
Fam Pract Manag. 2024;31(5):29-34
This educational supplement is funded by an unrestricted grant from Seqirus USA, Inc., and brought to you by the AAFP. Journal editors were not involved in the development of this content.
Introduction
Influenza causes an annual epidemic of upper respiratory illness in the United States. Flu season typically runs from October through May, with peak activity between December and February.1 The Centers for Disease Control and Prevention's preliminary in-season burden estimates indicated that from October 1, 2023, through June 15, 2024, there were2:
35 to 65 million influenza illnesses
16 to 30 million influenza medical visits
390,000 to 830,000 influenza hospitalizations
25,000 to 72,000 influenza deaths
You can put these figures in context by considering that motor vehicle traffic crashes caused an estimated 41,000 deaths in 2023.3 Despite the significant public health impact of influenza, the uptake of influenza vaccination has been low in recent years. For example, as of May 11, 2024, CDC data indicated that only 53.9% of U.S. children and 48.5% of U.S. adults received an influenza vaccine during the 2023–2024 flu season.4
Safe and effective vaccinations against seasonal influenza are available. As a family medicine clinician, you are well positioned to help protect your patients from severe illness and health complications by strongly recommending influenza vaccination as soon as it is available each year and providing the vaccine throughout the flu season.
Additional information and resources from the AAFP regarding influenza and influenza vaccines are available at aafp.org/vaccines.
Updates for the 2024–2025 Flu Season
In June 2024, the CDC's Advisory Committee on Immunization Practices unanimously approved the following updated recommendations for the 2024–2025 flu season5:
Routine influenza vaccination for all patients 6 months and older
Use of either high-dose or adjuvanted inactivated influenza vaccine for solid organ transplant recipients 18 to 64 years of age who are taking immunosuppressive medications
All influenza vaccines available for the 2024–2025 flu season will be trivalent vaccines, which is a change from the quadrivalent vaccines used in previous flu seasons. These vaccines will offer protection against two influenza A strains (H1N1 and H3N2) and the influenza B/Victoria lineage strain.5,6 Since the influenza B/Yamagata lineage strain has not circulated since March 2020,6 the trivalent vaccines will offer influenza protection that is similar to protection from the quadrivalent vaccines.
Recommendations for the 2024–2025 Flu Season5,7
All patients 6 months and older who do not have contraindications should receive the seasonal influenza vaccine.
Patients 65 years and older should receive a high-dose or adjuvanted inactivated influenza vaccine due to the limited effectiveness of standard-dose influenza vaccines in this population.
Patients with an egg allergy may receive either an egg-based or non–egg-based vaccine. However, patients who have had a severe allergic reaction to another component of an influenza vaccine should not receive a vaccine containing that component.
Solid organ transplant recipients 18 to 64 years of age who are taking immunosuppressive medications should receive a high-dose or adjuvanted inactivated influenza vaccine.
Live Attenuated Influenza Vaccine
For patients 2 through 49 years of age who have needle phobia or prefer intranasal influenza vaccination, live attenuated influenza vaccine, or LAIV, remains an option.8 It is important to note that patients must avoid close contact with severely immunocompromised people for seven days following administration of LAIV. In addition, there is a theoretical risk that recent use of influenza antiviral medications may impair LAIV effectiveness.8 Further study is needed to determine whether an interval between antiviral use and LAIV administration should be required.
LAIV is contraindicated in multiple populations, including the following8:
Pregnant people
People who are immunocompromised
People who have a cerebrospinal fluid leak
People who have cochlear implants
Children 2 to 4 years of age who have been diagnosed with wheezing or asthma
Children and adolescents who are at increased risk for Reye syndrome because they are taking aspirin or salicylates
Optimal Influenza Vaccination Timing
Most patients should get their influenza vaccine in September or October so they are protected during the peak transmission period from December to February. This includes people 65 years and older and pregnant people in their first or second trimester. They should wait until September or October to get their influenza vaccine unless vaccination later in the season will not be possible.
Influenza vaccination during July and August may be appropriate for some patients, including the following7:
Children who need two doses of influenza vaccine — This includes patients 6 months to 8 years of age who are receiving the influenza vaccine for the first time. The second dose must be administered at least four weeks after the first dose, so getting an initial vaccination in July or August allows these children to complete their two-dose series by September or October.
People who are in their third trimester of pregnancy during July and August — Vaccinating these patients in late summer helps protect infants who will be too young to receive their own influenza vaccine (i.e., younger than 6 months) during flu season.
Vaccine Effectiveness
The lifesaving impact of the influenza vaccine is significant. The CDC estimates that vaccination prevented 64,000 influenza-related deaths from the 2010–2011 flu season through the 2022–2023 flu season.9 As of late February 2024, interim data for the 2023–2024 flu season indicated that influenza vaccine effectiveness for preventing influenza-related illness was up to 67% in children and up to 49% in adults.10 In addition, the 2023–2024 seasonal influenza vaccines reduced pediatric influenza-associated hospitalization by up to 61% and adult influenza-associated hospitalization by up to 44%.10 Even if the seasonal influenza vaccine is not a perfect match for the main circulating strains of virus in a given year, it may provide protection against other strains that can cause illness during that flu season or a subsequent year.
Because certain populations (e.g., older adults, patients who are immunocompromised) often experience lower rates of vaccine effectiveness, it is particularly important for people with intact immune systems (e.g., children, younger adults) to get their influenza vaccine each year. By providing passive protection for higher-risk populations, these groups can help reduce the overall influenza disease burden.
Influenza Vaccine Safety
Influenza vaccine safety is closely monitored every year, and studies have shown that influenza vaccines are historically safe for most people. Data from a Vaccine Safety Datalink study showed a rate of 1.35 severe allergic reactions per one million doses of seasonal influenza vaccine administered, which is similar to the rate of 1.31 severe allergic reactions per one million doses of all vaccines.11 During the 2023–2024 flu season, nearly 160 million doses of influenza vaccine were administered to people in the United States,4 so an estimated 216 people may have experienced anaphylaxis. Clinicians administering influenza vaccines and people being vaccinated should monitor for signs and symptoms of a severe allergic reaction.
Vaccine administrators and/or patients should report adverse events after influenza vaccination to the Vaccine Adverse Event Reporting System at https://vaers.hhs.gov.
Reasons to Get the Influenza Vaccine
Patients may be complacent about getting an annual influenza vaccine partly because of their familiarity with the flu. Family medicine clinicians should emphasize the possible consequences of contracting influenza, including health effects, missed job or family obligations, financial impacts and the possibility of infecting susceptible family members and friends. Influenza vaccination is especially important for certain patient populations, including pregnant people and people with chronic health conditions (e.g., chronic obstructive pulmonary disease, heart disease, diabetes).12
If a patient points out that the vaccine does not guarantee protection from infection, it may be helpful to remind them vaccination can reduce the duration and severity of illness and the risk for hospitalization if they do get influenza. The CDC's Wild to Mild campaign highlights this point with the tagline, “A flu vaccine can take flu from wild to mild.”13 Getting vaccinated also protects other people in a patient's family and community, including those who are vulnerable to serious health complications from influenza.
Disparities in Influenza Vaccination Rates
RACIAL AND ETHNIC DISPARITIES
In the United States, disparities exist in the rates of influenza vaccination and severe influenza. A 2022 CDC study assessing racial and ethnic disparities in influenza hospitalization and vaccination coverage since 2009 found that non-Hispanic Black, American Indian or Alaska Native, and Hispanic adults had a statistically significant increased risk for hospitalization due to influenza.14 Figure 1 shows CDC data on cumulative rates of adult influenza hospitalizations by race and ethnicity during the flu seasons from 2009–2010 through 2022–2023.
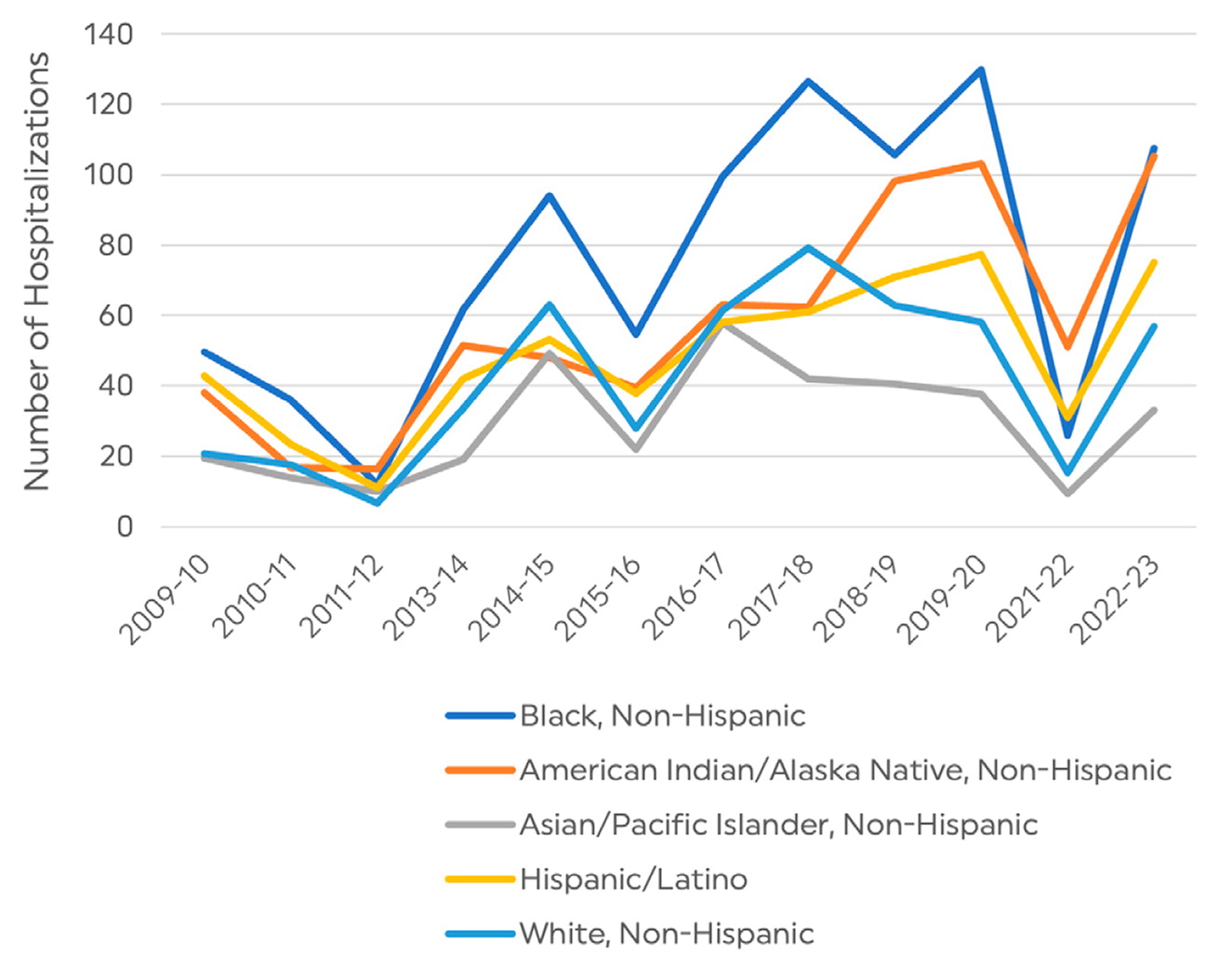
The 2022 study also found that vaccination rates were lower among Black, American Indian or Alaska Native, and Hispanic adults compared with vaccination rates for Asian and white adults. For example, in the 2021–2022 flu season, 53.9% of white adults and 54.2% of Asian adults received an influenza vaccine compared with 37.9% of Hispanic adults, 40.9% of American Indian or Alaska Native adults and 42% of Black adults.14 Since the 2010–2011 flu season, the rate of influenza vaccination among white and Asian adults has been consistently higher than the rate among Hispanic and Black adults. One key finding from the study was that “[t]he disparity in vaccination coverage by race and ethnicity was present among those who reported having medical insurance, a personal health care provider, and a routine medical checkup in the past year.”14 This suggests that limited access to health care and preventive services may not be the only barrier to influenza vaccination for certain populations.
DISPARITIES IN RURAL AREAS
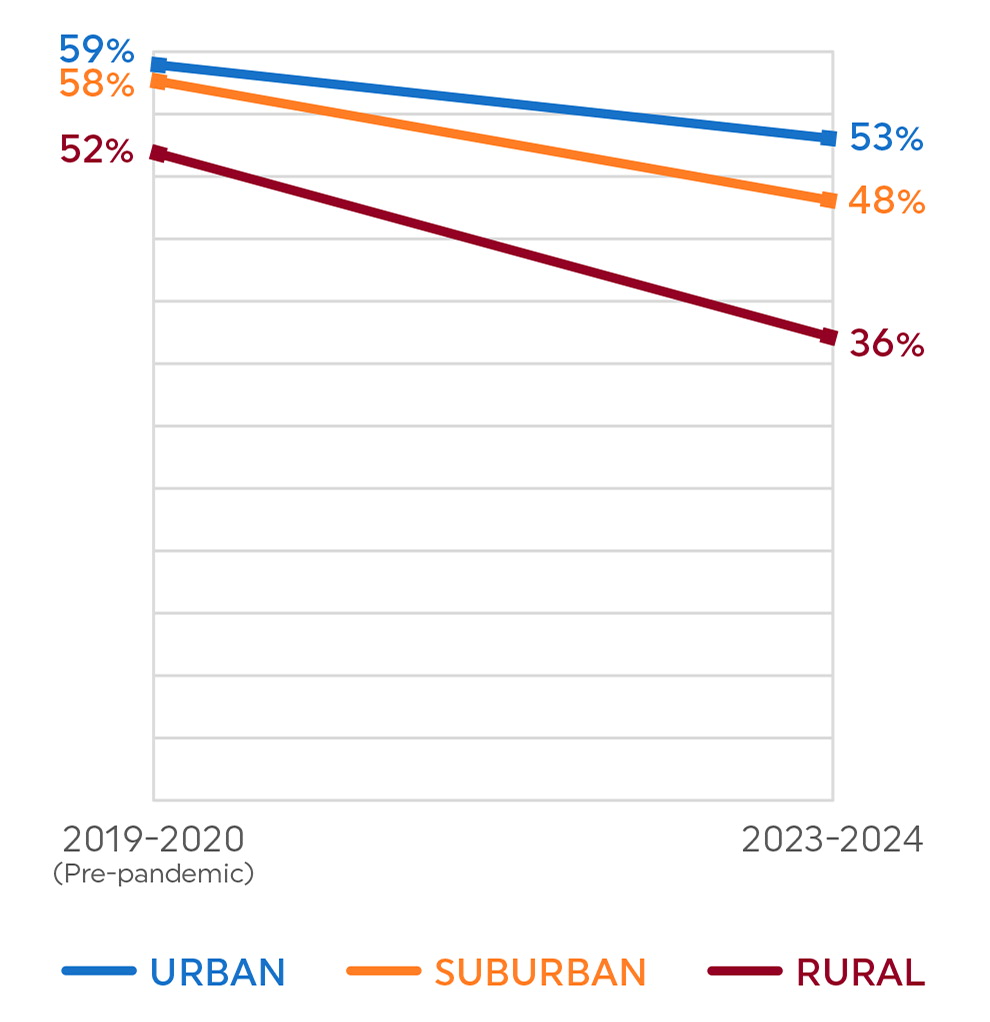
The CDC's midseason assessment of the 2023–2024 flu season highlighted disparities in vaccination coverage among people residing in rural areas.15 Figure 2 shows the difference in influenza vaccination rates among children in rural, urban and suburban areas prior to the COVID-19 pandemic and as of January 20, 2024. Similar disparities in influenza vaccination coverage were seen among adults. As of January 13, 2024, only 40% of rural adults had received the influenza vaccine compared with 48% of adults living in urban and suburban areas.15 The CDC noted, “This disparity in vaccine coverage based on urbanicity has been observed for several years and is widening.”15
Engaging Patients on Influenza Vaccination
In preparation for the upcoming flu season, health care teams should consider how to engage their patients on influenza vaccination more effectively.
Best immunization practices include the following:
Assess patients' immunization status at every visit to identify any needed vaccines.
Use presumptive, positive language to tell patients about the vaccines they need and recommend they get vaccinated during their current visit.
Address patients' vaccine-related concerns without being dismissive. These conversations can help overcome patients' vaccine hesitancy and build rapport and trust between patients and their care team.
If a patient declines a vaccine when it is offered, leave the door open for them to get it at another time. This honors the patient's autonomy while also reassuring them that they still have the opportunity to get vaccinated in the future.
In addition to preparing for flu season within your family medicine practice, you can look for opportunities to partner formally and informally with community leaders on vaccination efforts. Administering vaccines in settings outside of the clinic may increase access for people who prefer not to enter a health care facility for various reasons. By approaching these efforts with cultural humility and working with community leaders, you help ensure that messaging about influenza vaccination is culturally relevant and gets disseminated effectively. In addition, if people in the community express a lack of trust in the health care system or a sense of disconnection from medical care, you will be able to better understand and address their perspective.
ADDRESSING BARRIERS TO INFLUENZA VACCINATION
Given the current low levels of vaccine uptake and widening disparities in influenza vaccination rates, you have an opportunity to explore and address reasons your patients may be resistant to getting an influenza vaccine. Table 1 offers brief, evidence-based responses to questions patients often ask about influenza vaccination.
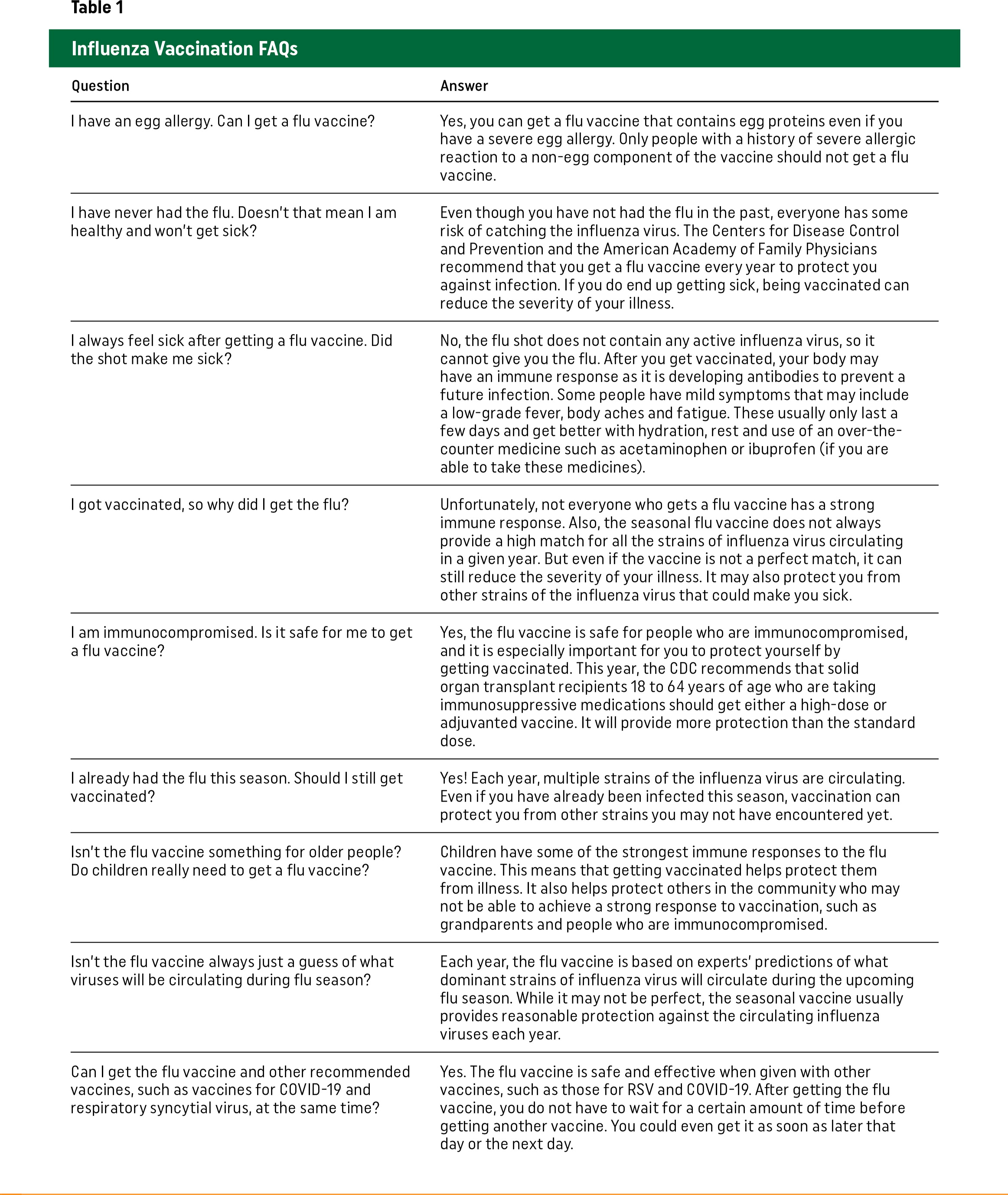
Table 1. Influenza Vaccination FAQs
| Question | Answer |
|---|---|
| I have an egg allergy. Can I get a flu vaccine? | Yes, you can get a flu vaccine that contains egg proteins even if you have a severe egg allergy. Only people with a history of severe allergic reaction to a non-egg component of the vaccine should not get a flu vaccine. |
| I have never had the flu. Doesn't that mean I am healthy and won't get sick? | Even though you have not had the flu in the past, everyone has some risk of catching the influenza virus. The Centers for Disease Control and Prevention and the American Academy of Family Physicians recommend that you get a flu vaccine every year to protect you against infection. If you do end up getting sick, being vaccinated can reduce the severity of your illness. |
| I always feel sick after getting a flu vaccine. Did the shot make me sick? | No, the flu shot does not contain any active influenza virus, so it cannot give you the flu. After you get vaccinated, your body may have an immune response as it is developing antibodies to prevent a future infection. Some people have mild symptoms that may include a low-grade fever, body aches and fatigue. These usually only last a few days and get better with hydration, rest and use of an over-the-counter medicine such as acetaminophen or ibuprofen (if you are able to take these medicines). |
| I got vaccinated, so why did I get the flu? | Unfortunately, not everyone who gets a flu vaccine has a strong immune response. Also, the seasonal flu vaccine does not always provide a high match for all the strains of influenza virus circulating in a given year. But even if the vaccine is not a perfect match, it can still reduce the severity of your illness. It may also protect you from other strains of the influenza virus that could make you sick. |
| I am immunocompromised. Is it safe for me to get a flu vaccine? | Yes, the flu vaccine is safe for people who are immunocompromised, and it is especially important for you to protect yourself by getting vaccinated. This year, the CDC recommends that solid organ transplant recipients 18 to 64 years of age who are taking immunosuppressive medications should get either a high-dose or adjuvanted vaccine. It will provide more protection than the standard dose. |
| I already had the flu this season. Should I still get vaccinated? | Yes! Each year, multiple strains of the influenza virus are circulating. Even if you have already been infected this season, vaccination can protect you from other strains you may not have encountered yet. |
| Isn't the flu vaccine something for older people? Do children really need to get a flu vaccine? | Children have some of the strongest immune responses to the flu vaccine. This means that getting vaccinated helps protect them from illness. It also helps protect others in the community who may not be able to achieve a strong response to vaccination, such as grandparents and people who are immunocompromised. |
| Isn't the flu vaccine always just a guess of what viruses will be circulating during flu season? | Each year, the flu vaccine is based on experts' predictions of what dominant strains of influenza virus will circulate during the upcoming flu season. While it may not be perfect, the seasonal vaccine usually provides reasonable protection against the circulating influenza viruses each year. |
| Can I get the flu vaccine and other recommended vaccines, such as vaccines for COVID-19 and respiratory syncytial virus, at the same time? | Yes. The flu vaccine is safe and effective when given with other vaccines, such as those for RSV and COVID-19. After getting the flu vaccine, you do not have to wait for a certain amount of time before getting another vaccine. You could even get it as soon as later that day or the next day. |
Resources to Enhance Outreach for the 2024–2025 Flu Season
www.immunize.org/clinical/a-z – Immunize.org is a nonprofit organization offering free clinical resources, including patient-friendly handouts that can be printed or added to an after-visit summary.
familydoctor.org/influenza – The Influenza Health Hub features trusted, reliable health information for patients from the American Academy of Family Physicians.
www.cdc.gov/flu/resource-center/index.htm – The CDC's Seasonal Influenza Resource Center offers a variety of communication and education materials, including wall signs, scripted messaging for patient portal outreach, and social media and print resources.
www.cdc.gov/flu/resource-center/nivw/activities.htm – The CDC's National Influenza Vaccination Week Digital Media Toolkit provides resources, vaccination messages and activities that practices can use in December to encourage people to get their flu vaccine before the peak of the season in January.
www.cdc.gov/flu/weekly/index.htm – FluView, the CDC's weekly influenza surveillance report, can be used to monitor the level of influenza activity during flu season. It provides data that may help bolster clinician recommendations during times of peak influenza transmissibility.
