
Fam Pract Manag. 2024;31(5):5-7
The publication of this supplement is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.

In our ongoing Beyond the Beltway series, we have described the many ways and places the American Academy of Family Physicians advocates for increased investment in primary care through well-designed payment models. The AAFP has long believed that the current approach to primary care payment – the complex, burdensome and undervalued fee-for-service payments – must change. To sustain and improve our specialty, it is critical that primary care moves away from the current FFS approach and towards well-designed payment systems aligned with the AAFP Guiding Principles for Value-based Payment.
The AAFP has developed six call-to-action briefs to translate our guiding principles into actionable steps key stakeholders can implement to sustainably support family physicians and their care teams. The briefs are linked at the bottom of the guiding principles webpage to include a background of value-based payment models, along with individual briefs describing in detail the principles of establishing accountability, risk adjustment, financial benchmarking, performance measurement and information sharing in primary care payment.
OPTIMIZING AND SCALING PRIMARY CARE PAYMENT
While sharing these principles is just one way the Academy influences the conversation, transforming primary care payment will require meaningful action from a broad and diverse set of stakeholders within and beyond the Beltway of Washington, D.C. That transformation has been slow, but successful innovation has been occurring for more than a decade.1–4 Primary care is now at a critical juncture, and efforts must shift to optimizing and scaling successful innovations by influencing key decision-makers and stakeholders to adopt well-designed primary care payment models more broadly.
One significant stakeholder is the Center for Medicare and Medicaid Innovation (also called the CMS Innovation Center). CMMI was created by the Affordable Care Act in 2010 to test new payment and care delivery models that could improve care quality and efficiency for Medicare, Medicaid and Children's Health Insurance Program beneficiaries. The AAFP has advocated with CMMI since its inception, and the Innovation Center's development of payment models has fostered relationships among public and private payers that can accelerate the optimizing and scaling of successful payment models across the Medicare and Medicaid programs, impacting millions of patients.
The AAFP also advocates and engages with private payers to drive participation in muti-payer opportunities, which theoretically lessens the burden on practices. We're also working with state chapters to achieve meaningful payment changes at the regional and state levels. Lastly, we aim to inform you, our members, about opportunities to improve primary care payment – whether you're a practice owner or an employed physician.
RECENT PRIMARY CARE INNOVATIONS FROM CMMI
In October 2021, the Centers for Medicare & Medicaid Services announced a refreshed strategic direction for the Innovation Center, focusing on five objectives to execute CMS' vision – driving accountable care, advancing health equity, supporting care innovations, addressing affordability and partnering to achieve system transformation.5 The following three dimensions are central to meeting this vision for primary care6:
Transitioning primary care payments away from FFS to a prospective approach to support team-based, coordinated care
Focusing on health equity through increased safety net provider participation, adjusting payments for underserved areas and requiring health equity plans from participants
Requiring multi-payer alignment, including Medicaid, when possible, and scaling successful model features to other payers to ensure care delivery and payment changes that are tested are sustainable
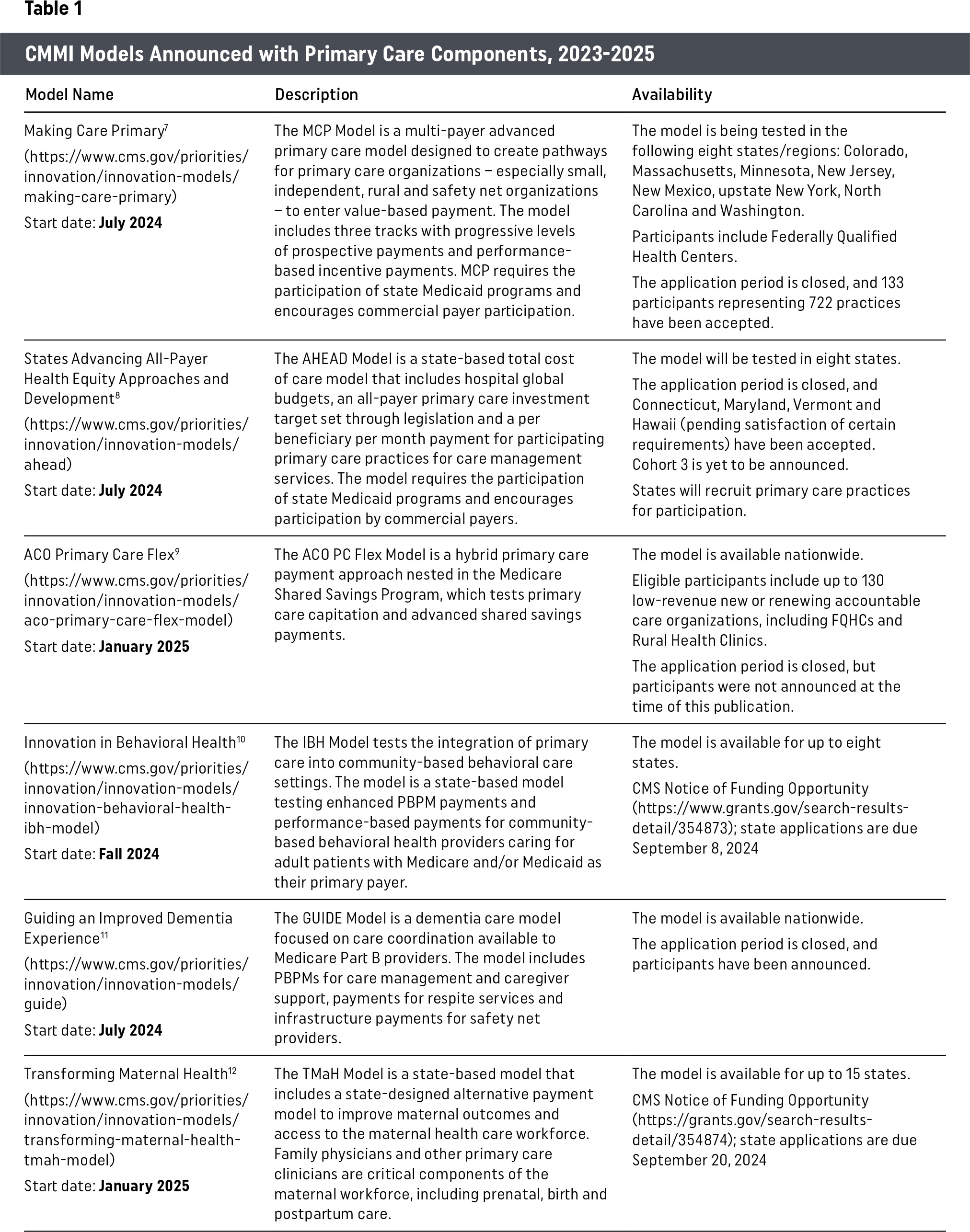
Several models have emerged from the Innovation Center in the past 18 months to transform primary care payment. Table 1 describes these models, which are directionally well-aligned with the AAFP Guiding Principles for Value-based Payment.
| Model Name | Description | Availability |
|---|---|---|
| Making Care Primary7 (https://www.cms.gov/priorities/innovation/innovation-models/making-care-primary) Start date: July 2024 | The MCP Model is a multi-payer advanced primary care model designed to create pathways for primary care organizations – especially small, independent, rural and safety net organizations – to enter value-based payment. The model includes three tracks with progressive levels of prospective payments and performance-based incentive payments. MCP requires the participation of state Medicaid programs and encourages commercial payer participation. | The model is being tested in the following eight states/regions: Colorado, Massachusetts, Minnesota, New Jersey, New Mexico, upstate New York, North Carolina and Washington. Participants include Federally Qualified Health Centers. The application period is closed, and 133 participants representing 722 practices have been accepted. |
| States Advancing All-Payer Health Equity Approaches and Development8 (https://www.cms.gov/priorities/innovation/innovation-models/ahead) Start date: July 2024 | The AHEAD Model is a state-based total cost of care model that includes hospital global budgets, an all-payer primary care investment target set through legislation and a per beneficiary per month payment for participating primary care practices for care management services. The model requires the participation of state Medicaid programs and encourages participation by commercial payers. | The model will be tested in eight states. The application period is closed, and Connecticut, Maryland, Vermont and Hawaii (pending satisfaction of certain requirements) have been accepted. Cohort 3 is yet to be announced. States will recruit primary care practices for participation. |
| ACO Primary Care Flex9 (https://www.cms.gov/priorities/innovation/innovation-models/aco-primary-care-flex-model) Start date: January 2025 | The ACO PC Flex Model is a hybrid primary care payment approach nested in the Medicare Shared Savings Program, which tests primary care capitation and advanced shared savings payments. | The model is available nationwide. Eligible participants include up to 130 low-revenue new or renewing accountable care organizations, including FQHCs and Rural Health Clinics. The application period is closed, but participants were not announced at the time of this publication. |
| Innovation in Behavioral Health10 (https://www.cms.gov/priorities/innovation/innovation-models/innovation-behavioral-health-ibh-model) Start date: Fall 2024 | The IBH Model tests the integration of primary care into community-based behavioral care settings. The model is a state-based model testing enhanced PBPM payments and performance-based payments for community-based behavioral health providers caring for adult patients with Medicare and/or Medicaid as their primary payer. | The model is available for up to eight states. CMS Notice of Funding Opportunity (https://www.grants.gov/search-results-detail/354873); state applications are due September 8, 2024 |
| Guiding an Improved Dementia Experience11 (https://www.cms.gov/priorities/innovation/innovation-models/guide) Start date: July 2024 | The GUIDE Model is a dementia care model focused on care coordination available to Medicare Part B providers. The model includes PBPMs for care management and caregiver support, payments for respite services and infrastructure payments for safety net providers. | The model is available nationwide. The application period is closed, and participants have been announced. |
| Transforming Maternal Health12 (https://www.cms.gov/priorities/innovation/innovation-models/transforming-maternal-health-tmah-model) Start date: January 2025 | The TMaH Model is a state-based model that includes a state-designed alternative payment model to improve maternal outcomes and access to the maternal health care workforce. Family physicians and other primary care clinicians are critical components of the maternal workforce, including prenatal, birth and postpartum care. | The model is available for up to 15 states. CMS Notice of Funding Opportunity (https://grants.gov/search-results-detail/354874); state applications are due September 20, 2024 |
IMPACT ON PRIMARY CARE PHYSICIANS
With the rapidly changing environment and a multitude of state-based models, there may be choices family physicians and primary care practices will have to make about which model(s) to participate in. While some models allow overlapping participation,13 such as participating in the Medicare Shared Savings Program and the AHEAD model at the same time, others do not. The AAFP is here to help you understand the options and navigate the changing landscape and its impact on how you can resource your practice to best meet your patients' needs. Considerations to account for as you evaluate your options include:
Financial incentives
Care delivery requirements
Reporting burdens
Ability to accept population accountability
Model alignment with practice goals
Community, network and payer alignment/partnership
EMERGING ISSUE: BROAD REFORMS TO SCALE PRIMARY CARE
Optimizing and scaling well-designed primary care payment is foundational to ensuring the long-term viability of family medicine practices. Unfortunately, our health care system underinvests in primary care as a whole, specifically in the bedrock on which most of these payment structures are currently based – FFS payments for primary care. While many factors contribute to underinvestment in primary care, the AAFP believes the following areas within the Medicare Physician Fee Schedule are significant culprits:
FFS payment is designed to pay for discrete services in ways that favor procedural service delivery.
FFS is incompatible with the continuous, comprehensive nature of relationship-based primary care.
Budget-neutrality requirements are unreasonably outdated and should not be narrowly focused only on physician services.
The lack of an inflationary update means payment has not kept pace with the inflationary costs of running a practice.
Each year, the CMS releases the MPFS proposed rule, and each year, the AAFP analyzes and responds to the proposal with comments and recommendations that put family physicians and patients at the forefront of payment considerations. While we continue to provide technical feedback on the MPFS and have just submitted this year's letter to CMS, we also believe that comprehensive, foundational reforms to the MPFS are needed for well-designed, value-based payments to be properly optimized and scaled in primary care. We describe our stance on this topic in this Beyond the Beltway feature and the AAFP's recent responses to Congress' requests for information here and here, and includes the following recommendations for reforming the MPFS:
Provide an annual inflationary update based on the Medicare Economic Index;
Improve FFS primary care payment rates with updated approaches to the valuation of both practice expenses and work relative value units; and
Reform budget-neutrality requirements.