
By offering uninsured patients a set of services in exchange for an affordable monthly fee, this practice has reduced no-shows and improved its patients’ health.
Fam Pract Manag. 2004;11(8):51-52
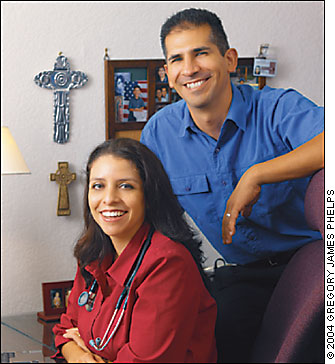
No one was surprised when Mr. Garcia missed another appointment. This was the second time in as many weeks that Mr. Garcia, a 40-year-old patient with uncontrolled diabetes and a history of chest pain, hadn’t shown up. Two years ago when Dr. Claudia Aguero-Vazquez and I opened our practice, one of the issues we swore we would address was no-shows. Having worked in both solo and large group practices, I had witnessed firsthand the problems this creates for everyone involved – physicians, staff, and, yes, patients.
I was convinced that by educating patients and enforcing the rules we could deal with the problem. Recognizing that people usually are motivated by incentives or consequences, we developed a new-patient packet that explained our expectations: Missing three confirmed appointments warranted dismissal from our practice.
I was ready to contact Mr. Garcia when it dawned on me that there might be another reason why he didn’t show. Both he and his wife are hardworking people with small startup businesses of their own. Despite these two incomes, they lacked medical insurance coverage. Even though we base our fees for self-pay patients on the Medicare fee schedule, two comprehensive appointments and his medications were enough to put him behind. Mr. Garcia had missed his appointment because he couldn’t pay for it.
Out of this realization came the Servium Plan. This plan, whose name was inspired by my wife’s high school motto, “to serve,” was to be offered to self-pay patients who demonstrated a financial need.
KEY POINTS
Patients who participate in the authors’ “Servium Plan” pay a discounted monthly fee and co-pay for an unlimited number of basic services.
The fee is based on the authors’ estimates of the number of visits most of their uninsured patients would be likely to make per year and what those patients could actually afford to pay.
These patients – and the practice – are healthier as a result.
Redefining “fee schedule”
The average patient visits the doctor three to four times a year. Since the unemployment rate in our area is 8 to 10 percent and many families are dependent on Medicaid, we figured five yearly visits should be our average, and we figured that a person like Mr. Garcia could afford to pay a certain amount for our services if he budgeted accordingly. With that in mind, we expanded the concept to enable Mr. Garcia and the other patients participating in the Servium Plan to contribute to their own subsidy pool on a monthly basis. At $35 per month per patient, 100 patients in the plan would contribute $3,500 per month or $42,000 per year to the subsidy pool, as well as $12,500 per year in co-pays (five visits per patient at $5 each).
Here’s how it works: Each patient signs an agreement that obligates him or her to pay $35 per month plus $5 per visit in exchange for a certain set of services. The agreement outlines that the patient is not eligible for or is not currently covered by any medical insurance program. It requires the patient to leave the program once he or she becomes eligible for an insurance plan through a public or employer plan. The agreement further requires the patient to deposit an undated, signed check for three months’ payment. Future payments can be made by the month. The patient may access our services as many times as needed. Office visits, rapid screens, tympanograms, electrocardiograms, vaccines and limited lab studies such as complete blood counts and basic metabolic panels are all covered services.
The Servium Plan gives patients both an incentive and a consequence to influence their behavior: If I keep my appointment, I get access to quality care without the worry of having to choose between putting food on my table or paying for an office visit.
Serving a need
It’s our third year in practice, and roughly 100 of our 1,700 patients are considered self-pay patients; 17 of these have accepted our offer to participate in the Servium Plan. Patients enrolled in the plan seem to appreciate the assistance they are getting. They show their thanks by paying on time and by bringing small tokens of gratitude such as a mango tree, fruit and pies.
As with any managed care plan, we cannot let the Servium Plan account for a large percent of our revenue, so we plan to restrict enrollment to 100. Other practices in our area are intrigued by our plan. We hope to convince 20 more practices to do the same for 100 patients. If so, we can affect the lives of 2,000 people in our area of the country. We have discussed the possibility of approaching local employers who do not offer health benefits to talk with them about our plan.
As for Mr. Garcia, he’s five months into the plan, has yet to miss an appointment and always makes his payment by the first of each month. His glucose is well controlled, and he is on the road to preventing the costly medical intervention he would have required had he not participated in our plan.