
With the right workflow, patient messages can largely be managed by nursing and support staff, relieving clinicians’ in-basket burden.
Fam Pract Manag. 2023;30(4):7-11
Author disclosures: no relevant financial relationships.

Prior to widespread implementation of the electronic health record (EHR), non-face-to-face patient contact with the primary care clinician's office was traditionally limited to telephone calls during office hours or patient voicemail messages after hours. Practices used telephone triage and medical advice protocols to ensure that patient calls or messages would be managed in a standardized way by the appropriate person in the practice.
Today, EHRs offer the use of patient portals, which allow unfettered patient-initiated messaging to the clinician at all hours of the day. This marks a major step forward in patient communication with the health care team but also marks a significant increase in indirect patient care needs. In primary care, these patient queries cover the gamut of health care needs, including appointment or referral requests, referral status updates, financial or insurance questions, result clarification, clinical advice requests, and medication requests (new or refill). Additionally, traditional phone calls are converted to EHR messages, which adds to the EHR message burden. While protocols and procedures on how to best manage patient telephone calls are well established, similar systems have not been widely adopted for electronic communication from patients.
This article describes how an academic family medicine practice designed and implemented a system for optimally managing electronic patient messages. Our multiple part-time clinicians comprise approximately 8.8 clinical FTEs managing a panel of 16,000 patients. The clinical team also includes 15 registered nurses (RNs)/certified medical assistants (MAs)/licensed practical nurses (LPNs), two triage RNs, two licensed clinical social workers, and one clinical pharmacist.
KEY POINTS
Patient portals mark a major step forward in patient communication with the health care team, but they also mark a significant increase in indirect patient care needs.
Practices should reconsider the clinician's role in message management.
By clarifying rules for routing and replying to patient messages, workflows can largely be handled by nursing and support staff.
A NEW WORKFLOW FOR PATIENT MESSAGES
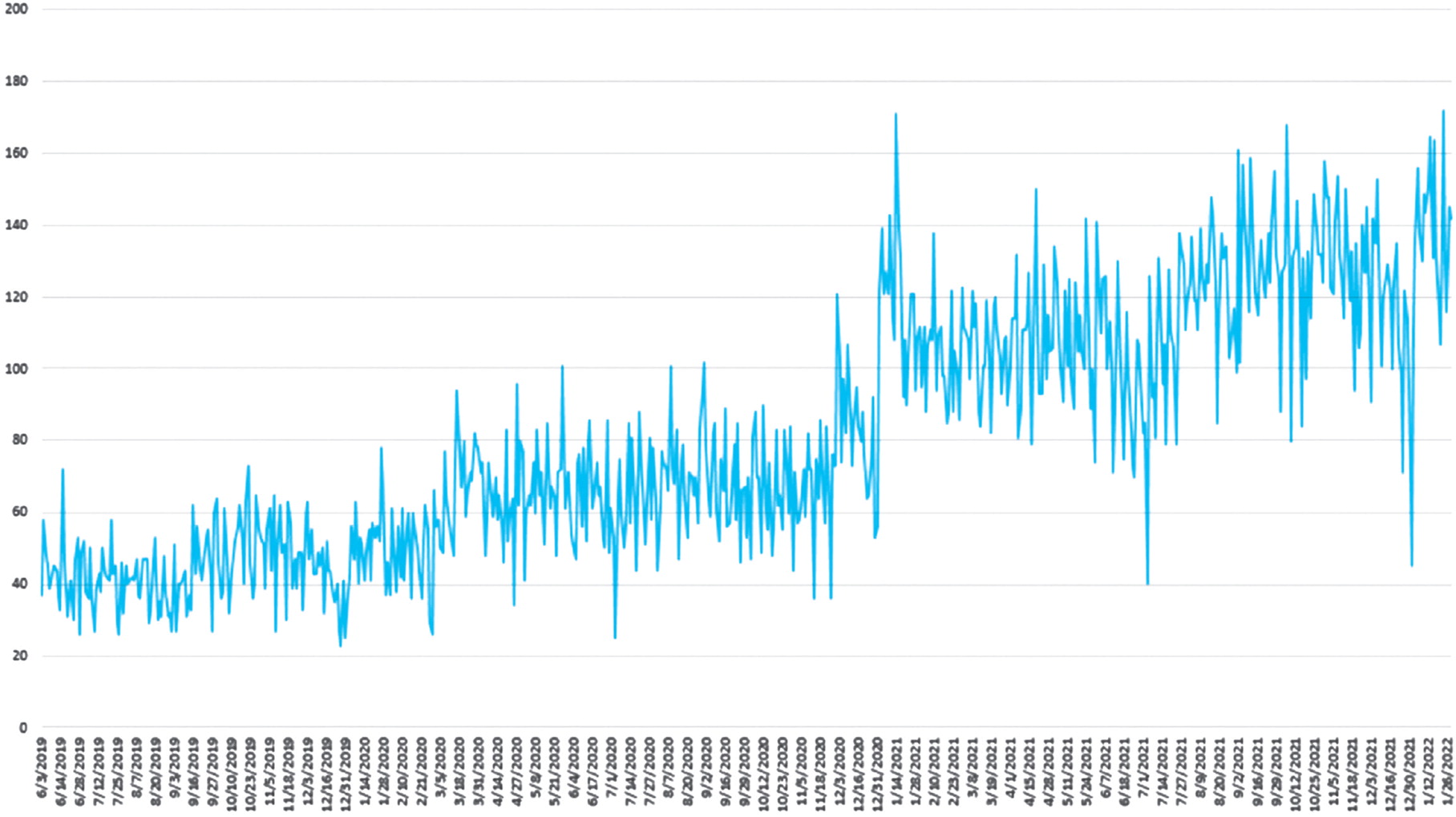
Before this intervention, all patient messages went directly to the clinician, who then decided whether to handle a message personally or forward it to another team member. As the volume of messages increased and response times increased, this strategy of having the clinician review all messages became non-viable.
Our first step in developing a new work-flow for managing patient messages was to assemble a small multidisciplinary work team with representatives from administration, nursing, and clinicians. The over-arching goal was to develop a consistent, systems-based approach to patient messaging and to get “the right message to the right team member.”
The group surveyed clinicians about their message preferences. Overall, clinicians preferred that all messages be reviewed and filtered first by a non-clinician team member. Clinicians only wanted certain messages routed to them — mostly medication questions about directions for use, side effects, or dose adjustments. For messages involving symptoms not improving despite treatment, their preference was to not have the message routed to them but to have the patient scheduled for a follow-up visit. Most other messages could be handled by staff or converted to a visit.
Using the clinician survey results, the team reviewed the different types of messages available in the patient portal (new complaint, medication refill, billing question, etc.) and determined which message types should go to which team members first. Input from nursing staff was essential in ensuring that the most appropriate message ended up in front of the correct person. (See the workflow.)
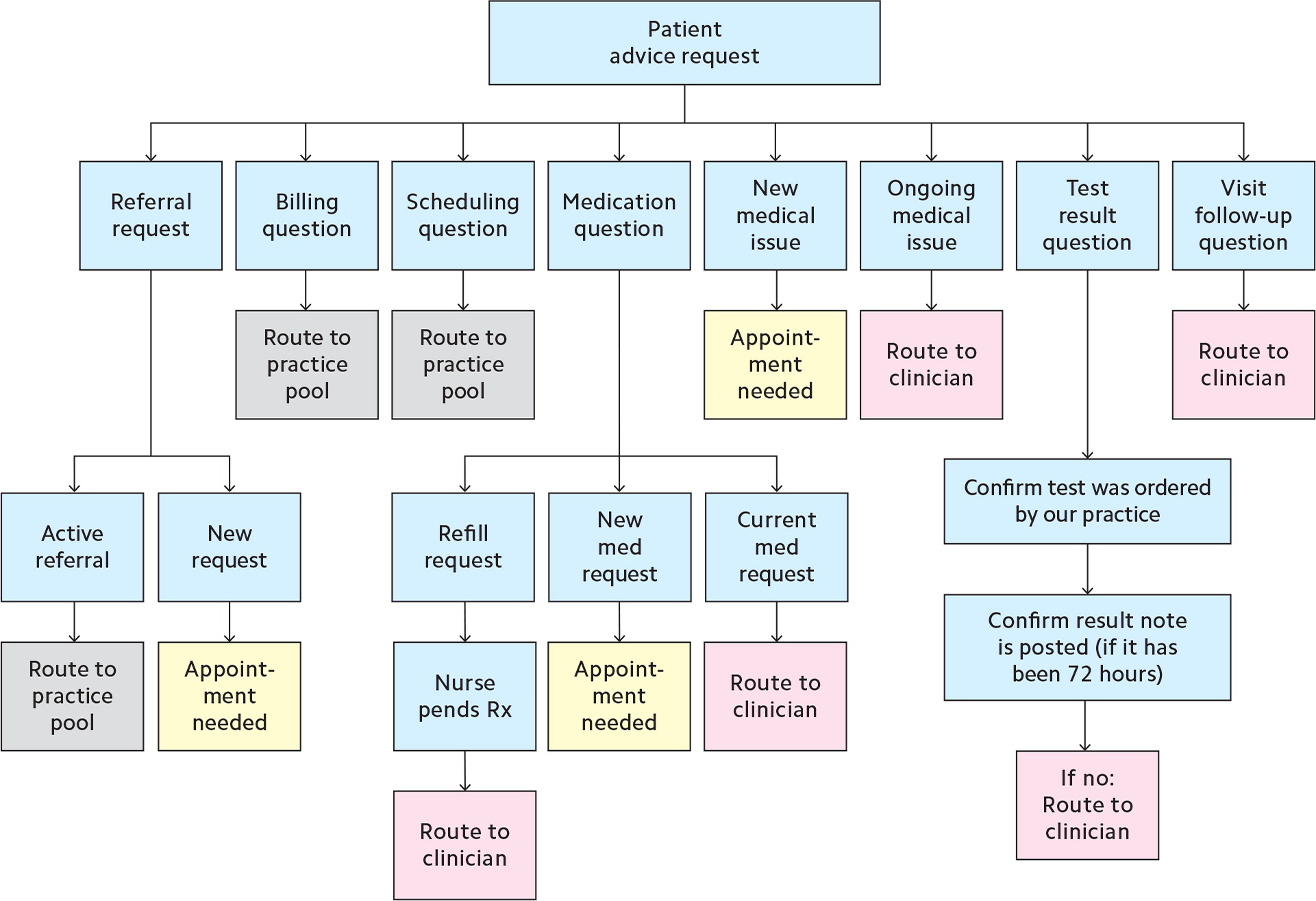
The next step was to expand the practice pools for message routing. (See a selected list of practice pools.) All patient-initiated messages would first land in a general practice pool, and an RN would read and review all messages from this initial pool. We used RNs as the first-line filter for two main reasons. The first is practical. Our MAs' and LPNs' main duties are related to direct clinical care provided to the patients seen in the practice, whereas our RNs have more of an administrative/supervisory role. The second is clinical. If patient messages include issues that are clinical in nature, the RN is able to appropriately triage these patients for clinical visits. The team considered whether message filtering should be done by nonclinical team members; however, after discussion, the group determined there were no available nonclinical staff to do this work and a clinical team member was better suited for it. This first-line filtering is critical since patient messages are not first reviewed by a clinician.
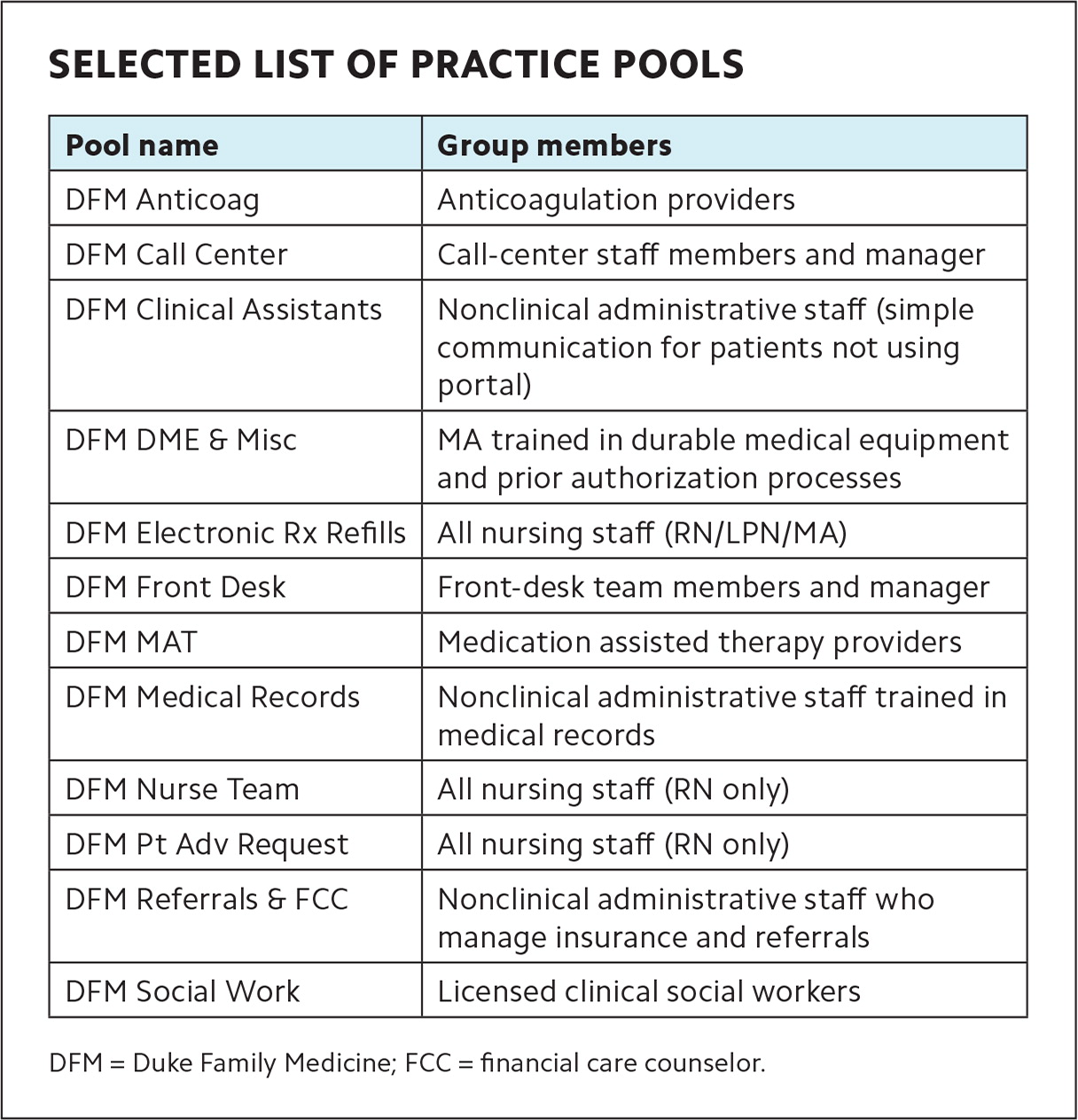
| Pool name | Group members |
|---|---|
| DFM Anticoag | Anticoagulation providers |
| DFM Call Center | Call-center staff members and manager |
| DFM Clinical Assistants | Nonclinical administrative staff (simple communication for patients not using portal) |
| DFM DME & Misc | MA trained in durable medical equipment and prior authorization processes |
| DFM Electronic Rx Refills | All nursing staff (RN/LPN/MA) |
| DFM Front Desk | Front-desk team members and manager |
| DFM MAT | Medication assisted therapy providers |
| DFM Medical Records | Nonclinical administrative staff trained in medical records |
| DFM Nurse Team | All nursing staff (RN only) |
| DFM Pt Adv Request | All nursing staff (RN only) |
| DFM Referrals & FCC | Nonclinical administrative staff who manage insurance and referrals |
| DFM Social Work | Licensed clinical social workers |
After reviewing a message, the RN routes it to the appropriate team member/practice pool to handle and notifies the patient of the expected response time. For example, if a patient is asking about an active referral request, the RN can route the message to the “referrals” practice pool, which includes nonclinical administrative staff who manage insurance and referrals. A member of the pool will then handle the message. (See the workflow.)
To assist RNs with message management, our project leader developed reference documents and SmartPhrases. These phrases, also known as “dot phrases,” allow staff to easily insert commonly used chunks of text into their responses to patient messages by typing a period (dot) followed by a short user-generated phrase. (See the list of SmartPhrases.) The project lead and nursing leadership also offered training sessions for team members who would be reviewing and filtering messages. The practice did not hire additional staff. The nursing staff was up-trained to do this work, and it has been incorporated into their clinical responsibilities. We piloted the new work-flow using select clinician EHR in-baskets. Once refined, it was rolled out to the entire practice.
LESSENING THE CLINICIAN IN-BASKET BURDEN
The following example contrasts the old and new workflows and illustrates how the change has positively affected clinician workload.
Patient message: “Dear Doctor, you saw me six weeks ago, and at that time you put in a referral to podiatry, but I have not yet heard back.”
In the old workflow: This message would have gone to the clinician, who would have done two things: 1) message the patient back, letting them know that a team member would look into their question, and 2) forward the message to the referral coordinators. The referral coordinators often-times would then send information back to the clinician, who would then notify the patient of the referral status.
In the new workflow: This message is reviewed by an RN, who responds to the patient using standard language and forwards the message to the referral coordinator, per the routing rules. The referral coordinator reviews the file and contacts the patient with the referral status and any instructions. In this example, the clinician is only involved if there is an issue, for example, if the referral was never placed.
FEEDBACK AND LESSONS LEARNED
Informal feedback on the new workflow indicates increased clinician satisfaction, improved clinical efficiency, and improved staff satisfaction. Clinicians indicate that messages coming to them are more likely to be clinician-level issues and their individual in-basket burden has lessened. Overall, our team felt that message turnaround times decreased significantly and we were able to review and disperse more messages to the appropriate next location.
While we do not have formal feedback from patients about this process, we have found that the closed-loop communication from the RN has been helpful for letting patients know that their message has been received and what the next steps will be, which may include a visit with the clinician. Our nursing staff have noted some dissatisfaction from patients who felt they were receiving canned responses, so we encourage personalized messages as appropriate. Nurses can decide whether or not to use SmartPhrases.
If patients indicate that they want their message sent to their clinician, we do that and set expectations around a timeline for their response. Clinicians are free to respond however they choose. They often support the advice provided by nursing staff, which reassures patients.
This new workflow has put more onus on each team member at each step in the message management process. Nursing and clinical support staff have indicated that they now feel empowered to act on items they can own. This has resulted not only in better message management but also meeting patients' needs in a timelier manner.
We anticipate that technology will continue to advance and improve additional aspects of in-basket management. Some EHRs may have an “auto-response” feature built in, which could help inform patients of expected response times or next steps. It is not hard to imagine that soon practices will be able to use “chat-bots” or other artificial intelligence modalities to filter or reply to messages, or to address patient needs electronically. Until such time, workflows such as ours can be used to relieve clinician burden and serve as a template to drive future change.
SmartPhrase name |
Response to patient message (stock language) |
Message routed to |
.inbbilling |
We have received your message about a billing question. Your message has been forwarded to the billing team for further review. For immediate assistance regarding your bill, please call Customer Service at ***-***-**** (local) or 1-800-***-**** (toll-free). Hours are 8:00 am to 5:00 p.m. Monday, Tuesday, Wednesday, and Friday and 8:00 am to 4:00 pm Thursday. |
DFM Referrals & FCC |
.inbdme |
Thank you for reaching out about durable medical equipment (DME). This request has been forwarded to your health care team for review. Many insurance companies require an office visit with a clinician before authorizing these supplies or equipment. If an appointment is required, you will be contacted before any paperwork is started. Please allow 5 to 7 business days for completion and processing of these order forms, if appropriate. A staff member will notify you when this request is complete. |
DFM DME & Misc |
.inbnewissue |
Thank you for reaching out; however, the best way to address this health concern with your clinician is to schedule an appointment. To schedule, call ***-***-**** (option 1). Please be aware that many of our clinicians are not necessarily in clinic every day, so if your PCP is unavailable, you are welcome to schedule with another one of our clinicians. In addition to offering office visits, many of our clinicians also offer virtual visits. |
No routing |
.inbreferralactive |
Thank you for inquiring about your current referral. Your message has been forwarded to the referral coordinating team for further review and assistance. If you are requesting further recommendations for choosing a clinician in the specialty field you were referred to, your message will be forwarded to your clinician. Please allow three business days for a response. If there is no response, we may not have any recommendations for a specific clinician Note: After a referral has been ordered by your clinician, there is a 24-business-hour processing time for ASAP or urgent referrals and a 48-business-hour processing time for routine referrals. |
DFM Referrals & FCC |
.inbresultcomment |
Your clinician sent you a specific note about this lab or imaging test. To review your clinician's notes on your recent lab or imaging tests, please click on "Test Results." You will need to select each test result individually. The note will be under "Comment from Doctor's Office," which appears above the result value or narrative. Please let us know if you have further questions about your clinician's notes to you about these results. |
No routing |
.inbresultunviewed |
Your clinician has not yet reviewed the lab test or imaging test result. After your clinician reviews the result, we will send you a specific note about this result. Please be aware that clinicians have up to 72 business hours to review results. To review your clinician's notes on your recent lab work, click on "Test Results." You will need to select each test result individually. The note will be under "Comment from Doctor's Office," which appears above the result value or narrative. Please let us know if you have further questions about your clinician's notes to you about these results. |
No routing |
.inbroutetopcp |
Your message has been received and will be forwarded to your clinician for review. If a response is being requested, please allow up to three business days for a response to your message. Duke MyChart messaging is for non-urgent issues. If you require more immediate attention or are having a symptom-based complaint, please contact our office directly at ***-***-****. |
Clinician |
.inbscheduling |
We have received your message. One of our team members will reaching out to you by telephone or MyChart to discuss scheduling in more detail. During regular business hours, you can reach our call center staff at ***-***-**** (option 1). If this is in regards to an appointment for imaging, you may contact this scheduling team at ***-***-****. There is also an option for managing your appointments via MyChart. Please be sure your telephone ringer is turned on and your voicemail box is empty so we can leave a message if we are unable to reach you. |
DFM Call Center DFM Front Desk |
.inbtriage |
Thank you for reaching out. We are trying to speak with you by telephone to better asses your symptom-based concern. Please call back at ***-***-**** (option 8) to reach our triage nurse. MyChart messages are not used for discussion of urgent matters. |
DFM Pt Adv Request |
.inbvisitfu |
Your message has been sent to the clinician you most recently had an appointment with. Please allow three business days for a response to your message. |
Clinician
|
.inbworkletter |
Thank you for reaching out about a letter for work. The request for a work excuse or restrictions requires a clinician approval. This message was forwarded to the clinician you recently saw for this issue. Please allow three business days for review and completion, if appropriate. The document will be available in the “Letters” portion of your MyChart. |
Clinician
|
