special status will report one activity. All other participants must report two.
Other notable CMS efforts to strengthen primary care. In a recent report, CMS stated that “a strengthened primary care infrastructure can produce better access to high quality care, resulting in better and more equitable health outcomes.”8 The agency pointed to the following CMMI programs as efforts to strengthen primary care:
Making Care Primary, a 10.5-year program that aims to improve care for people on Medicare and Medicaid in eight states,
States Advancing All-Payer Health Equity Approaches and Development (AHEAD), an 11-year program that provides funding to states that commit to increasing primary care payment, improving care coordination, and curbing overall cost growth, with the goal of improving population health and lowering costs.
(See the article "Navigating the Transition to Value-Based Payment: Options for Independent Practices" for more information about these and other programs.)
Additionally, CMS' ongoing support of the MSSP, the largest accountable care (i.e., value-based payment) program in traditional Medicare, remains a core example of the agency's commitment to strengthening primary care. With 480 ACOs and more than 700,000 physicians and other providers, MSSP serves nearly half of all traditional Medicare beneficiaries. Starting in 2024, advanced payments were available to ACOs caring for underserved populations.
WHAT TO DO
To be ready for the 2025 payment and coding updates, practices can do the following:
Verify your billing systems are up to date, including adding new codes, deleting old codes, and updating fee schedules.
Consider whether to start billing for APCM services by reviewing the requirements and assessing the financial impact. Review the Value in Primary Care MVP reporting option and register by the deadline (typically toward the end of November).
Make sure care teams are up to date on the new policies for hepatitis B immunizations and colorectal cancer screening.
Check with your payer relations representatives to see what CPT policy changes take effect the first of the year (e.g., which new telemedicine codes they're adopting).
If you're reporting to MIPS, review the quality and improvement activities inventories. As always, make sure your selected measures and activities are still available and the requirements have not changed. Updated inventories are available on the QPP website.
Keep watching this article online for updates on potential conversion factor relief. With luck, it may even come before the crowds thin out at the gym.
