
Fam Pract Manag. 2024;31(4):4-6
The publication of this supplement is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.

A major priority for the American Academy of Family Physicians (AAFP) is to increase payment for family physicians, with much of our energy focused on primary care payment models and how they dictate the manner in which organizations are paid. Those organizations include independent, physician-owned single or multispecialty practices; large health care organizations (e.g., hospital-based health systems); medical insurance providers; and retail giants (e.g., Amazon, Walmart). While progress has been made to increase family physician payments while reducing physician burden, it has been at a relatively glacial pace.1 Even more frustrating, physician compensation is not commensurate with the progress made in value-based care payments to the health systems that employ those physicians.2 With most physicians working as employees,3 including more than 73% of AAFP members,4 this disconnect matters.
DATA-DELIVERED ADVOCACY
The AAFP advocates to improve family physician employment and compensation in many ways, two of which we bring to your attention in this Beyond the Beltway feature. First, in 2023, the AAFP adopted a new policy in its position paper, Principles to Optimize Family Physician Employment. In this paper, we outline the wide range of factors that organizations should consider if they wish to be an employer of choice for family physicians. Each of these main principles has sub-principles and recommended key practices employers can review to assess whether their culture, policies, and other practices improve professional satisfaction and help retain family physicians. The principles are also the basis for our 5 Signs of a Good Physician Employer.
Many factors, including compensation, can impact professional satisfaction. The AAFP Career Benchmark Dashboard, available at no cost to members, allows family physicians to benchmark compensation levels and see how fellow family physicians serving in similar and different roles and practice settings describe how their work is structured, along with their professional satisfaction and well-being. This depth of information is helpful for students, residents, and family physicians making crucial career decisions. For example, family physicians considering relocation can find information about geographic differences in compensation; residents determining which practice setting to pursue can compare differences between role types and practice settings; and medical students can explore family medicine to learn more about the specialty. The Career Benchmark Dashboard is an important step toward creating pay transparency and empowering family physicians with the information they need to navigate opportunities. The resource increases the understanding of family physicians' many vital roles and strengthens the family medicine pipeline.
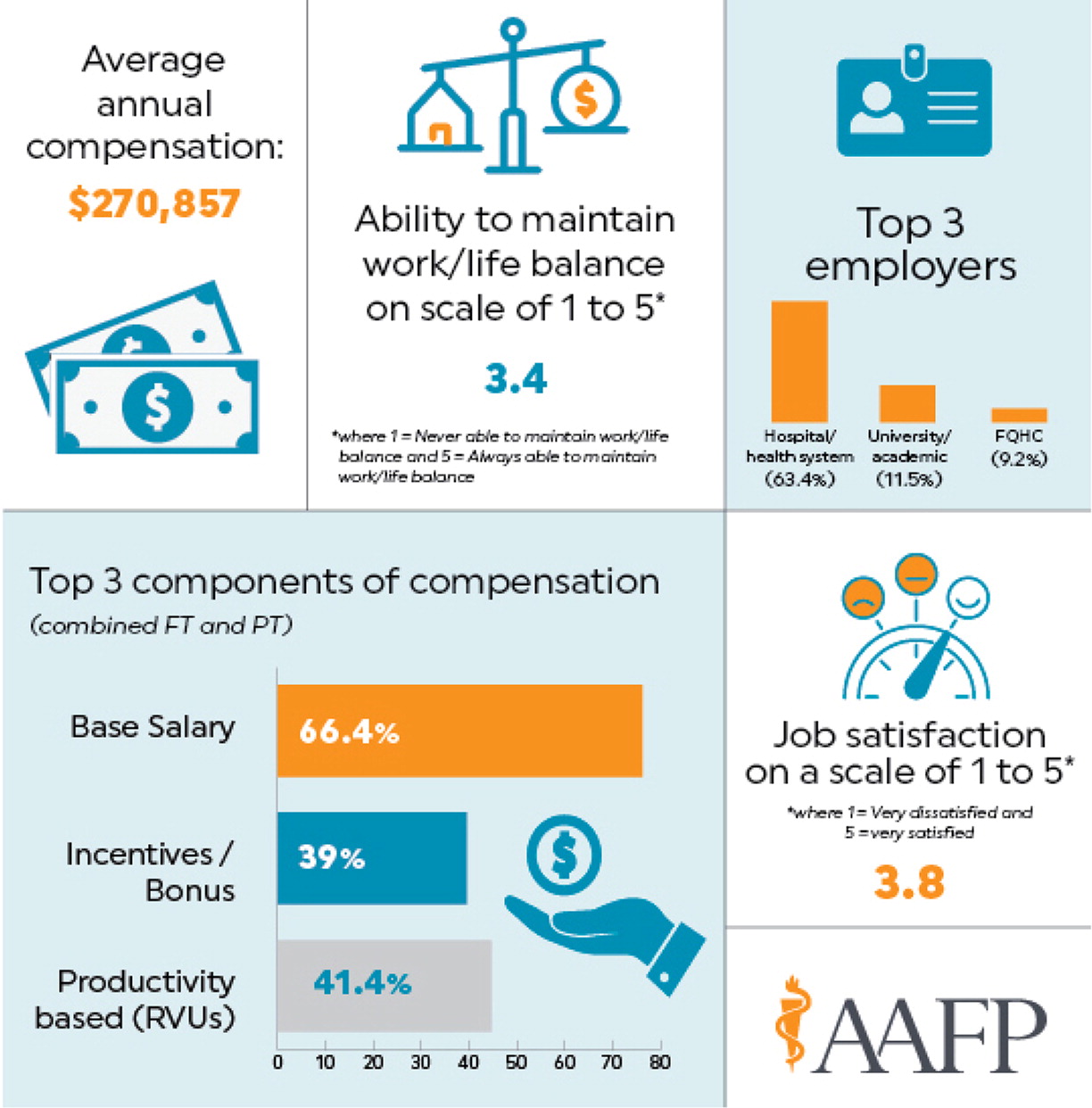
The interactive dashboard relies on data from a 2023 survey with 7,500 family physician responses and provides a high-level view of averages from the entire sample. The “Explore” links in the dashboard are located directly above the figures and charts for the six categories (i.e., total responses, average compensation, satisfaction, work information, roles, and secondary source of income) and provide a breadth of information users can filter by various demographics and work situations. The filters allow users to better understand the family physician market for compensation and other aspects of employment and drill down to assess factors relevant to their circumstances or different career paths. For example, users can filter such information as full- or part-time status, with 83% of family physician respondents in 2022 reporting that they practice full-time, with an average annual salary of $274,359.5 The average part-time compensation was $185,943 for physicians reporting as less than full-time, regardless of hours worked.
The customizable, in-depth view allows family physicians, students, and residents to explore the factors most important when making career decisions. Additional information in the dashboard includes the amount of paid time off and funding for continuing medical education (CME). The compensation section shows salary distribution, compensation structure, benefits, and bonuses. The job satisfaction section compares overall satisfaction, work-life balance, level of autonomy, and level of burnout across a variety of roles, clinical settings, or employer types. Limiting filters within a category or increasing the number of filter categories is the best way to ensure there are more than 11 responses and data is displayed.
EMERGING ISSUE: PRIMARY CARE AS AN INVESTMENT STRATEGY
Primary care has attracted significant attention and investment from large health care-related businesses (e.g., CVS, Walgreens, Aetna, United Healthcare), retail giants (e.g., Amazon, Walmart), and private equity firms. For many of these companies and firms, the alignment of primary care with their business strategy is relatively straightforward. For others, such as Amazon and Walmart, the reason for their investment in primary care may be less obvious. Warning signs have been flashing recently as a number of these businesses announce shifts in their primary care participation. Walmart recently announced the closure of all 51 of its health centers across five states, in addition to closing its virtual care services.6 With its massive success as a retailer, particularly in rural communities, Walmart's entry into primary care was perceived as a potential solution to many communities' lack of primary care access. Their decision to discontinue their primary care services has raised concerns about access in those communities.7,8
So, what is the market telling us if a massively successful corporation like Walmart fails to make primary care work? One apparent answer is that primary care business models (i.e., approaches to reimbursement and payment) that rely solely on an undervalued and administratively burdensome fee-for-service payment are unsustainable.9 We know there are countless examples of primary care working well, either because companies are benefitting and profitable from well-designed and implemented primary care payment models or due to the creativity, tenacity, and passion of dedicated family physicians. The latter approach is not a long-term, sustainable model due to our enormous primary care workforce challenges.10 While solutions may not always be clear, the AAFP will continue to advocate for our members using the best data available to increase your compensation, reduce your burden, and improve your professional satisfaction in all settings and all ways.
