
Fam Pract Manag. 2025;32(1):10-12
The publication of this supplement is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.

The consolidation of health care organizations has accelerated dramatically during the past 10-plus years, with a significant impact on family physicians, their practices and patients.1,2 Consolidation can occur horizontally (e.g., organizations provide similar services, such as when two hospitals merge or one acquires another); vertically (e.g., an organization adds or expands its service offerings, such as when a hospital acquires a physician practice); or cross-market (e.g., organizations in different geographic markets join together, such as when Risant Health became a new entity when Kaiser Permanente finalized its merger with Geisinger Health).1,3
Motivating factors in the rise of health care consolidations include the need for improved efficiencies due to financial pressures, regulatory requirements and/or technological advancements.2 These factors can vary based on the type of transaction (i.e., merger versus acquisition) and the level of aligned interests between the organizations. Ideally, their respective interests would be highly aligned, but that is not always the case, with financial considerations often playing a significant role.
American Academy of Family Physicians Executive Vice President and Chief Executive Officer Shawn Martin testified to the U.S. Senate Committee on Finance that far too often “practices that have consolidated did so not from a position of opportunity, but to avoid economic ruin.”4
Financially, many smaller, physician-owned practices have struggled to keep up with the rising costs of health care delivery and the complexities of administrative requirements. By joining larger organizations, they often do so for financial reasons and to gain access to greater resources, capital and negotiating power with insurers, which can lead to more sustainable operations.2,5
IMPACT OF HEALTH CARE CONSOLIDATION FOR FAMILY PHYSICIANS
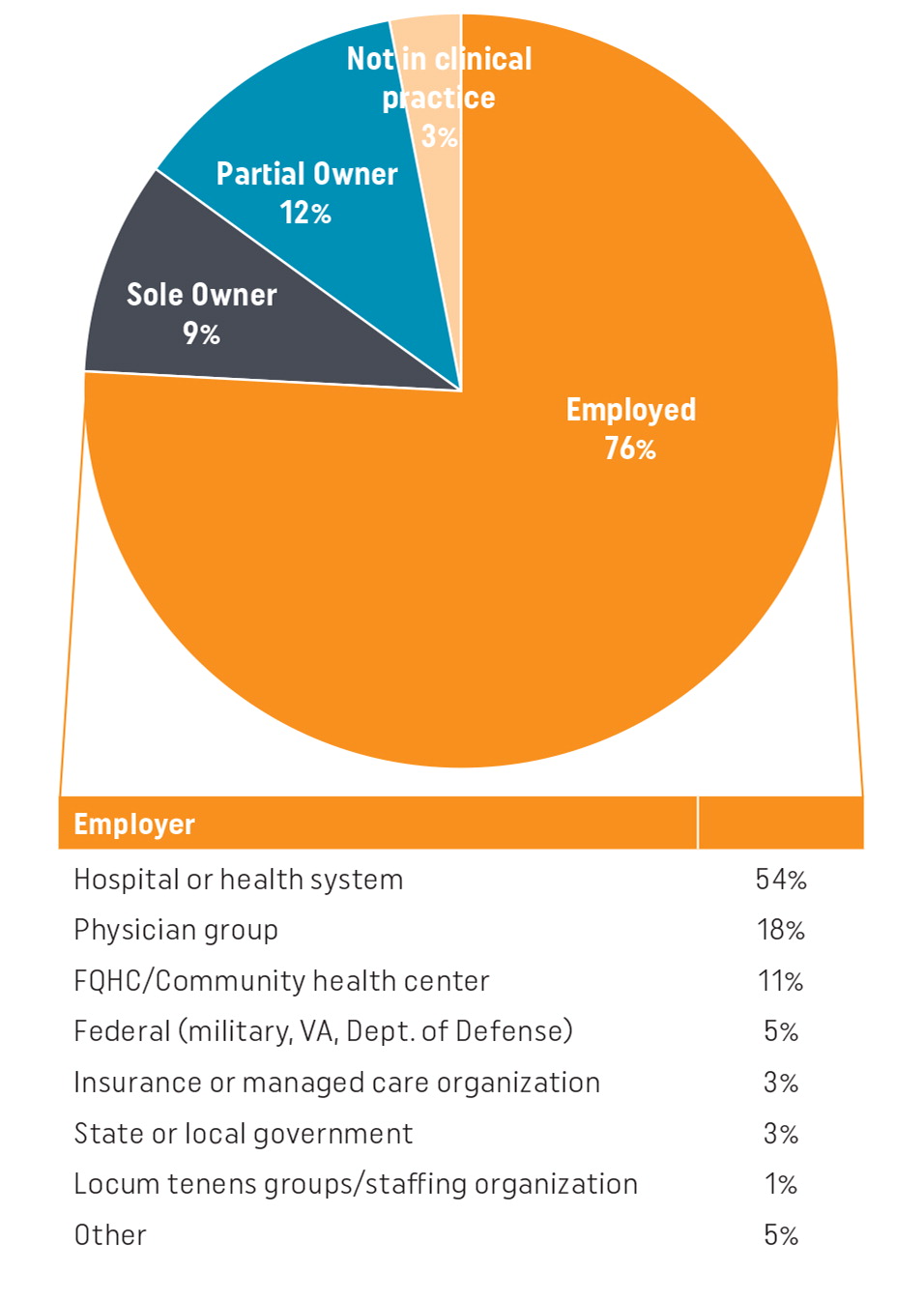
Today, we have a substantially different physician practice landscape with fewer independent practices and a growing number of physicians working as employees of large health systems. Your collective voices through the annual AAFP Membership Survey tells us that 76% of AAFP members are employed, most commonly by a hospital or health system (54%) or physician group (18%), as illustrated in Figure 1. Only 21% of AAFP members are sole or partial owners of their practice.4 By contrast, in 2011, 59% of AAFP members were employed and 37% were sole or partial owners of their practice.
These findings echo employment/ownership findings of other physician specialties. The Physician Practice Benchmark Survey, conducted bi-annually by the American Medical Association, reports that practices wholly owned by physicians (i.e., private practices) decreased 13% between 2012 and 2020 (from 60.1% to 46.7%).5 Physicians working in larger practices (50-plus physicians) increased from 12.2% to 18.3% over the same period.
AAFP ADVOCACY AND WORK TO BETTER EQUIP YOU
The AAFP is working hard to address the foundational issues that have contributed to the increase in practice acquisition. At the top of that list are advocating to strengthen investment in primary care (www.aafp.org/advocacy/advocacy-topics/physician-payment.html) and eliminating administrative burdens (www.aafp.org/family-physician/practice-and-career/administrative-simplification/prior-authorization.html) associated with getting paid for the care you deliver. We are tackling these priorities by advocating on your behalf with federal regulators and national payers in the private sector. We have a wealth of resources and information for chapters to help you effectively advocate and influence decisions to improve family physician employment.
The AAFP strongly stands in support of independent practices (www.aafp.org/about/policies/all/independent-practice.html) and regularly advocates for payment policies and practices “to ensure independent practices are not left behind,” a sentiment expressed by AAFP Board Chair and independent practice owner Steven Furr, MD, in testimony before the U.S. Senate Committee on Finance. We support independent practices in all their forms, including direct primary care (www.aafp.org/about/policies/all/direct-primary-care.html), with a wide range of resources (www.aafp.org/family-physician/practice-and-career/delivery-payment-models/direct-primary-care.html) for members interested in DPC practice. Further, the AAFP collaborates with other organizations to hold the DPC Summit (www.dpcsummit.org/home.html) each year to inform and equip physicians who may be interested in the practice model.
The AAFP is focused on ensuring you are equipped with the knowledge and resources to determine the path that best meets your career needs, whether you are employed or a practice owner. If you are employed, we have a vast library of career and employment resources (www.aafp.org/family-physician/practice-and-career/managing-your-career.html) to choose the best employer for you and to help negotiate a beneficial contract.
With so many employed physicians, the AAFP recognizes that decisions made by your employing organizations can strengthen or weaken your position as a physician and the family medicine workforce. In 2023, the AAFP sought to understand better the principles family physicians value in their employment settings and what is working and what is not. With input from AAFP members — including those in leadership positions within organizations employing family physicians — the AAFP adopted as policy at the 2023 Congress of Delegates the Principles to Optimize Family Physician Employment (Position Paper) (www.aafp.org/about/policies/all/principles-employment.html).
The principles in the position paper describe ideal employment practices that value and prioritize primary care and family medicine, foster professional satisfaction and retention, support primary care and family medicine and advance equity in employment for family physicians. The principles are organized around the following themes:
Total compensation
Leadership and culture
Clinical and operational autonomy
Care delivery supports
Contracting and transparency
AAFP RESOURCES
The AAFP is continually developing resources to assist you as you make important career decisions, including the following:
If you are newly entering family medicine, considering a job change or currently employed, the Signs of a Good Physician Employer infographic can help you evaluate employers.
Centered around our ideal employment practices, you'll find our Best Practices for Health Care Organizations Employing Family Physicians. If you are one of the many AAFP members in a leadership position within your organization — or if you own your practice — this document further outlines the ideal employment practices. It can help you assess how well you or your organization is living up to those principles.
The AAFP's Family Medicine Career Benchmark Dashboard gives you access to compensation benchmarks at a national, regional or state-level to inform your professional goals and career decisions. The dashboard represents survey data from more than 7,500 family physicians.
The resources noted here are only a small window into the wealth of information the AAFP has to support our members in achieving professional satisfaction and fulfillment in their careers as family physicians. Consider bookmarking our Practice & Career webpage (www.aafp.org/family-physician/practice-and-career.html) as we update and add new content to help in your professional journey.
ALIGNING ORGANIZATIONAL VALUES WITH FAMILY PHYSICIAN PRIORITIES
The questions in Table 1 are designed to help you assess how well your organization's actions align with the values and priorities of family physicians. Use this tool to evaluate your current or potential employment situation. You can also use the questions if you are a practice owner or to spark conversations with leaders in your organization to identify best practices and ways to improve family physician employment.
Total Compensation
|
Leadership
|
Clinical and Operational Autonomy
|
Care Delivery Supports
|
Contracting and Transparency
|
