
Team-based care improves quality and efficiency while making practice more sustainable. Here's how to better advocate for getting the help you need.
Fam Pract Manag. 2023;30(4):31-37
Author disclosures: no relevant financial relationships.

The physicians at your group practice have been looking at models to help manage the exploding volume of non-visit work, including responding to in-basket messages, coordinating referrals, and managing prior authorizations. The physicians believe that bringing on a referral coordinator and a licensed vocational/practical nurse to manage these tasks would make their work more sustainable. You were nominated to share the idea with leadership and secure their support, but you have no idea where to start.
Team-based care has clear advantages for improving care quality, the patient experience, and the sustainability of practicing primary care. Family medicine physicians are often tasked with making a business case to their organization's senior leadership to justify additional personnel, a task that can feel daunting. Learning how to present the benefits of expanding team-based care in terms that resonate with leadership is essential for obtaining buy-in. This article presents five strategies to build a business case for investing in the care team.
KEY POINTS
Team-based care models have been shown to improve access/capacity, population health, patient experience, and costs while making the practice of primary care more sustainable for physicians.
Getting leadership to invest in the primary care team may require presenting a business case that speaks to the organization's priorities and considers various payment model incentives.
Increased productivity is a compelling argument; with an optimized team, physicians are freed from lower-level tasks and their productivity increases, which drives improvements across other key metrics.
1. UNDERSTAND YOUR AUDIENCE
Seeking to understand the perspectives and priorities of key leaders and stakeholders is an important first step. This can often be accomplished with an “inquisitive interview.” Before making a formal pitch to your leadership team, approach a supportive person in senior leadership for advice. Explain what you would like to do, and ask how they would approach it. In particular, try to understand the answers to these questions:
What are the health system's pain points? Can the proposed team model help address those? For example, excessive patient wait times due to inadequate access is a common concern, so showing ways that team-based models expand visit capacity would be important. Poor ratings on patient experience surveys may be another area of concern, so showing how the model would improve patient communication or reduce cycle times or wait times could be beneficial.
How does the proposed team model relate to things that are important to the organization? Consider system priorities reflected in the organization's mission statement, financial or regulatory pressures, or quality improvement initiatives. For example, if providing superior patient experience is a core principle of the organization, you would want to show how the team model can help with this.
What would convince stakeholders that the proposed team model is feasible in the long term? What would they consider an adequate return on investment? For example, how much of an improvement in population health quality metrics or visit volumes would they consider significant enough to sustain the model? Understanding which specific metrics your leadership team would be looking at will help you present your business case more effectively.
2. UNDERSTAND YOUR PAYMENT INCENTIVES
Different payment mixes shift the financial incentives within a health system and, consequently, determine which metrics would be most impactful to target. While the predominant payment model nationally continues to be fee for service, many health systems receive at least some funding from other models (see “Common payment models”). Exploring the proposed team model's potential impact on each relevant funding stream uncovers how it may benefit the health system.
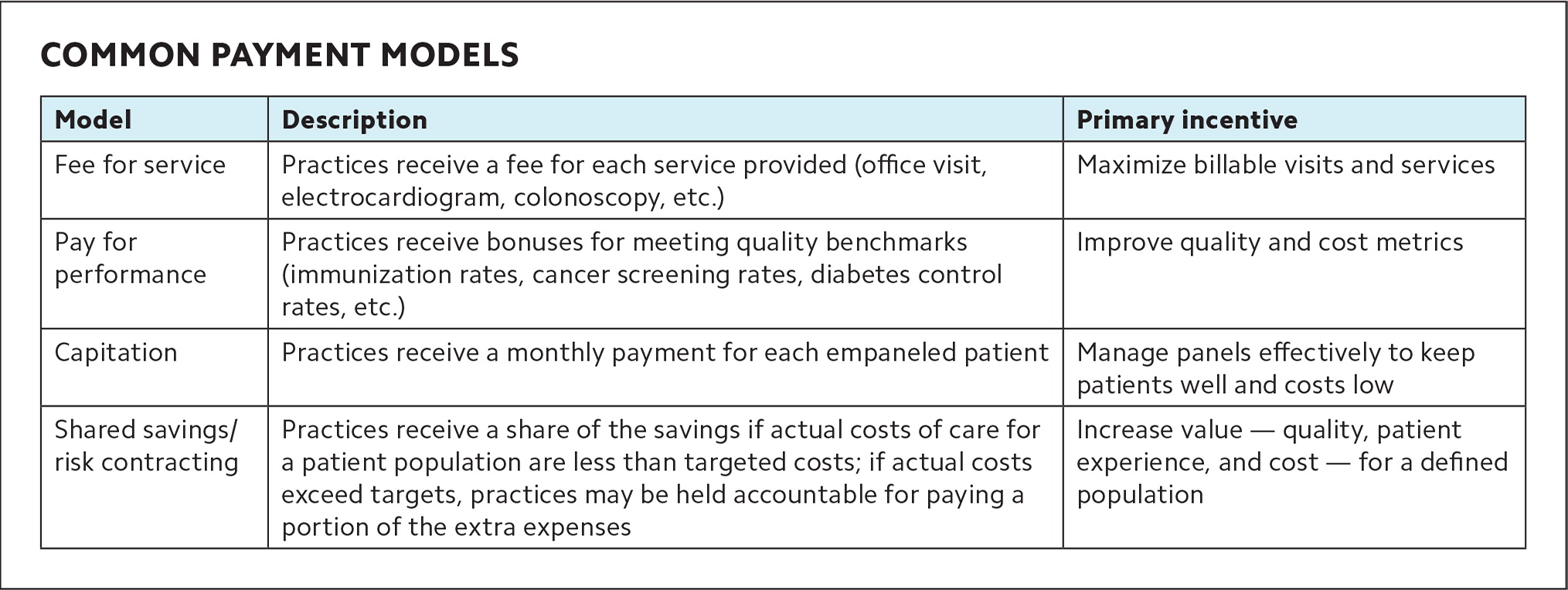
| Model | Description | Primary incentive |
|---|---|---|
| Fee for service | Practices receive a fee for each service provided (office visit, electrocardiogram, colonoscopy, etc.) | Maximize billable visits and services |
| Pay for performance | Practices receive bonuses for meeting quality benchmarks (immunization rates, cancer screening rates, diabetes control rates, etc.) | Improve quality and cost metrics |
| Capitation | Practices receive a monthly payment for each empaneled patient | Manage panels effectively to keep patients well and costs low |
| Shared savings/risk contracting | Practices receive a share of the savings if actual costs of care for a patient population are less than targeted costs; if actual costs exceed targets, practices may be held accountable for paying a portion of the extra expenses | Increase value — quality, patient experience, and cost — for a defined population |
In fee-for-service payment, the primary incentive is to maximize billable visits and services using billing codes whenever possible. Certain nonphysician team members can provide a variety of billable services. For example, registered nurses (RNs) can bill for annual wellness visits, chronic care management, and transitional care management using specific Medicare codes; clinical pharmacists can bill for certain services using “incident to” billing; and licensed clinical social workers and psychologists can bill for some of their visits. Current reimbursement for such codes may not be sufficient to cover all costs associated with providing these services but can partially offset them, at least. Even when nonphysician team members cannot bill for services, they can often contribute to services, which decreases the time required by physicians and frees them for higher-value work.
Some creativity will likely be needed to further demonstrate the value of the proposed team model under fee-for-service payment. RN co-visits can work well. In this model, RNs are trained to do most of the history-taking, exam, scribing, and pending orders for straightforward visits, and the clinician spends about five minutes with the patient to confirm the plan. The visit adds capacity to the physician's schedule, is fully billable, and increases access for patients. Similarly, if other team members can contribute to clinician efficiency and sustainably allow an additional 1–2 billable visits per half day, this is beneficial under fee-for-service.
In pay for performance, the primary incentive is to improve metrics. Therefore, you will need to understand what your organization measures, which metrics have room for improvement, and which ones could benefit from the proposed team model. Consider common metrics for screening rates and disease control as well as safety or patient experience. For example, if cancer screening rates are a priority metric in your organization, having additional staff support to help close care gaps would be beneficial.
In capitation, the primary incentive is to keep patients well. Because practices receive per-member-per-month payments not tied to visits or billable services, this model supports nontraditional encounters and outreach designed to prevent or manage illness and keep patients out of the hospital. The proposed team model can add to the business case through increased rates of prevention, better chronic disease management, reduced health care costs/hospitalizations, and other quality indicators. Additionally, when more team members help clinicians manage a panel, the panel size can grow, which brings in more capitation dollars.
In shared savings/risk contracting, the primary incentive is to increase value, which takes into account quality, the patient experience, and cost. Here again, the proposed team model can add to the business case through improved prevention and screening, better chronic disease management, reduced health care costs/hospitalizations, and other quality indicators. For this model to be effective, the savings need to be shared with primary care.
3. REVIEW EVIDENCE FOR THE PROPOSED TEAM MODEL
The literature is rife with data and success stories to support various team-based care models. Improvements may involve just the core team, e.g., a clinician and medical assistant (MA) responsible for a panel of patients, or may include the extended care team, which supports several core teams. Some studies have mapped out proposed staffing ratios and costs for comprehensive primary care teams, which may be helpful as a reference.1–2 Compile data on how your specific roles of interest can affect quality of care, access, clinician/staff/patient satisfaction, and other metrics. See the examples of supportive evidence for particular team-based care improvements.
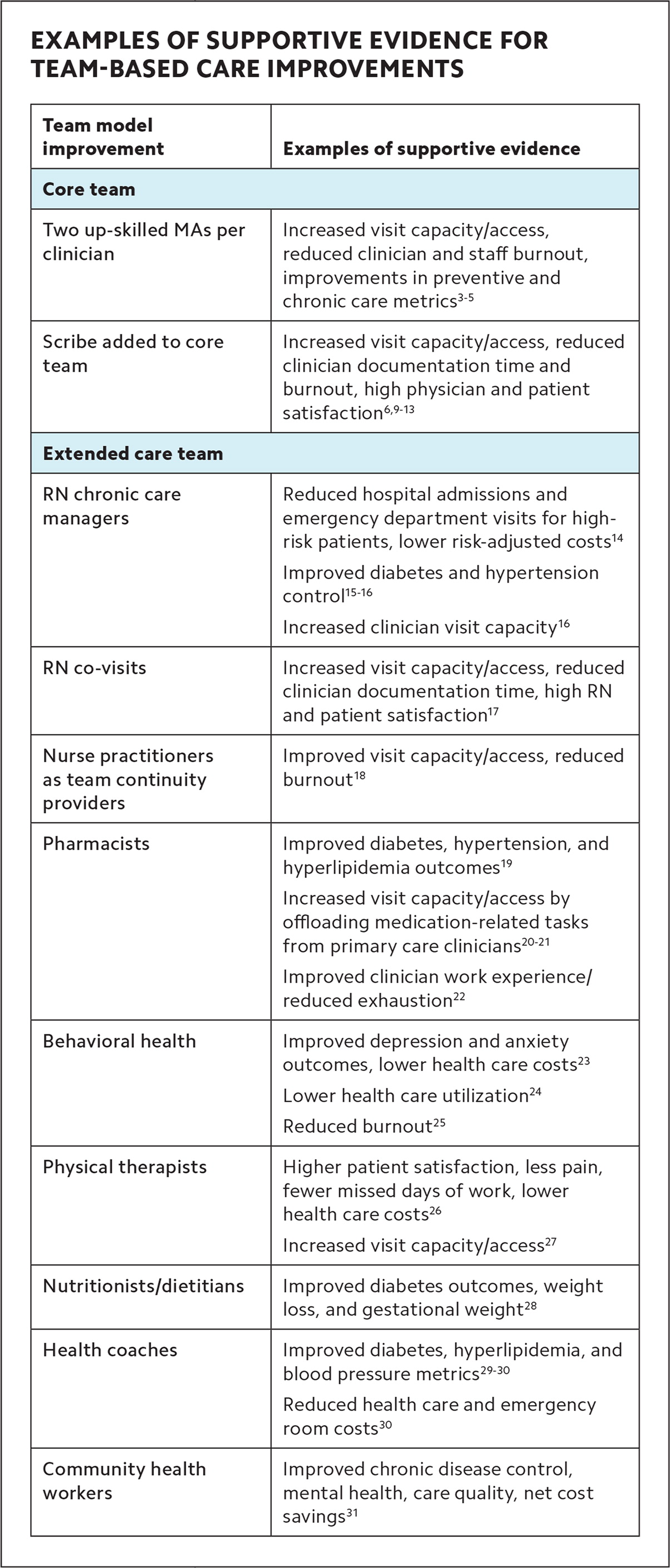
| Team model improvement | Examples of supportive evidence |
|---|---|
| Core team | |
| Two up-skilled MAs per clinician | Increased visit capacity/access, reduced clinician and staff burnout, improvements in preventive and chronic care metrics3–5 |
| Scribe added to core team | Increased visit capacity/access, reduced clinician documentation time and burnout, high physician and patient satisfaction6,9–13 |
| Extended care team | |
| RN chronic care managers | Reduced hospital admissions and emergency department visits for high-risk patients, lower risk-adjusted costs14 Improved diabetes and hypertension control15–16 Increased clinician visit capacity16 |
| RN co-visits | Increased visit capacity/access, reduced clinician documentation time, high RN and patient satisfaction17 |
| Nurse practitioners as team continuity providers | Improved visit capacity/access, reduced burnout18 |
| Pharmacists | Improved diabetes, hypertension, and hyperlipidemia outcomes19 Increased visit capacity/access by offloading medication-related tasks from primary care clinicians20–21 Improved clinician work experience/reduced exhaustion22 |
| Behavioral health | Improved depression and anxiety outcomes, lower health care costs23 Lower health care utilization24 Reduced burnout25 |
| Physical therapists | Higher patient satisfaction, less pain, fewer missed days of work, lower health care costs26 Increased visit capacity/access27 |
| Nutritionists/dietitians | Improved diabetes outcomes, weight loss, and gestational weight28 |
| Health coaches | Improved diabetes, hyperlipidemia, and blood pressure metrics29–30 Reduced health care and emergency room costs30 |
| Community health workers | Improved chronic disease control, mental health, care quality, net cost savings31 |
4. TRANSLATE YOUR VALUE ARGUMENT INTO TERMS AND METRICS PERTINENT TO ORGANIZATIONAL PRIORITIES
As you prepare your pitch to the chief financial officer (CFO) or other senior leadership, include talking points and perhaps a one-page handout or short slide presentation. Use the context obtained in the previous steps to demonstrate how the proposed team model will meet the organization's needs.
Describe the impact on key metrics. For example, additional staff could improve screening rates and disease management, leading to better population health metrics and higher payments, depending on your payment model. See “Potential metrics for team-based care.” Remember to consider non-financial metrics of value to the health system as well. These could include equity, access, patient experience, or safety. To get specific data on metrics for your clinic or system, turn to your practice manager, electronic health record, IT support team, quality improvement leaders, or others at the system level who could help.
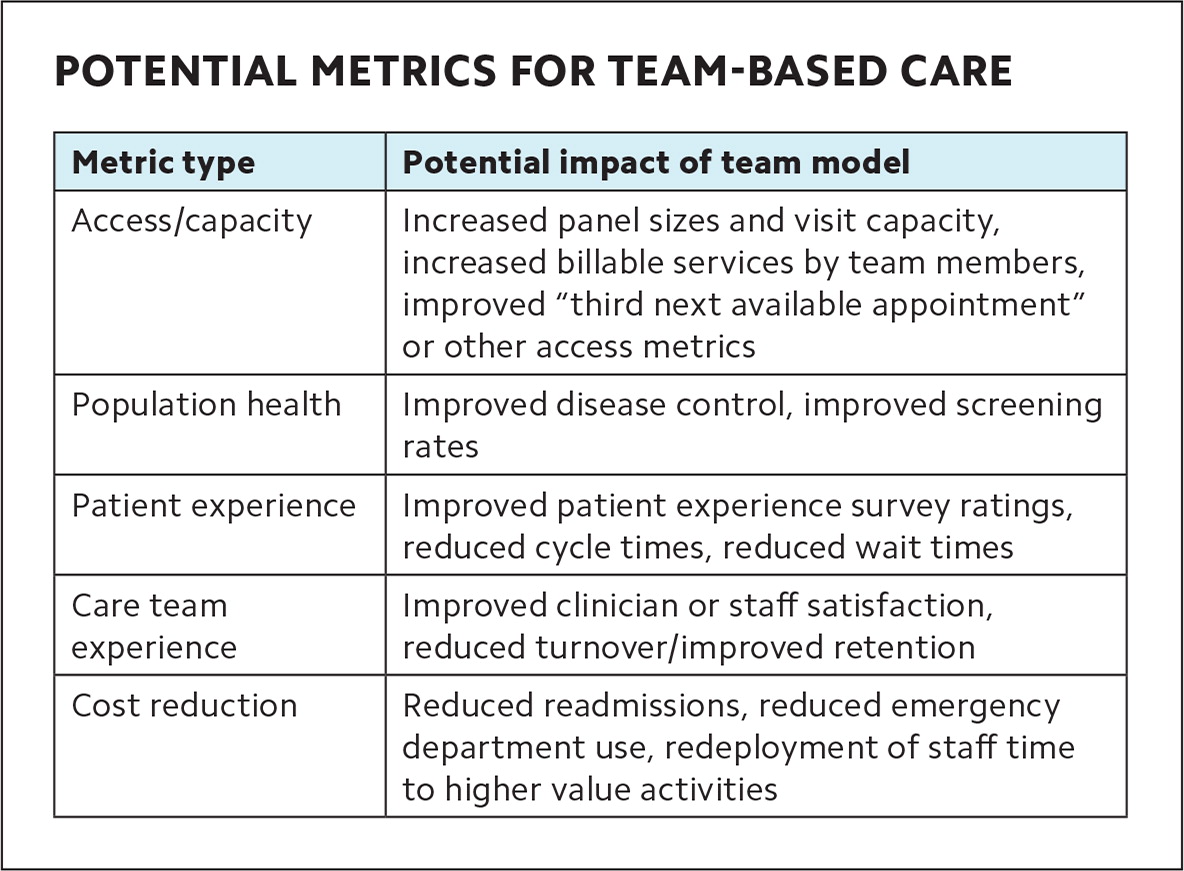
| Metric type | Potential impact of team model |
|---|---|
| Access/capacity | Increased panel sizes and visit capacity, increased billable services by team members, improved “third next available appointment” or other access metrics |
| Population health | Improved disease control, improved screening rates |
| Patient experience | Improved patient experience survey ratings, reduced cycle times, reduced wait times |
| Care team experience | Improved clinician or staff satisfaction, reduced turnover/improved retention |
| Cost reduction | Reduced readmissions, reduced emergency department use, redeployment of staff time to higher value activities |
Highlight productivity gains. This is a powerful argument. When practices have the right people on the team and everyone is working at the top of their license, physicians are freed from lower-level tasks and their productivity increases. This drives improvements across other important metrics such as access/capacity and costs. In core team models such as those used within Bellin Health and University of Colorado,3–5 the increased efficiency of the 2:1 core team (2 MAs per physician) allows an additional, sustainable 1–2 visits per clinic session, which offsets the costs of the second MA/care team coordinator while expanding access/capacity. Similarly, in one study, the reduced documentation time and increased physician productivity from the use of scribes was projected to result in more than twice their costs in revenue.6 In extended team models, where chronic care RNs or clinical pharmacists provide routine hypertension or diabetes follow-up visits, for example, this frees the primary care clinician to see other patients on the panel, which improves access. Consider where physicians or staff could be redeployed to higher-value activities through the proposed model and how this could improve capacity, costs, or other metrics. If adoption of the team model is contingent on increased productivity (e.g., greater numbers of visits or larger patient panels), those expectations need to be transparent to clinicians and front-line staff from the start.
Address potential avoided costs. Any discussion of the benefits of team-based care should take into account the costs of not making improvements to the team model, such as the costs of burnout and increased turnover. One study estimated that the cost of turnover for an MA was $14,200 in 2017; with a 59% turnover rate in the study, that resulted in a total cost of $213,000.7 In another study, during a transition to team-based care with expanded MA roles, MAs reported greater job satisfaction despite also reporting a higher workload.8 AMA STEPS Forward estimates the cost of physician turnover at two to three times their annual salary and provides a calculator for the organizational cost of turnover due to physician burnout. If the proposed team model can realistically address issues that are causing clinicians and staff to leave or reduce their hours, the savings add up quickly.
Take the long view. Consider the long-term perspective and priorities for your health system to better reflect big-picture benefits of the team model. For example, will your system be moving toward value-based care, and would the proposed team model help your practice prepare for the change in incentives? Is the health system seeking a greater market share or relying on primary care to channel patients to other parts of the system, which would justify investment in the primary care team? Describe what the costs might be of a reduced market share caused by not meeting the needs of the patient population and how the team model would help address those needs (e.g., prompt access, equity, safety, and patient experience).
Show the math. The business case will be more compelling if you support your proposed benefits and costs with budget estimates. This includes a realistic acknowledgment of the expenses of the staffing model, including additional salary, benefits, training, and onboarding costs. If the model involves part, but not all, of a staff member's time such that some of the staff member's time would be covered by other sources, prorate these costs accordingly. Similarly, use historic data to price out projected benefits of the model. Include the short- and long-term contributions from various dimensions, including billable services provided directly by the team member, additional billable services other team members will be able to provide with the team member's support, additional pay-for-performance dollars with expected quality metric improvements, and reduction in turnover costs. Use this data to calculate the return on investment in the team model. See the “Proposal planning worksheet” to help outline your proposal.
PROPOSAL PLANNING WORKSHEET
Use this worksheet to draft your team-based care proposal. Keep answers concise and focus on the most impactful points.
1. Current state/problem: Briefly describe the current situation, using specifics whenever possible.
Examples: “Clinicians are spending an estimated X hours per week on administrative tasks that do not require medical decision-making” or “A1C rates are persistently low, resulting in missed opportunity for $X in pay-for-performance dollars.”
2. Impact of the problem on metrics of concern: List major metrics of concern to the health system and describe the impact of the problem in terms of priority metrics.
Examples: “Clinician turnover is at an all-time high at X%, costing the health system an estimated $Y per year on recruiting and training costs. This also limits patient access as the clinic is functioning at Z% capacity due to difficulty hiring” or “We are under pressure from our primary payer to reduce preventable readmissions, but we struggle as a system to connect with patients within three days of discharge.”
3. Proposed solution: Briefly describe the proposed team model that will address the problem, including references to data supporting the impact of the model if possible.
Example: “We propose hiring a nurse chronic care manager to help with patient education, medication management, and lifestyle modification counseling for patients with diabetes or hypertension. Studies have shown that an RN care manager can successfully improve diabetes and hypertension control rates.”
4. Projected impact of the solution on metrics of concern: Consider major metrics of concern to the health system and describe how the team model may directly or indirectly affect these.
Examples: “A nurse transitions coordinator who could connect with patients before and after discharge could dramatically improve the quality of our post-hospital follow up and reduce readmissions” or “An RN chronic care manager would offload some chronic care visits from our primary care clinicians to improve access while improving our chronic care quality metrics.”
5. Projected net benefit: Use available system data to make reasonable estimates of the financial impact of the model. Outline the major ways it may increase payments/funding or save costs, and compare the increased revenue to the rough annual costs needed for the model.
Example: “Time saved on documentation by hiring a scribe would allow clinicians to see one additional patient per clinic session, which averages to an additional $X per year. This offsets the $Y annual salary needed to fund a full-time scribe. Further savings would be made by reducing turnover from clinician burnout.”
6. Proposed next steps: List a few next action steps to implement the model, such as setting up a meeting with the relevant managers or planning a small pilot.
5. KEEP MOVING FORWARD
Be prepared for the likelihood that you won't get everything you ask for from leadership. If you initially get a “no,” you may need to refine your argument and try again in a few months. Another option is to ask for a small pilot project — for example, giving one team an additional team member for one year or carving out part of one staff member's time for population health outreach targeting a priority metric of the health system. A small pilot of the proposed team model can act as proof of concept and help the organization assess the true benefits and costs. This may also be an easier initial step for system leadership to invest in or fund through grants.
Choosing and tracking metrics for the pilot is critical, as it will affect your future ability to advocate for scaling up the model. Metrics should capture short-term benefits as well as potential indicators of long-term benefits (for example, a staff satisfaction survey as a proxy for future burnout/turnover impact). If the model's sustainability is contingent on a specific metric (e.g., productivity), make sure the team knows what that metric is — and is tracking and prioritizing it. This aligns sustainability of the business case with front-line staff's priorities. Create feedback loops that include both leadership and front-line staff to ensure data transparency.
PUTTING IT ALL TOGETHER
The day has arrived, and you have an hour with the CFO. She listens carefully to your pitch about the proposed team model and then starts to list all the reasons why it won't work for the health system at this time. You are well prepared and present data on how the model would make larger patient panels sustainable while improving panel management, which aligns with an upcoming shift to increased capitation. You also describe how excessive in-basket time is negatively affecting clinician productivity and satisfaction, and you provide estimates of how the proposed team model would lead to improvements in these areas, offsetting the staffing costs. The CFO is impressed by your comprehensive approach and sees the benefits of the team model and the need for additional personnel. She authorizes you to conduct a one-year pilot within your team with plans to expand it site-wide if specific metrics are achieved.
