
Fam Pract Manag. 2024;31(4):19-21
The publication of this supplement is funded by the Centers for Disease Control and Prevention (CDC) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $603,907, with 100 percent funding by the CDC/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, or an endorsement by, the CDC/HHS or the U.S. government. This supplement is brought to you by the AAFP. Journal editors were not involved in the development of this content.
Introduction
Marijuana is the most commonly used drug of abuse during pregnancy in the United States,1 with self-reported use ranging from 2–5% for all women and 15–28% among women who are young, urban, and socioeconomically disadvantaged.2 Many patients use it for its nausea-relieving properties during pregnancy and believe it is relatively safe since it is natural.
The reality is the more than 500 chemicals found in marijuana — including the mind-altering compound delta-9-tetrahydrocannabinol (THC) — can pass through a woman's placenta to the developing fetus during pregnancy and to a baby through breast milk, affecting the growing infant.1 While data is limited and often confounded by other substance use, research indicates a significant risk of cannabis use in pregnancy.3 Reviews show infants born to women who used marijuana during pregnancy were more likely to require neonatal intensive care unit admission, had lower birth weights,4 higher stillbirth rates, and lower Apgar scores (i.e., a test after birth to determine how well the baby tolerated the birthing process).5
Analyses of longitudinal studies show associations between prenatal marijuana exposure and developmental effects on adolescents, including decreased performance on memory, impulse control, problem-solving, quantitative reasoning, verbal development, and visual analysis tests.6 Many effects persist into young adulthood and appear to have a dose-dependent relationship.7
This educational supplement describes different cannabis products, their effects, practice guidelines and recommendations, and screening tools to identify patients who are using cannabis during pregnancy and while breastfeeding.
The WEED mnemonic below is a good starting point to consider when discussing cannabis use with patients who are pregnant or breastfeeding.
WEED: Practice Mnemonic for Addressing Cannabis Use in Pregnancy13
Welcome questions about cannabis use
Explore alternatives to cannabis for common pregnancy ailments, such as anxiety and nausea
Explain the potential risks of cannabis use
Deliver a harm-reduction message by recommending a decrease in the dose and frequency for patients who are not able or willing to remain abstinent during pregnancy
Cannabis Products and Duration of Effects
Marijuana consists of dried leaves, flowers, stems, and seeds derived from either the Cannabis sativa or Cannabis indica plants.8 It can be processed into a number of different forms, which can be consumed orally (i.e., edibles, capsules/tablets, tinctures, lozenges/films), inhaled (i.e., pre-rolls, pipes/bongs, concentrates, vapes [dried flower or concentrates]), or applied to the skin (i.e., topicals).9
The time to onset and duration of the effects may vary depending on how cannabis is consumed. Inhalation produces the fastest onset of effects, from seconds to a few minutes of inhalation, and the effects can last up to six hours. Ingestion produces the slowest onset of effects from 30 minutes to two hours of ingestion but a longer duration, with the effects lasting up to 12 hours after use.10
Cannabis Effects
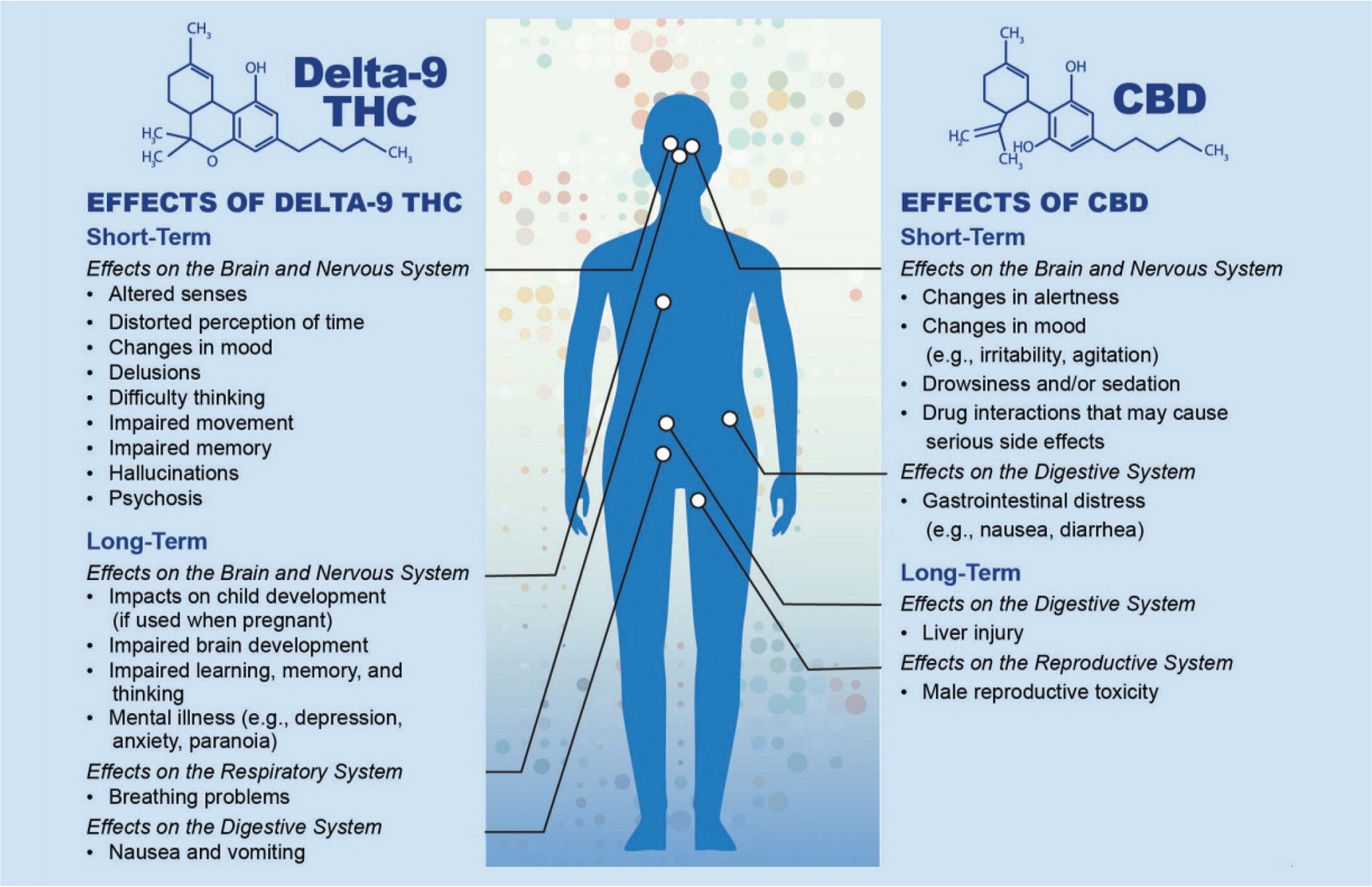
Of the more than 500 chemical compounds found in the cannabis plant, more than 100 are cannabinoids (i.e., chemical compounds that produce a range of physical and mental effects).11 Figure 1 below describes the potential health effects of the two most common cannabinoids: delta-9-THC and cannabidiol (CBD).
Guidelines and Recommendations
The U.S. Preventive Services Task Force (USPSTF) recommends screening all adults for unhealthy drug use when appropriate diagnosis, treatment, and care can be offered or referred.12
However, the American Academy of Family Physicians (AAFP) “concludes that the evidence is insufficient to assess the benefits and harms for screening adolescents and adults for unhealthy drug use. This statement does not include screening for opioid use disorder.”14 The Academy believes it is important to discuss the developmental and negative impacts of marijuana on children, adolescents, and individuals who can become pregnant.15
The American College of Obstetricians and Gynecologists (ACOG) recommends asking patients before and early during pregnancy about cannabis use, as well as alcohol, tobacco, and other substance use.2 They also recommend that patients using cannabis should be counseled about the potential adverse health effects of continued cannabis use during pregnancy and while breastfeeding, discourage cannabis use during pregnancy and lactation, and encourage alternative therapies that have better pregnancy-specific safety data.
Screening for Cannabis Use
Screening and brief intervention (SBI) is an evidence-based approach for early intervention and treatment for unhealthy substance use, including cannabis.16 Early intervention and screening can raise patient awareness of behavior patterns, inform patients about the risks of substances, and reduce their use and harm. SBI should be a part of standard lifestyle screening that includes questions about diet, exercise, and sleep.
The validated screening options in the box below can be used to fit the type of patient encounter, time constraints, and patient needs. Screening is an excellent way to begin the conversation and determine if further questions or interventions are necessary.
The National Institute on Drug Abuse (NIDA) question asks about illegal drug use or using a prescription medication for non-medical reasons. Given that cannabis is now legal in many states, the term illegal in the question may be confusing, so using the word ‘cannabis' could be substituted for ‘illegal drug.'
Key Takeaways
There is no known safe amount of cannabis use during pregnancy.1
The effects of cannabis use on overall health and pregnancy are not fully understood, and there are many untested claims of health benefits, including for treating nausea and vomiting in pregnancy.7
Significant effects on the endocannabinoid system suggest cannabis and CBD could pose serious risks to the developing brain, and active components of cannabis can cross the placenta and be found in breast milk.1
More research is needed to fully understand the effects of cannabis use during pregnancy.17 Given this lack of understanding, the ACOG recommends discouraging the prescription or suggestion of cannabis use during preconception, pregnancy, and lactation.2
Studies have established that cannabis use is often concurrent with tobacco, alcohol, or other substance use, which are all known to affect pregnancy and lifelong outcomes and should all be addressed by the primary care physician and other providers.7
The American Society of Addiction Medicine (ASAM) supports reforms to reverse punitive approaches to substance use during and after pregnancy, as they are not evidence-based and disproportionately affect people of color.18 Furthermore, treatment services are limited for people who are pregnant, and those who do not receive treatment should not be assumed to have rejected treatment.
