
Fam Pract Manag. 2024;31(4):33-38
The publication of this supplement is supported by a cooperative agreement (6 NU66IP000681-02-01) with the Centers for Disease Control and Prevention (CDC), U.S. Department of Health and Human Services. This supplement is brought to you by the AAFP. Journal editors were not involved in the development of this content.
Introduction
In August 2020, the American Academy of Family Physicians (AAFP) was awarded a five-year cooperative agreement by the Centers for Disease Control and Prevention (CDC). The agreement's core focus was the improvement of adult immunization rates among racial and ethnic minority populations. The AAFP implemented Improving Adult Immunization Rates Among Racial and Ethnic Minority Populations, a project to develop effective strategies, tools and resources to increase and improve vaccination rates among adults from racial and ethnic minority groups. The project used the team-based Office Champions Quality Improvement Model, which employed Plan-Do-Study-Act (PDSA) cycles to implement interventions to improve immunization rates, assess the effectiveness of the interventions and make adjustments to meet quality benchmarks.
The AAFP selected 22 family medicine practices to participate in this project. These practices used a team-led approach and incorporated interventions, strategies and resources into their daily workflow to guide their care teams' efforts to improve adult immunization rates for racial and ethnic minority patients.
In this supplement, five high-performing family medicine practices that participated in Improving Adult Immunization Rates Among Racial and Ethnic Minority Populations describe how they increased adult vaccination rates among their patients from racial and ethnic minority groups by implementing targeted quality improvement and practice improvement (QI/PI) initiatives, incorporating best practices and applying lessons learned.
Their outcomes show that the continuity of care provided by physicians and other health care team members within family medicine practices makes them ideally suited to address the many challenges and barriers impacting adult vaccination rates, especially among historically marginalized populations and populations that are underserved by the health care system.
Northwestern McGaw Family Medicine Residency
Authors: Adiba Khan, MD; Joyce Jones-King, MD; and Ashley Watson, MD
Located in Lake County, Illinois, Northwestern McGaw Family Medicine Residency at Lake Forest is a practice with five attending physicians and 24 resident physicians. We serve a diverse population of patients of all ages.
QI/PI INITIATIVES
Our primary goal was to increase vaccination rates among our African American patient population. We aimed to achieve 65% vaccination rates for influenza and human papillomavirus (HPV), a 60% recombinant zoster vaccination rate and a 70% pneumococcal vaccination rate among eligible African American patients.
To achieve our goals, we established two intervention arms: residency education and clinical process improvement. For residency education, we developed a two-part curriculum that included the following:
Vaccine counseling: The first part of the curriculum focused on topics including the basic science of vaccines, vaccine-preventable diseases, and vaccine recommendations, schedules, safety, efficacy and administration.
Addressing vaccine hesitancy: The second part of the curriculum reviewed the origins of medical mistrust among people in the African American community. It also focused on increasing clinician confidence in addressing vaccine hesitancy through patient-centered conversations that incorporate specific motivational interviewing techniques.
Our clinical process improvement interventions were multifold. We engaged clinic staff at every step to create a comprehensive intervention plan. During the rooming process, medical assistants were empowered to ask patients about indicated vaccines and place standing orders if a patient agreed to be vaccinated. Culturally sensitive patient education materials about vaccination were placed in all examination rooms. Clinicians were encouraged to use the knowledge they acquired during educational sessions and strongly recommend vaccines at every visit. Attending preceptors reviewed vaccine gaps with residents to further reduce missed opportunities for immunization. In addition, to address the inherent challenges of maintaining continuity in a residency practice, we created a process to standardize documentation regarding vaccine refusal or delay so that other clinicians could continue conversations about indicated vaccines with patients as appropriate.
PRACTICE RESULTS
Vaccine administration rates for eligible African American adults increased across three measurement periods, demonstrating the positive impact of our practice's efforts to improve vaccine uptake in this patient population (Figure 1).

SUCCESSES AND BARRIERS
Our successes were largely attributable to increased awareness of vaccination rates within our practice. We provided data regarding vaccines to our staff and clinicians and created shared goals for improvement. Our two-part vaccine curriculum was well received by resident physicians, who reported increased confidence in having difficult conversations with patients. Clinical process improvements were clearly outlined and easy to implement, and we regularly evaluated their ease of integration.
Many of the barriers we faced were related to the COVID-19 pandemic. For example, when our practice limited well visits so we could accommodate sick visits, opportunities to identify and address gaps in preventive vaccinations were also limited. The increase in tele-visits reduced these opportunities even more. In addition, once our clinic started offering the COVID-19 vaccine series and subsequent boosters, clinicians focused their efforts on addressing hesitancy specifically related to the unique concerns surrounding these vaccines. It was also challenging to use our electronic health record (EHR) to break down immunization rates by clinician and by patient race/ethnicity. Using a randomly selected patient sample as part of this QI/PI project simplified our analysis.
SUSTAINABILITY
We created an annual Addressing Vaccine Hesitancy Day to review our practice's vaccination rates and implement our educational curriculum. It is held in early fall to coincide with the beginning of flu season. We hope that this yearly event will reinvigorate clinicians and staff and increase the sustainability of our efforts.
The University of Kansas Health System
Authors: Michelle Sommer, MD; Joel Hake, MD; and Melodie Jones-Loo
Situated on the border of Kansas City, Kansas, and Kansas City, Missouri, University of Kansas Family Medicine and Community Health provides full-spectrum care and serves a diverse patient population.
QI/PI INITIATIVES
Our clinic's initiatives were made possible by our staff's efforts and the support of The University of Kansas Health System. Our clinic uses the health system's EHR and its patient portal, which allows patients to see preventive care recommendations and their overdue vaccinations.
For our first QI/PI initiative, we provided education about the immunization rate improvement project during our pre-clinic team huddle. On the team huddle message board, we posted a daily reminder to check the vaccination status of each patient. This initiative coincided with the health system's implementation of a new automated patient messaging system that sent patients health maintenance reminders, including information about their vaccine needs.
Our next intervention involved conducting formalized in-service education for nurses and clinical staff about certain vaccinations, including information about patient eligibility, timing and administration practices. During this project phase, we also placed vouchers for the recombinant zoster vaccine in all patient rooms. For patients whose vaccines are only covered through pharmacy benefits, these vouchers still served as a physical reminder to get vaccinated.
Our most recent intervention has been using a previsit planning strategy. A team of nurses reviews future patient appointments to look for health maintenance deficiencies, including vaccine gaps, and places pended orders to address any identified deficiencies. Our clinicians can then easily visualize a patient's deficiencies, review them with the patient during the office visit and complete the pended orders if appropriate.
PRACTICE RESULTS
Our interventions primarily targeted the two vaccines with the lowest vaccination rates in our clinic: recombinant zoster and HPV. We successfully increased our shingles and HPV vaccination rates by 2% and 20% above our baseline, respectively. Our pneumococcal vaccination rate did not need to be improved because it started at 100%. Our COVID-19 and influenza vaccination rates declined from baseline, which aligns with a national trend.1
SUSTAINABILITY
Sustaining improved vaccination rates requires a multifaceted approach that addresses various aspects of health care delivery in our clinic. We plan to use targeted education and outreach to continuously educate clinicians, nursing staff, patients and caregivers about the importance of immunization. We also plan to continue disseminating vaccine-related information through diverse communication channels, including our patient portal and automated patient messaging system.
In addition, our health system has invested in information systems to track vaccine administration and alert clinicians and staff about vaccines that are due. We will provide ongoing training to ensure that clinicians and staff are up to date with the latest immunization guidelines, techniques and safety protocols. We have trained staff on pre-visit planning that includes calling patients before visits to discuss their health care needs. By implementing these strategies in a coordinated manner, stakeholders can work together to sustain improvements and further improve immunization practices.
The Stevenson Family Health Center
Author: Eugene Schiff, MD, MPH, AAHIVS
Located in the Soundview neighborhood of the Bronx in New York, the Stevenson Family Health Center is a federally qualified health center (FQHC) run by the not-for-profit Institute for Family Health. Approximately 1.4 million people live in the Bronx, and 57% of residents identify as Hispanic, 28% identify as Black, 8% identify as white and 4% identify as Asian.2 It is one of the poorest counties in New York state.3,4 Our practice serves more than 10,000 patients of all ages who are mostly immigrants and people of color.
QI/PI INITIATIVES
Front desk staff, medical assistants, care navigators, nurses, physicians and clinic and organizational leaders were all involved in the Improving Adult Immunization Rates Among Racial and Ethnic Minority Populations project. Our QI/PI initiatives included using recall and reminder systems, stocking various vaccines on a more timely basis and requesting optimization of clinical decision support. We recommended vaccination at each patient visit. We also presented vaccine coverage data broken down by race/ethnicity at various all-staff meetings and organization-wide leadership meetings.
PRACTICE RESULTS
Our practice's immunization rates for patients from racial and ethnic minority groups showed improvements over three measurement periods for the following vaccines:
Influenza: 10% increase over baseline
COVID-19: 2% increase over baseline
Recombinant zoster: 266% increase over baseline
○ Period 1: 0 patients vaccinated
○ Period 2: 3 patients vaccinated
○ Period 3: 11 patients vaccinated
Pneumococcal: increase from 37% coverage to 100% coverage
Tetanus and diphtheria toxoid/tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Td/Tdap): increase to 92% coverage
Over the third measurement period, the rate of HPV vaccination decreased by 17%.
A simultaneous initiative that focused on random chart reviews for African American patients showed the following results:
Improvements in rates of influenza vaccination (30% increase) and HPV vaccination (84% increase)
High rates of pneumococcal vaccination (100%) and Td/Tdap vaccination (85%)
Decreasing rates of COVID-19 vaccination (26% decrease)
SUCCESSES AND BARRIERS
In response to challenges related to purchasing the recombinant zoster vaccine and stocking it directly in the clinic, we partnered with an on-site pharmacy to access it. We were successful in maintaining high pneumococcal vaccination rates when we introduced the pneumococcal 20-valent conjugate vaccine (PCV20) in 2023. Making the COVID-19 vaccine available to our patients and having standing orders for the administration of COVID-19 and influenza vaccines helped us increase coverage.
Since our practice only had the Moderna COVID-19 vaccine, some patients preferred to seek the Pfizer vaccine elsewhere. Decreases in the COVID-19 vaccination rate among our adult African American patients may be attributed to the following factors:
Elimination of citywide COVID-19 vaccine mandates in our area
Vaccine fatigue
Limited perception of individual risk
Lack of understanding of vaccine efficacy
Concern about vaccine side effects
Misinformation
Lack of standard EHR clinical decision support for COVID-19 vaccines
Frequently changing COVID-19 vaccine recommendations from the CDC and the Food and Drug Administration (FDA)
We had difficulty using recall/reminder systems to contact large numbers of patients regarding influenza and COVID-19 vaccines. We also faced challenges with real-world standing order implementation for these vaccines. This was partly due to limited information technology (IT) resources, limited appointment availability, nursing staff shortages and challenges in hiring nurses. Although competing priorities made it difficult to achieve and maintain all-staff participation in vaccination efforts, the multiyear design of this project helped support continuity.
SUSTAINABILITY
In the future, we hope to use automated recall/reminder systems for vaccinations, improve clinical decision support and implement a “Vaccines as a Vital Sign” campaign for adults and children across our organization. Reviewing baseline racial and ethnic disparities in vaccination rates and the results of this project with leadership and all staff will help us identify and target efforts for future improvements.
MetroHealth
Authors: Antoinette Abou-Haidar, MD, and Hemalatha Senthilkumar, MD
Located in Cleveland, Ohio, MetroHealth is a Cuyahoga County public safety-net hospital system. MetroHealth strives to reduce health disparities among racial and ethnic minority populations that have historically been disadvantaged by facing more barriers to health care, including inequitable access. Our practice, the Ohio City Health Center, is situated within the Urban Community School's campus and is committed to building a healthier, stronger community. Many of our clinicians are bilingual to meet the needs of our Spanish-speaking patients.
QI/PI INITIATIVES
Our QI/PI project involved six vaccines — influenza, COVID-19, Tdap, HPV, recombinant zoster and pneumococcal — and was disseminated to the entire clinic. Our nurse manager ensured all of the vaccines were ordered and available. Vaccine champions were trained to make a strong recommendation to patients during check-in. Patients who were due for vaccinations were sent a reminder via text, letter or patient portal message. Informatic services generated a monthly progress report. Our on-site pharmacy was an additional resource to help us improve our vaccination rates. Due to our practice's low rate of HPV vaccination compared with the state average, we conducted a multidisciplinary project focused on increasing this rate.
PRACTICE RESULTS
Our practice's immunization intervention led to an increase in vaccine administration rates for influenza, COVID-19, HPV and recombinant zoster vaccines over one year (Figure 2). Our rate of pneumococcal vaccination decreased compared to baseline.
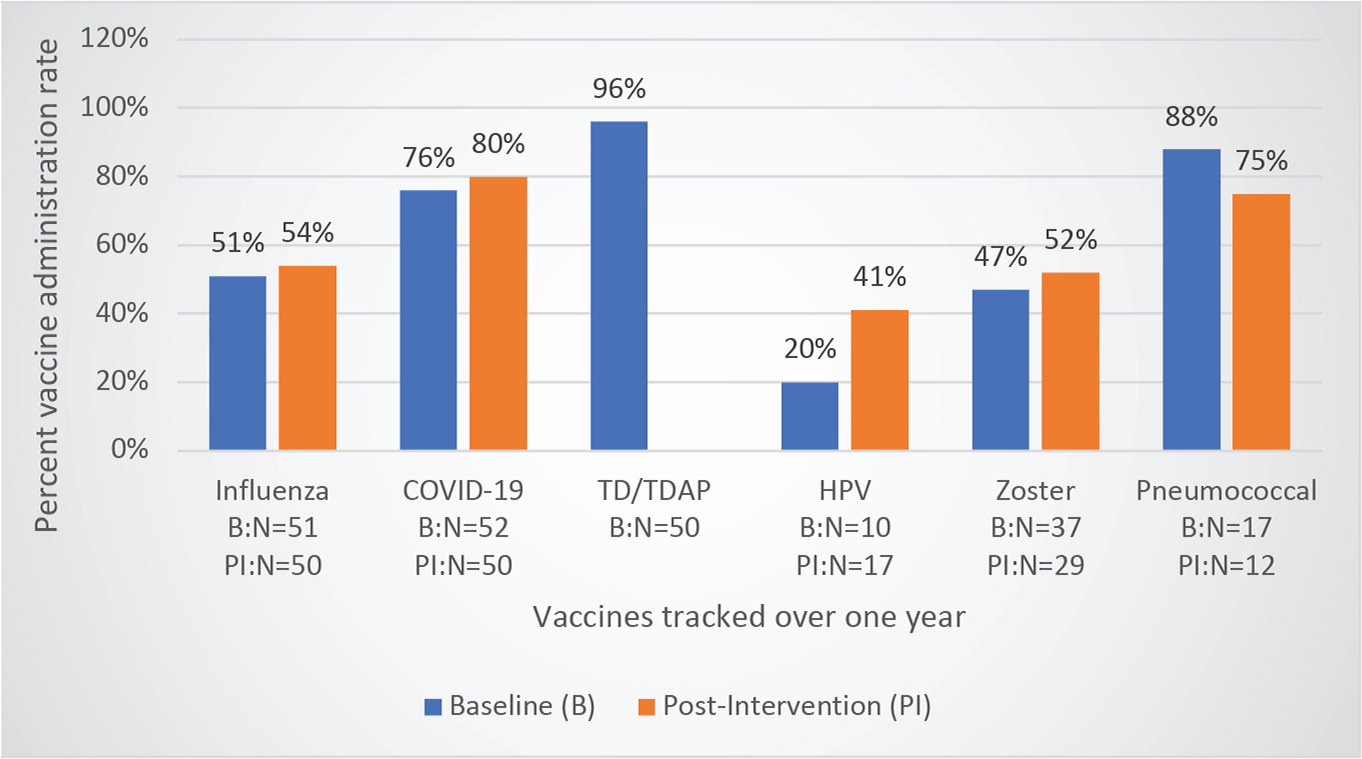
SUCCESSES AND BARRIERS
Our success stemmed from using a consistent approach and employing the CDC's strategic framework to do the following:
Identify undervaccinated communities
Use open conversations to empower families in their decision to vaccinate
Address myths and misinformation
Our strategies included using reminders in the EHR and developing office procedures to reduce missed opportunities. We also communicated the benefits of each vaccine to patients and recommended getting needed vaccinations “on the same day in the same way.” Because a patient may change their mind once they have a better understanding of the benefits of vaccination, it was essential to elicit and address our patients' concerns about vaccines and give them access to resources for additional information. If a patient declined vaccination, we followed the recommendation to conclude the visit by saying we would have another conversation about vaccines with them at their next visit.
We encountered the following barriers to vaccination:
Patient-related factors such as misinformation, language barriers, low literacy levels and lack of awareness
Parental hesitancy related to the number of vaccines given at one time, long-term side effects or other concerns
Clinician-related factors such as varying ability to give a confident recommendation to vaccinate, lack of time to discuss patient concerns, limited staff resources, limited vaccine availability and lack of access to our state's immunization registries
SUSTAINABILITY
We plan to continue positive trends by making a strong recommendation for vaccination at every office visit, addressing patients' concerns, dispelling vaccine myths, empowering medical assistants to offer vaccines at check-in and designating a dedicated vaccine champion to serve as a role model within the practice.
Summa Health
Authors: Evan Howe, MD, and Michelle Bender, BSN, RN, AMB-BC
The Family Medicine Center in Akron, Ohio, was accepted to be part of the AAFP's Improving Adult Immunization Rates Among Racial and Ethnic Minority Populations project in 2021. As a primary care residency program, we already had some fundamental immunization practices in place to engage our population of patients who have been made vulnerable. For example, we have an opt-out policy for the influenza vaccine. During flu season, we actively offer the influenza vaccine to patients, engaging them at the first point of contact so we can get them vaccinated. This approach has been very successful and has kept our influenza vaccination rates above the national average. Participating in an initiative to improve adult immunization rates among racial and ethnic minority populations seemed like a natural way for us to continue building on our existing foundation.
QI/PI INITIATIVES
Our first step in this initiative was getting our residents and clinical team engaged. During the first measurement period, we tried to develop and adopt a dot phrase, or smart phrase, for use in our patient notes. During a visit, the clinician would enter the dot phrase and have a conversation with the patient about appropriate vaccine options. This gave clinicians an easy way to document the patient's response to their vaccination recommendation in a discrete field. Once an order was placed, staff would administer the specified vaccine(s).
During the second measurement period, we encountered some barriers. The COVID-19 pandemic was ongoing. Like most practices, we experienced considerable staff turnover and staffing gaps, so keeping up with training needs was a challenge. In addition, our patients were much sicker when they came into the office. We had fewer opportunities to discuss preventive care, and these conversations were not a priority in many cases.
Our metrics did not change much during the second measurement period, so we had to rethink our strategy. Because staff engagement was key to the success of our opt-out policy for the influenza vaccine, we decided to engage our staff more in the QI/PI initiatives for this project. Our next steps will include asking clinic staff to review vaccines due and best practice advisory notifications when they enter the examination room. Once a patient has been guided into the examination room, staff will offer any needed vaccines. If the patient agrees to be vaccinated, our registered nurses (RNs) can pend vaccines and ask the physician to sign off on them. Once the physician signs off, staff will get the vaccines ready to administer prior to the care visit. Administering vaccines before patients meet with a physician will prevent delays on the back end and allow for additional preventive services to be completed.
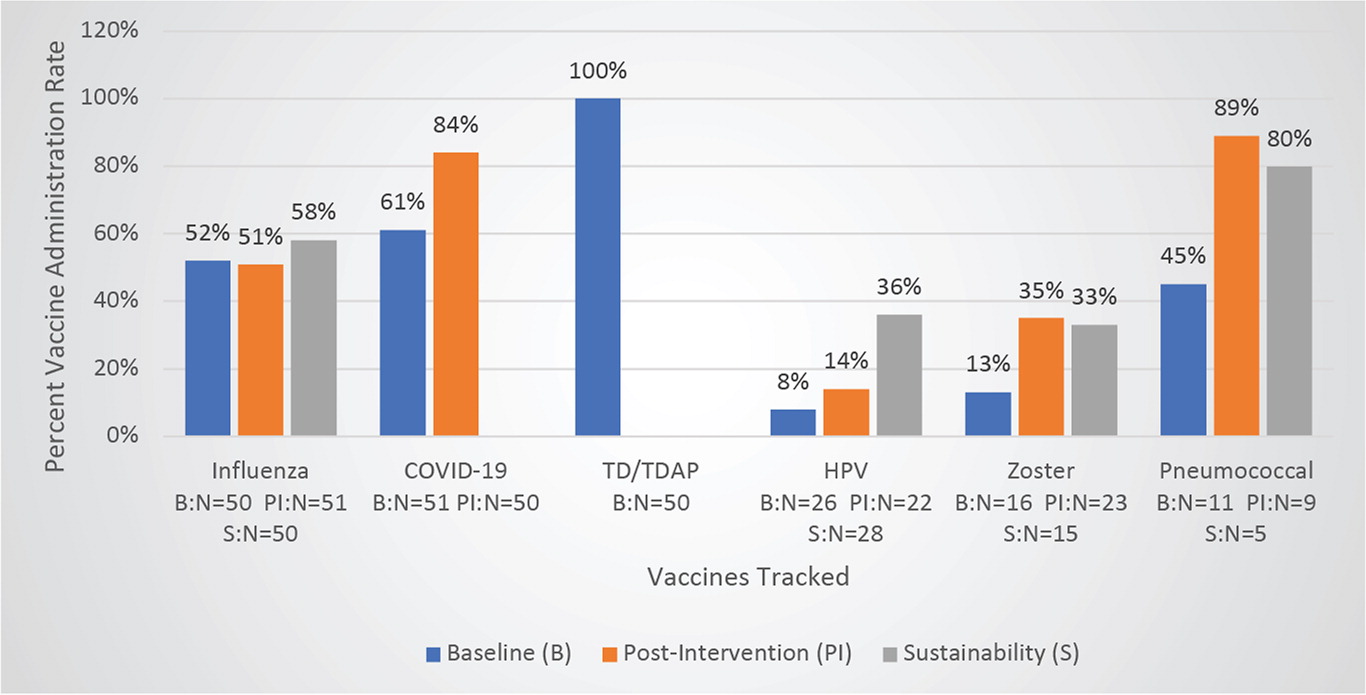
PRACTICE RESULTS
Figure 3 shows the impact of our practice's QI/PI initiatives on vaccine administration rates.
SUCCESSES AND BARRIERS
During the third measurement period, The Family Medicine Center highlighted the Td/Tdap and pneumococcal vaccines. Staff and clinicians focused on opportunities to review all vaccines due and educate patients about vaccines and their health.
At the end of 2022 and into 2023, our health system transitioned to a foundational EHR that was our own version. This made it more challenging to retrieve metrics during the measurement period. However, in spite of facing this additional barrier, we saw successful outcomes from our initiatives. We are proud of our small successes and will continue to build upon them by following best practices for preventive patient care.
