
Am Fam Physician. 2006;74(5):756-762
This is part I of a two-part article on cirrhosis and chronic liver failure. Part II, “Complications and Treatment,” appears in this issue of AFP.
Patient information: See related handout on cirrhosis and chronic liver failure, written by the authors of this article.
Author disclosure: Nothing to disclose.
Cirrhosis and chronic liver failure are leading causes of morbidity and mortality in the United States, with the majority of preventable cases attributed to excessive alcohol consumption, viral hepatitis, or nonalcoholic fatty liver disease. Cirrhosis often is an indolent disease; most patients remain asymptomatic until the occurrence of decompensation, characterized by ascites, spontaneous bacterial peritonitis, hepatic encephalopathy, or variceal bleeding from portal hypertension. Physical examination of patients with cirrhosis may reveal a variety of findings that necessitate a hepatic- or gastrointestinal-based work-up to determine the etiology. Some patients already may have had laboratory or radiographic tests that incidentally uncovered signs of cirrhosis and its comorbidities. No serologic or radiographic test can accurately diagnose cirrhosis. A significant correlation has been demonstrated between persistently elevated liver function tests and biopsy-proven underlying hepatic disease; thus, a more targeted serologic work-up is indicated in patients whose liver function test results are persistently abnormal. Unnecessary medications and surgical procedures should be avoided in patients with cirrhosis. Referral for liver biopsy should be considered only after a thorough, non-invasive serologic and radiographic evaluation has failed to confirm a diagnosis of cirrhosis; the benefit of biopsy outweighs the risk; and it is postulated that biopsy will have a favorable impact on the treatment of chronic liver disease.
Cirrhosis and chronic liver failure together were the 12th most common cause of death in the United States in 2002, accounting for 27,257 deaths (9.5 per 100,000 persons), with a slight male predominance.1 Approximately 40 percent of patients with cirrhosis are asymptomatic, and the condition often is discovered during a routine examination with laboratory or radiographic studies, or at autopsy. In 2000, there were 360,000 U.S. hospital discharges related to cirrhosis and liver failure.1 This article, part I of a two-part series, outlines the diagnosis and evaluation of cirrhosis and chronic liver failure (Figure 1). Part II discusses complications and treatment.2
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Although no laboratory test can diagnose cirrhosis accurately, liver function tests, a complete blood count with platelets, and a prothrombin time test should be performed if a liver abnormality is suspected. | C | 14 |
| If clinical, laboratory, and radiographic data are inconclusive, but suspicion of cirrhosis remains, a diagnostic liver biopsy should be performed. | C | 15,17 |
| If serum transaminase levels are greater than twice the upper limit of normal or remain elevated for longer than six months, additional serologic studies should be performed to evaluate for various etiologies of cirrhosis. If clinical suspicion for liver disease is high, further serologic work-up is warranted earlier. | C | 15 |
| Abdominal ultrasonography is a specific, reliable, noninvasive, fast, and cost-effective test that should be used as a first-line radiographic study for diagnosing cirrhosis. | C | 20,21 |
Single or multifactorial insults to the liver ultimately lead to cirrhosis, the most common being alcohol abuse, chronic hepatitis C, and obesity with concomitant nonalcoholic fatty liver disease (Table 1).3,4 Nonalcoholic fatty liver disease (NAFLD; formerly known as nonalcoholic steatohepatitis, or NASH) is an increasingly common cause of liver injury; risk factors include obesity, diabetes, hypertriglyceridemia, and profound weight loss after jejunoileal bypass.5
| Most common causes | |
| Alcohol (60 to 70 percent) | |
| Biliary obstruction (5 to 10 percent) | |
| Biliary atresia/neonatal hepatitis | |
| Congenital biliary cysts | |
| Cystic fibrosis | |
| Primary or secondary biliary cirrhosis | |
| Chronic hepatitis B or C (10 percent) | |
| Hemochromatosis (5 to 10 percent) | |
| NAFLD (10 percent)—most commonly resulting from obesity; also can occur after jejunoileal bypass | |
| Less common causes | |
| Autoimmune chronic hepatitis types 1, 2, and 3 | |
| Drugs and toxins | |
| Alpha-methyldopa (Aldomet) | |
| Amiodarone (Cordarone) | |
| Isoniazid (INH) | |
| Methotrexate | |
| Oxyphenisatin (Prulet)* | |
| Perhexiline* | |
| Troglitazone (Rezulin)* | |
| Vitamin A | |
| Genetic metabolic disease | |
| α1-Antitrypsin deficiency | |
| Amino acid disorders (e.g., tyrosinemia) | |
| Bile acid disorders | |
| Carbohydrate disorders (e.g., fructose intolerance, galactosemia, glycogen storage diseases) | |
| Lipid disorders (e.g., abetalipoproteinemia) | |
| Porphyria | |
| Urea cycle defects (e.g., ornithine carbamoyltransferase deficiency) | |
| Wilson’s disease | |
| Idiopathic/miscellaneous | |
| Granulomatous liver disease (e.g., sarcoidosis) | |
| Idiopathic portal fibrosis | |
| Indian childhood cirrhosis | |
| Polycystic liver disease | |
| Infection | |
| Brucellosis | |
| Congenital or tertiary syphilis | |
| Echinococcosis | |
| Schistosomiasis | |
| Vascular abnormalities | |
| Chronic, passive hepatic congestion caused by right-sided heart failure, pericarditis | |
| Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease) | |
| Veno-occlusive disease | |
According to estimates from the United Network for Organ Sharing, 75 to 80 percent of cirrhosis cases could be prevented by eliminating alcohol abuse, and approximately 3.9 million Americans have chronic hepatitis C.6 In August 2005, there were 17,935 persons with cirrhosis (from various etiologies) in the United States who were awaiting a liver transplant.6 Mortality rates in patients with alcoholic liver disease are considerably higher than in patients with other forms of cirrhosis. The Centers for Disease Control and Prevention estimates that 75,766 deaths and 2.3 million years of potential life lost during 2001 were attributable to excessive alcohol use, an average of approximately 30 years of potential life lost for each alcohol-attributable death.7
Definitions and Etiologies
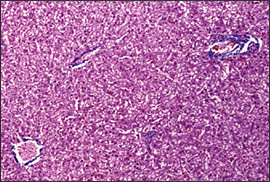
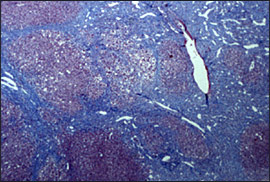
The liver aids greatly in the maintenance of metabolic homeostasis by processing dietary amino acids, carbohydrates, lipids, and vitamins; metabolizing cholesterol and toxins; producing clotting factors; and storing glycogen. Injury to the liver parenchyma associated with an influx of acute or chronic inflammatory cells is termed hepatitis. Cirrhosis refers to a progressive, diffuse, fibrosing, nodular condition that disrupts the entire normal architecture of the liver (Figures 2 through 4; Table 1).3,4 Fibrosis previously was thought to be an irreversible scarring process formed in response to inflammation or direct toxic insult to the liver, but current evidence suggests that fibrosis may be reversible in some patients with chronic hepatitis B after antiretroviral therapy.8


Any chronic insult to the liver can cause progression to cirrhosis. Although numerous pathophysiologic mechanisms of injury exist, the final common pathway is persistent wound healing resulting in hepatic parenchymal fibrosis. In most persons, approximately 80 to 90 percent of the liver parenchyma must be destroyed before liver failure is manifested clinically. When complications of cirrhosis occur, they typically are related to impaired hepatic function or actual physical disruption and reorganization of the liver parenchyma.3
Clinical Presentation
HISTORY
Cirrhosis often is a silent disease, with most patients remaining asymptomatic until decompensation occurs. Physicians should inquire about risk factors that predispose patients to cirrhosis (Figure 1).Quantity and duration of alcohol consumption is an important factor in the early diagnosis of cirrhosis.3 Other risk factors include those for hepatitis B and C transmission (e.g., birthplace in endemic areas, sexual history exposure risk, intranasal or intravenous drug use, body piercing or tattooing, accidental contamination with blood or body fluids), as well as transfusion history and personal or family history of autoimmune or hepatic diseases.3
Early and well-compensated cirrhosis can manifest as anorexia and weight loss, weakness, fatigue, and even osteoporosis as a result of vitamin D malabsorption and subsequent calcium deficiency. Decompensated disease can result in complications such as ascites, spontaneous bacterial peritonitis, hepatic encephalopathy, and variceal bleeding from portal hypertension (discussed further in part II2). Clinical symptoms at presentation may include jaundice of the eyes or skin, pruritus, gastrointestinal bleeding, coagulopathy, increasing abdominal girth, and mental status changes. Each of these clinical findings is the result of impaired hepatocellular function with or without physical obstruction secondary to cirrhosis. Because hepatic enzyme synthesis is required for drug metabolism, heightened sensitivity and medication toxicity may occur in patients with impaired hepatic enzyme synthesis.3,9
PHYSICAL EXAMINATION
Physical examination of patients with cirrhosis may reveal a variety of findings that should lead to a targeted hepatic- or gastrointestinal-based work-up (Table 2).10 Many patients will already have had serologic or radiographic tests or an unrelated surgical procedure that incidentally uncovered signs of cirrhosis.
| Abdominal wall vascular collaterals (caput medusa) | |
| Ascites | |
| Asterixis | |
| Clubbing and hypertrophic osteoarthropathy | |
| Constitutional symptoms, including anorexia, fatigue, weakness, and weight loss | |
| Cruveilhier-Baumgarten murmur—a venous hum in patients with portal hypertension | |
| Dupuytren’s contracture | |
| Fetor hepaticus—a sweet, pungent breath odor | |
| Gynecomastia | |
| Hepatomegaly | |
| Jaundice | |
| Kayser-Fleischer ring—brown-green ring of copper deposit around the cornea, pathognomonic for Wilson’s disease | |
| Nail changes: | |
| Muehrcke’s nails—paired horizontal white bands separated by normal color | |
| Terry’s nails—proximal two thirds of nail plate appears white, whereas the distal one third is red | |
| Palmar erythema | |
| Scleral icterus | |
| Vascular spiders (spider telangiectasias, spider angiomata) | |
| Splenomegaly | |
| Testicular atrophy | |
Most patients with cirrhosis severe enough to lead to ascites have additional stigmata of cirrhosis on physical examination. Accurately diagnosing ascites depends upon the amount of f luid present in the abdomen, the technique used to examine the patient, and the patient’s habitus. The most useful physical finding in confirming the presence of ascites is f lank dullness to percussion. When this is detected, it is helpful to determine whether it shifts with rotation of the patient (shifting dullness) or whether it can be percussed anteriorly. One study found absence of f lank dullness to be the most accurate predictor against the presence of ascites; the probability of ascites without f lank dullness was less than 10 percent.11 Approximately 1,500 mL of fluid must be present before dullness is detected on physical examination, whereas routine ultrasonography can detect as little as 50 mL of f luid in the abdomen.10
Vascular spiders (spider angiomata, spider telangiectasias) are vascular lesions usually found on the trunk, face, and upper extremities. Although their pathogenesis is incompletely understood, it is believed that their presence in men is associated with an increase in the estradiol to free testosterone ratio.12 Vascular spiders are not specific for cirrhosis: they also occur during pregnancy, in patients with severe malnutrition, and in healthy persons. The number and size of vascular spiders have been shown to correlate with the severity of chronic liver disease. Patients with numerous large vascular spiders are at increased risk for variceal hemorrhage.13
Laboratory Evaluation
No serologic test can diagnose cirrhosis accurately.3 The term liver function tests is a misnomer because the assays in most standard liver panels do not reflect the function of the liver correctly.10 Although liver function tests may not correlate exactly with hepatic function, interpreting abnormal biochemical patterns in conjunction with the clinical picture may suggest certain liver diseases. When a liver abnormality is suspected or identified, a liver panel, a complete blood count (CBC) with platelets, and a prothrombin time test should be performed.14 Common tests in standard liver panels include the serum enzymes aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase, and γ-glutamyltransferase; total, direct, and indirect serum bilirubin; and serum albumin. The ALT is thought to be the most cost-effective screening test for identifying metabolic or drug-induced hepatic injury, but like other liver function tests, it is of limited use in predicting degree of inflammation and of no use in estimating severity of fibrosis.15 One study found that a platelet count of less than 160 K per mm3has a sensitivity of 80 percent for detecting cirrhosis in patients with chronic hepatitis C.16
A prospective study showed a strong correlation between liver function test results elevated to greater than twice the upper limit of normal for at least six months and underlying liver disease proved by liver biopsy.17 Additional serologic studies should be pursued in such circumstances to evaluate for various etiologies of cirrhosis (Table 3).14,15,18,19 If clinical suspicion for liver disease is high, then further serologic work-up is warranted within six months.15 If a patient has a persistently increased ALT level, viral hepatitis serologies should be assayed. If these are negative, the remaining serologic work-up should include an antinuclear antibodies test or anti–smooth muscle antibody test, or both, to evaluate for autoimmune hepatitis; and a fasting transferrin saturation level or unsaturated iron-binding capacity and ferritin level18 to evaluate for hereditary hemochromatosis.15 In patients younger than 40 years in whom Wilson’s disease is suspected, serum ceruloplasmin and copper levels should be measured,19 but screening all patients with chronic hepatic injury for Wilson’s disease is not indicated.15 Primary biliary cirrhosis or primary sclerosing cholangitis should be suspected in patients with chronic cholestasis. Testing for α1-antitrypsin (A1AT) deficiency may be of benefit in patients with chronic hepatic injury and no other apparent cause. Although the role of A1AT deficiency in liver disease in adults is not clearly defined, testing is especially important in neonates with evidence of hepatic injury.15 Ultrasonography or biopsy is necessary to establish the diagnosis of NAFLD.
| Etiology | Laboratory tests and results |
|---|---|
| Alcoholic liver disease | AST:ALT ratio > 2* |
| Elevated GGT | |
| α1-Antitrypsin deficiency | Decreased serum α1-antitrypsin |
| Genetic screening recommended in equivocal cases | |
| Autoimmune hepatitis (type 1) | Positive ANA and/or ASMA in high titer |
| Chronic hepatitis B | Positive HBsAg and HBeAg qualitative assays |
| Once HBeAg is negative and HBeAb is positive, HBsAg should be monitored periodically to determine viral clearance. | |
| Hepatitis B virus DNA quantification used to document viral clearance | |
| Elevated AST and/or ALT* | |
| Chronic hepatitis C | Positive hepatitis C virus antibody qualitative assay |
| HCV RNA quantification used to document viral clearance | |
| HCV viral genotype to determine potential response to antiretroviral therapy | |
| Elevated AST and/or ALT* | |
| Hepatocellular carcinoma | Elevated alpha fetoprotein, AST, and/or ALT* |
| Elevated ALP with obstruction or cholestasis | |
| Hereditary hemochromatosis | Elevated fasting transferrin saturation, unsaturated iron-binding capacity, or ferritin. A transferrin saturation ≥45 percent or an unsaturated iron-binding capacity 155 mcg per dL (27.7 μmol per L) should be followed by analysis for HFE (hemochromatosis) gene mutations. |
| Nonalcoholic fatty liver disease | Elevated AST and/or ALT* |
| Ultrasonography or biopsy necessary to establish diagnosis. | |
| Primary biliary cirrhosis and primary sclerosing cholangitis | Diagnosis made via contrast cholangiography, can be supported clinically by positive antimitochondrial antibody (primary biliary cirrhosis) or antineutrophil cytoplasmic antibody (primary sclerosing cholangitis) in high titers. |
| Elevated AST, ALT, and ALP common | |
| Wilson’s disease | Serum ceruloplasmin < 20 mg per dL (200 mg per L) (normal: 20 to 60 mg per dL [200 to 600 mg per L]), or low serum copper level (normal: 80 to 160 mcg per dL [12.6 to 25.1 μmol per L]) |
| Basal 24-hour urinary copper excretion > 100 mcg (1.57 μmol) (normal: 10 to 80 mcg [0.16 to 1.26 μmol]) | |
| Genetic screening recommended in equivocal cases, but must be able to detect multiple mutations in Wilson’s disease gene. |
Radiographic Studies
Although various radiographic studies may suggest the presence of cirrhosis, no test is considered a diagnostic standard.3 The major use of radiographic studies is to detect ascites, hepatosplenomegaly, hepatic or portal vein thromboses, and hepatocellular carcinoma, all of which strongly suggest cirrhosis.
ULTRASONOGRAPHY
Abdominal ultrasonography with Doppler is a noninvasive, widely available modality that provides valuable information regarding the gross appearance of the liver and blood flow in the portal and hepatic veins in patients suspected to have cirrhosis. Ultrasonography should be the first radiographic study performed in the evaluation of cirrhosis because it is the least expensive and does not pose a radiation exposure risk or involve intravenous contrast with the potential for nephrotoxicity as does computed tomography (CT). Nodularity, irregularity, increased echogenicity, and atrophy are ultrasonographic hallmarks of cirrhosis. In advanced disease, the gross liver appears small and multinodular, ascites may be detected, and Doppler flow can be significantly decreased in the portal circulation. The discovery of hepatic nodules via ultrasonography warrants further evaluation because benign and malignant nodules can have similar ultrasonographic appearances.20 A study using high-resolution ultrasonography in patients with cirrhosis confirmed with biopsy or laparoscopy found a sensitivity and specificity for cirrhosis of 91.1 and 93.5 percent, respectively, and positive and negative predictive values of 93.2 and 91.5 percent, respectively.21
CT AND MRI
CT and magnetic resonance imaging (MRI) generally are poor at detecting morphologic changes associated with early cirrhosis, but they can accurately demonstrate nodularity and lobar atrophic and hypertrophic changes, as well as ascites and varices in advanced disease. Although MRI sometimes differentiates among regenerating or dysplastic nodules and hepatocellular carcinoma, it is best used as a follow-up study to determine whether lesions have changed in appearance and size.20 CT portal phase imaging can be used to assess portal vein patency, although flow volume and direction cannot be determined accurately.22
Although used rarely, magnetic resonance angiography (MRA) can assess portal hypertensive changes including flow volume and direction, as well as portal vein thrombosis.22 One study reported that MRI can accurately diagnose cirrhosis and provide correlation with its severity.23 Despite the potential of MRI and MRA in the diagnosis and evaluation of patients with cirrhosis, their widespread use is limited by their expense and by the ability of routine ultrasonography with Doppler to obtain adequate information for the diagnosis of cirrhosis and presence of complications.
Liver Biopsy
Referral for liver biopsy should be considered after a thorough, noninvasive serologic and radiographic evaluation has failed to confirm a diagnosis of cirrhosis; the benefit of biopsy outweighs the risk; and it is postulated that biopsy will have a favorable impact on the treatment of chronic liver disease. The sensitivity and specificity for an accurate diagnosis of cirrhosis and its etiology range from 80 to 100 percent, depending on the number and size of the histologic samples and on the sampling method.24
Liver biopsy is performed via percutaneous, transjugular, laparoscopic, open operative, or ultrasonography- or CT-guided fine-needle approaches. Before the procedure, a CBC with platelets and prothrombin time measurement should be obtained. Patients should be advised to refrain from consumption of aspirin and nonsteroidal anti-inflammatory drugs for seven to 10 days before the biopsy to minimize the risk of bleeding.