
These insider tips can save you time by putting your imaging requests on the path to easier approval.
Fam Pract Manag. 2024;31(1):7-11
Author disclosures: no relevant financial relationships.

Prior authorizations continually rank as one of the top administrative burdens on physicians.1 While they can be a hassle, and are perhaps used for too many medications and procedures, prior authorizations are an important tool for managing advanced imaging, which is one of the leading causes of high health care costs in the U.S.2
As a radiology benefits management clinical reviewer and a supervisor of reviewers, we would like to share some tips to help our fellow physicians avoid that dreaded peer-to-peer call request, prevent clinical denials, and generally make prior authorizations less burdensome.
KEY POINTS
Prior authorization is burdensome to physicians, but it’s an important tool for managing expensive imaging studies and can be easier if physicians and their staff follow a few key tips.
Common reasons for denials include unsent or incomplete documentation, another clinician ordering the same test, and ordering the wrong type of test (e.g., CT vs. MRI).
To ease your prior authorization burden, leverage your team, make sure you’ve included proper documentation for specific studies, and consider alternatives to imaging.
COMMON REASONS FOR DENIALS
There is often a simple explanation as to why the study you ordered for your patient didn’t get approved. Here’s what can go wrong and how to prevent it.
Documentation not sent. You may have documented everything necessary for pre-authorization, but if you or your staff don’t send that documentation to the reviewer, it is not possible for the reviewer to make the determination. The clinical reviewer assesses whether your request is medically necessary by comparing your notes with widely accepted, evidence-based clinical guidelines. (Ask the insurer for a link to their guidelines, if needed.)
Documentation sent but incomplete. If your imaging request is assigned a peer-to-peer status, then the reviewer has likely concluded that your documentation does not support your order. A peer-to-peer call is an opportunity for you to supply clarifying information. Make sure your staff sends over the correct supporting documents with completed, signed visit notes, not preliminary or incomplete notes. To support medical necessity, be sure your documentation includes key details such as relevant signs and symptoms, relevant lab or other test results, physical exam findings, prior failed treatments, contra-indicated treatments, or prior reports (for repeat studies).
Concurrent request for the same study. It is somewhat common for another office or clinician to order the same study you did, without you knowing about it. Before your study can be approved, the other study will need to be withdrawn. Sometimes another clinician’s request may have been approved, but the patient did not get the study done before the approval expired. If that’s the case, make sure that background information is in the note (“patient did not get the prior approved study, so study is still needed”).
Wrong test ordered. When evaluating a condition, it is important to order the right test for the right patient at the right time. Some ordering clinicians assume that because it is generally cheaper to get a computed tomography (CT) scan than a magnetic resonance imaging (MRI) the insurance company is more likely to approve the CT. However, in practice, this is not the case. Cost is not the only factor in the determination of medical necessity. For example, radiation exposure and study effectiveness are also considered.
One of the most common causes of denials for brain imaging is this very issue — ordering a CT instead of an MRI. If your patient is experiencing worsening headaches and you are concerned about underlying pathology, you should order an MRI instead of a CT. This produces no radiation exposure for the patient and gives you the better study for neuroimaging. If there is a contraindication to getting an MRI, make sure you put that in the documentation.
TIPS TO IMPROVE THE PROCESS
Making a few small changes in the way you order imaging studies can save you a lot of time on prior authorization.
Consider alternatives to imaging. Keeping in mind excessive radiation exposure, consider alternatives to CT when evaluating abdominal pain of unknown origin, for example. You can avoid many CT scans of the abdomen and pelvis with a proper physical examination, laboratory and urine evaluation, and ultrasonography. If you already completed a basic workup but still need the CT, make sure to attach the results of your workup to your request. Certain conditions require a CT right away, but most do not fall into that category.
Think twice when ordering two tests. For example, abdomen and pelvis studies seem to be ordered reflexively as a combination. However, you may only need one of those studies to evaluate a certain part of anatomy. If you need a triple-phase liver study, for example, just order the abdomen study. If you need an adrenal protocol study, that is also just the abdomen. If you are ordering a second test because you are reevaluating a pancreatic cyst, be sure to include the prior report so we can verify that the timeframe for interval surveillance is correct (we look at the date of the prior study and the size of the lesion).
Involve your staff. Sometimes, reviewers cannot tell from the visit notes if the study is approvable, and we request a call from your office. You do not need to be the one to make the phone call for the peer-to-peer discussion. You can have a member of your staff call to see if it is a documentation issue or something else they can help with, which saves you time. If we just need them to attach supporting documentation, you never need to be the one on the phone.
Make the justification clear. For example, if you suspect acute appendicitis or diverticulitis, be sure to document your clinical concerns and provide supporting documentation such as a fever or other key elements from your exam findings. If you are concerned about unintentional weight loss, provide the timeframe and percent weight loss in the documentation. If you are ordering a CT urogram for hematuria, be sure to include the rationale and a copy of the urine microscopy results (not just a dip-stick). Do you think your patient has kidney stones? Most of the time, you can find all the information you need with a urinalysis, ultrasound, or x-ray. But if your patient needs a CT for a kidney stone, please justify this in your notes (e.g., by documenting inconclusive results from prior studies). If your patient is about to have surgery or needs reassessment after a surgery, this needs to be in the notes as well. And if you’re seeking a prostate MRI for elevated PSA levels, document that there is a plan to biopsy or that the patient is under active surveillance for known prostate cancer.
COMMON EXAMPLES
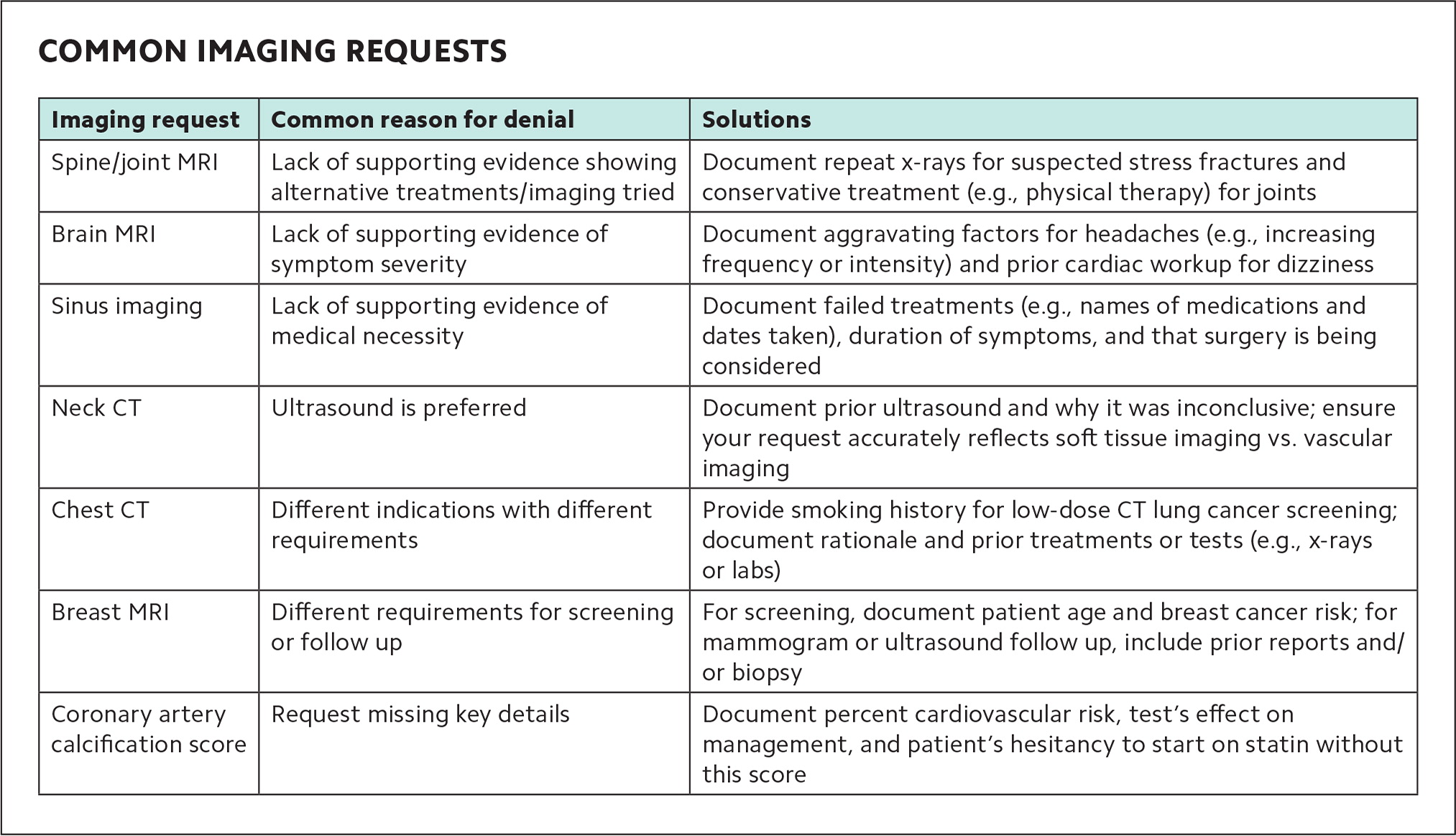
Here are some common prior authorization requests, reasons for denials, and ways to smooth the path to approval (see “Common imaging requests” for a summary).
| Imaging request | Common reason for denial | Solutions |
|---|---|---|
| Spine/joint MRI | Lack of supporting evidence showing alternative treatments/imaging tried | Document repeat x-rays for suspected stress fractures and conservative treatment (e.g., physical therapy) for joints |
| Brain MRI | Lack of supporting evidence of symptom severity | Document aggravating factors for headaches (e.g., increasing frequency or intensity) and prior cardiac workup for dizziness |
| Sinus imaging | Lack of supporting evidence of medical necessity | Document failed treatments (e.g., names of medications and dates taken), duration of symptoms, and that surgery is being considered |
| Neck CT | Ultrasound is preferred | Document prior ultrasound and why it was inconclusive; ensure your request accurately reflects soft tissue imaging vs. vascular imaging |
| Chest CT | Different indications with different requirements | Provide smoking history for low-dose CT lung cancer screening; document rationale and prior treatments or tests (e.g., x-rays or labs) |
| Breast MRI | Different requirements for screening or follow up | For screening, document patient age and breast cancer risk; for mammogram or ultrasound follow up, include prior reports and/or biopsy |
| Coronary artery calcification score | Request missing key details | Document percent cardiovascular risk, test’s effect on management, and patient’s hesitancy to start on statin without this score |
Spine and joint studies are commonly ordered in primary care, with an MRI typically being the study of choice. If you are concerned about a stress fracture, especially of the hip, be sure to document this and send your x-ray reports. Most stress fracture evaluations require a repeat x-ray 10–14 days after symptoms develop, because a stress reaction can be seen on plain films for joints that are not the hip. Most joint studies require a period of conservative treatment (e.g., physical therapy, a doctor-supervised home exercise program, or a chiropractic course). Certain conditions would justify bypassing this requirement, but you would have to document a positive finding on exam (for the spine, it would be a neurologic deficit; for the joint, it would be a joint-specific derangement). A physical therapy discharge summary can supply key details to ensure the right body region was treated, the treatment took place within the past six months, and a good-faith effort was made for at least 4–6 weeks (this can vary based on body region and insurance company). Abnormal electromyography studies showing radiculopathy can also help to justify your request for MRI. Be sure to send those reports as well.
Brain studies are often ordered for headaches, dizziness, and memory impairments. But MRIs are not routinely needed for headaches, so if you’re seeking prior authorization for that, document the compelling reasons such as increasing frequency or intensity, or neurological abnormalities on exam. For dizziness, there are many causes other than central pathology, so be sure to document that your concern is truly for a central cause. It’s often prudent to get a full cardiac workup to identify an etiology for a patient’s dizziness. If you’re ordering a study due to memory impairment, be sure to document your memory testing (e.g., Mini-Mental State Examination or Montreal Cognitive Assessment results showing impairment) and results of basic lab work that rules out reversible causes (e.g., vitamin B12, thyroid-stimulating hormone, complete blood count, and basic metabolic panel).
Sinus studies are commonly ordered, even for patients that do not meet medical necessity criteria. Imaging is usually only needed if the patient is considering surgery, and then documentation of failed treatments and duration is required. Include the names of the medications tried, the dates the patient took them, and whether your patient was compliant with treatment.
Neck studies are often ordered to assess masses or vascular issues. Ultrasounds are usually preferred for this because they can obtain high-quality images without radiation. Therefore, if you’re seeking a CT, be sure to include prior, recent ultrasound reports and explain why the results are inconclusive. Also, make sure your study wasn’t denied because you requested authorization for the incorrect type (e.g., neck CT for soft tissue vs. neck CT angiogram for vascular disease).
Chest CT studies are commonly ordered, but there are different indications and qualifying criteria. For instance, the low-dose CT screening test for lung cancer requires that you document the patient’s age, pack per year smoking history, lack of new respiratory symptoms, and smoking status. If reviewers cannot verify these criteria fall within the U.S. Preventive Services Task Force guidelines, they can’t approve the study. If you order chest imaging for a reason other than lung cancer screening, please document the rationale for it and any prior treatments or tests performed (such as a chest x-ray report, pulmonary function test results, or lab tests). Sometimes you will need a different test, such as chest CT angiography, if it is for a vascular problem (such as an embolism or aneurysm). This happens more often than you might think.
Breast MRI studies are being ordered more frequently. If you order an MRI for breast cancer screening, be sure to include the age of the patient and percentage lifetime risk for developing breast cancer. When you order it to follow up on abnormal mammogram or ultrasound imaging, be sure to include the prior reports and biopsy results (or an explanation for why a biopsy cannot be done).
Coronary artery calcification score is another common study that often leads to peer-to-peer calls. Some insurers consider this study investigational and simply won’t approve it. For the plans that do cover it, having a few key details in the note can help ensure your request is approved. Document the patient’s cardiovascular risk (e.g., 18%) and how this test would justify a change in management. If the patient is already on a statin, ordering this test just to see the disease burden would not be a compelling rationale. However, if the patient has an intermediate 10-year risk and is hesitant to start a statin without knowing the calcium score, then this test is justified. Make sure to put a statement about this in the note.
WORKING TOGETHER
A judicious approach to advanced imaging requests is the best way to avoid peer-to-peer calls. In general, only order tests that could change your management. A test is usually not justified if you are just “checking” on a chronic condition, and this often leads to denials and frustration. When your management hinges on an imaging study, document your clinical concerns and attach all supporting evidence to show medical necessity. When there is clear documentation of how the study will change management of the problem, it is usually easy for us to approve your test.
However, if your study does not get approved, do not hesitate to call and ask why — or have your staff reach out. Together, we can make it a brief and positive experience. The clinical reviewer will let you know what was missing and what you need to do to get the study approved. By approaching these calls with an open mind and a growth mindset, we can all move forward in this ever-changing and often-challenging medical landscape.
ADDITIONAL READING
A Guide to Relieving Administrative Burden: Prior Authorization [AAFP supplement] describes AAFP advocacy efforts and techniques, technologies, and transformations to help reduce prior authorization burden.
Simplification Push Yields Major Prior Authorization Win [AAFP News] and CMS Prior Authorization Final Rule Explained [AMA video] describe a January 2024 final rule from CMS that will bring automation and efficiency to the prior authorization process for certain goverment-regulated health plans, require them to provide specific reasons for denials and public reporting of approval and denial metrics, and shorten the time-frame for decisions.
