
Am Fam Physician. 2018;98(11):654-660
Patient information: See related handout on common dental infections, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Oral health directly affects overall health and quality of life. More Americans lack dental insurance than medical insurance. Patients with poor oral health are more likely to have respiratory and cardiovascular diseases, adverse pregnancy outcomes, and diabetes mellitus. Early childhood caries is the most common chronic condition in American children. Certain illicit and prescription drugs increase the risk of enamel erosion and caries formation in adults. Incision and drainage is the treatment of choice for dental abscess. Risk factors for periodontal disease include smoking, diabetes, human immunodeficiency virus infection, use of certain medications, and genetic susceptibility. Patients with gingivitis typically present with swollen, erythematous gum tissue that bleeds easily with brushing or flossing. One in three children will have an injury to the primary teeth, and one in five 12-year-old children will have an injury to the permanent teeth. All dental fractures should be evaluated with imaging and managed in conjunction with a dental professional. Immediate reimplantation is the preferred treatment for avulsed permanent teeth. Primary care clinicians are well positioned to reduce rates of oral disease. Family physicians can incorporate oral health into routine practice through counseling about diet, oral hygiene, smoking cessation, and fluoride supplementation; application of fluoride varnish; and screening for dental disease.
At the turn of the millennium, the U.S. Surgeon General declared dental disease a silent epidemic.1 Despite the decades-old tradition of separating oral and systemic health and hygiene, there are inseparable linkages.2,3 Oral health directly affects overall health and quality of life.4 A careful oral examination reveals information about numerous systemic conditions, from nutritional deficiencies to infections and cancer. Poor oral health has been associated with respiratory and cardiovascular diseases, adverse pregnancy outcomes, and diabetes mellitus.5 Training in oral health care varies among medical schools and residency programs.6,7
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Families should be counseled about effective caries prevention in children, including the benefits of dental sealants and not giving milk, formula, or juice in bottles to children whose teeth have started to erupt; and how to brush and floss at all ages. | C | 18, 27, 29, 32 |
| Gingivitis can be prevented or reversed with regular dental cleaning, proper brushing, and flossing. | C | 19 |
| All dental fractures should be evaluated with imaging and managed in conjunction with a dental professional. | C | 23 |
| Immediate reimplantation is the preferred treatment for avulsed permanent teeth. | C | 25 |
| Teeth, gums, and oral mucosa should be examined at all child and adult wellness visits. | C | 27 |
| Fluoride varnish should be applied when the first primary tooth comes in, then twice yearly in all infants and young children. | B | 28, 29 |
| Fluoride supplements should be prescribed for children beginning at six months of age if their primary water source is deficient in fluoride. | B | 28–30 |
Dental Anatomy
Primary teeth erupt between six months and two years of age. Normally, four incisors, two canines, and four molars occupy each arch (maxillary and mandibular) and constitute a total of 20 primary teeth. At around six years of age, the primary dentition begins to be replaced by permanent teeth. This process is typically complete by 18 years of age. The typical adult has 32 permanent teeth: four incisors, two canines, four premolars, and six molars in each arch.
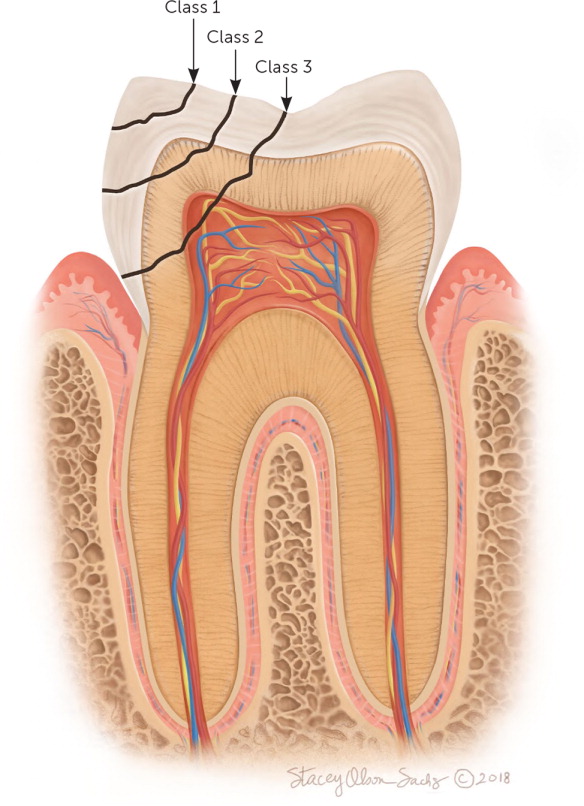
Structurally, each tooth has a crown that is visible above the gingival border. Crown enamel is the hardest structure in the human body. Below the crown is a bony material (dentin) that protects the inner pulp (Figure 1).8 The root of the tooth also has pulp and dentin with an outer layer of cementum. The tooth is held in place at the root by periodontal ligaments that fuse with the alveolar bone of the maxilla and mandible. The apical foramen and pulp canal allow blood vessels and nerves to enter the pulp, supplying nutrition and sensation to each tooth.

Disease Burden
Dental disease is a common cause of medical visits (Table 1).9 In 2010, there were more than two million visits to the emergency department for nonurgent dental problems.10 These largely preventable conditions cost an estimated $2 billion per year.11 In addition to expenditures associated with nonurgent emergency care, annual costs related to hospitalizations for complications of abscessed teeth approach $1 billion.12

| Condition | Definition | Clinical findings | Complications | Treatments |
|---|---|---|---|---|
| Abscess | Localized bacterial infection | Localized pain and swelling | Cellulitis | Incision and drainage, root canal, or extraction |
| Cellulitis | Diffuse bacterial infection of soft tissue | Pain, erythema, and swelling | Regional spread | Antibiotics, root canal, or extraction |
| Irreversible pulpitis | Inflammation of the tooth pulp | Poorly localized pain | Periapical abscess and cellulitis | Root canal or extraction |
| Pericoronitis | Inflamed gum over incompletely erupted tooth | Pain, erythema, and swelling | Cellulitis | Irrigation;antibiotics for concurrent cellulitis |
| Reversible pulpitis | Inflammation of the tooth pulp | Hot/cold sensitivity | Periapical abscess and cellulitis | Filling |
| Tooth avulsion | Missing tooth | Visibly missing | Resorption | Reimplantation or splinting |
| Tooth fracture | Broken tooth | Visible fracture; confirm with radiography | Pulpitis and sequelae | Filling, root canal, or extraction |
| Tooth luxation | Loose tooth | Confirm with radiography | Aspiration, pulpitis, and sequelae | Splinting, root canal, or extraction |
The indirect costs associated with dental disease are enormous. In 2010, an estimated 51 million school hours and 164 million work hours were missed because of dental disease.1 Poor oral health disproportionately affects academic performance in underinsured or uninsured children.13 Lack of access to dental care compounds the problem. Twice as many Americans lack dental insurance compared with those who lack medical insurance. An estimated 74 million Americans had no dental insurance in 2016.14 These patients are more likely to have heart disease, diabetes, and osteoporosis. Conversely, patients who do have dental insurance are more likely to visit a dental professional, take their children to a dental professional, receive recommended preventive screenings and treatments, and have better overall health.
Infection: Dental Caries, Pulpitis, and Abscess
Dental caries is the most common chronic disease world-wide. Acid produced by oral bacteria (primarily Streptococcus mutans) in the biofilm complex adherent to the tooth surface is responsible for the pathogenesis of dental caries. Oral bacteria thrive in the mouth after certain foods and drinks are consumed, particularly those containing sugar. In the presence of sugar, pathogenic bacteria create an acidic environment that fuels the development of a polymicrobial biofilm matrix that damages the tooth surface.15
Early childhood caries is the most common chronic condition in American children.16 It is defined by the presence of at least one decayed, cavitated or noncavitated lesion and a missing or filled tooth (due to caries) in a child younger than six years.17 The incidence of early childhood caries is rising and disproportionately affects children in underserved communities. Early childhood caries affects primary teeth and can progress rapidly. Children who are given bottles of milk, formula, or juice after teeth begin to erupt are more likely to develop early childhood caries.18 This condition is preventable when identified early. Caries initially appears as opaque white spots on the surface of the tooth enamel (Figure 2).9 Progression leads to cavitation (Figure 3).9 If untreated, caries can result in more severe dental infections (e.g., abscess, cellulitis).


In adults, certain illicit and prescription drugs (particularly those that decrease saliva production) increase the risk of enamel erosion and caries formation. Saliva helps remineralize teeth, reduces bacteria on teeth, and raises oral pH by helping to neutralize bacterial acid production. Older patients have decreased saliva production and are more likely to take medications that affect oral health (Table 2).

| Cause of dental disease | Medication |
|---|---|
| Dry mouth | Antidepressants (selective serotonin reuptake inhibitors, tricyclics) |
| Antihistamines | |
| Antihypertensives (atenolol, clonidine, terazosin [Hytrin]) | |
| Antipsychotics | |
| Cannabinoids | |
| Decongestants | |
| Diuretics | |
| Muscle relaxants | |
| Opioids | |
| Protease inhibitors | |
| Proton pump inhibitors | |
| Stimulants for attention-deficit/hyperactivity disorder | |
| Gingival hyperplasia | Calcium channel blockers |
| Immunosuppressive agents | |
| Phenytoin (Dilantin) | |
| Stomatitis/oral inflammation | Chemotherapy |
| Immunosuppressive agents | |
| Inhaled corticosteroids | |
| Sugar-containing medications | Antacids |
| Cough syrups and cough drops | |
| Vitamins |
Initially, dental caries is painless. As the erosion progresses, inflammation and pain can occur, particularly after hot or cold beverages are consumed. Reversible pulpitis occurs when the carious erosion encroaches on the pulp, causing transient pain that resolves spontaneously. Definitive treatment involves removing carious tissue and placing a filling. If untreated, pulpitis becomes irreversible and results in persistent pain requiring a root canal or tooth extraction. Irreversible pulpitis can progress to apical periodontitis, which produces severe and persistent pain that localizes to the affected tooth. Management involves root canal or extraction. If the process continues, inflammation and infection of the tooth apex result in apical periodontitis with abscess formation (Figure 4).19 Incision and drainage is the preferred treatment for dental abscess. Nonsteroidal anti-inflammatory drugs, acetaminophen, and judicious use of opioids are options for pain control. An evaluation by a dental professional is appropriate for any of these conditions. Fever and regional lymphadenopathy are clinical clues to a progressing infection that can involve the fascial planes of the head and neck, representing a true medical emergency if the airway is compromised. If cellulitis or extraoral manifestations are present, antibiotics should be prescribed pending consultation with a subspecialist (Table 3).20


| Antibiotic | Dosage for adults |
|---|---|
| Amoxicillin | 500 mg orally three times per day or 1 g orally two times per day |
| Amoxicillin/clavulanate (Augmentin) | 500/125 mg orally three times per day or 875/125 mg orally two times per day |
| Clindamycin | 300 to 600 mg orally three times per day |
| Penicillin | 1.2 to 2.4 million units per day intramuscularly or intravenously |
| 250 to 500 mg orally four times per day |
Periodontal Disease: Gingivitis, Periodontitis, and Pericoronitis
Nearly one-half of American adults have periodontal disease.1 Periodontal disease has been associated with diabetes, cardiovascular disease, adverse pregnancy outcomes, and ischemic vascular disease.2,21 Risk factors for periodontal disease include smoking, diabetes, human immunodeficiency virus infection, use of certain medications, and genetic susceptibility. Periodontal disease often starts as gingivitis (i.e., inflammation of the gums; Figure 5 and Figure 6).19 Patients typically present with swollen, erythematous gum tissue that bleeds easily with brushing or flossing. Periodontitis occurs when the inflammatory process progresses to the periodontal ligament and, potentially, the supporting alveolar bone. Pericoronitis is a localized infection that occurs within a gingival flap created by a partially erupted tooth or an impacted wisdom tooth.


Gingivitis can be prevented or reversed with regular dental cleaning, proper brushing, and flossing.19 The use of chlorhexidine (Peridex) oral rinse can help reverse gingivitis. Periodontitis is most common in men 30 to 50 years of age. Presenting signs and symptoms typically include halitosis, red and swollen gums that bleed with brushing or flossing, pain with eating, and loose or sensitive teeth. Treatment for periodontitis begins with scaling and root planing to remove plaque and tartar on the tooth and root surfaces. Adding chlorhexidine rinses and antibiotic therapy is an option for managing chronic periodontal disease.19,22 Pericoronitis is treated by removing trapped debris. Use of chlorhexidine oral rinses and referral to a dental professional are indicated if conservative measures are ineffective.
Dental Trauma
Dental trauma is particularly common in children, for whom family physicians are often the initial source of care. One in three children will have an injury to the primary teeth, and one in five 12-year-old children will have an injury to the permanent teeth.23 The Ellis classification system is helpful for characterizing dental fractures, which can involve the crown and/or root of the tooth24 (Figure 7). An accurate history describing the time and mechanism of injury is particularly important when evaluating a dental fracture. All dental fractures should be evaluated with imaging and managed in conjunction with a dental professional.23 Class 1 injuries are limited to the enamel and do not require urgent evaluation. Class 2 injuries extend to the dentin, have hot/cold sensitivity, and should be urgently assessed by a dental professional. Class 3 injuries have exposed pulp and require an urgent root canal.
Dental concussion, luxation, and avulsion are other common dental traumas. With a dental concussion (i.e., trauma without displacement), there is tenderness to percussion with no evidence of fracture or dislocation. Concussion can be managed with pain control, soft diet, and referral to a dental professional.
There are several forms of luxation injuries. With subluxation, the tooth is mobile but not dislodged. Management is the same as for dental concussions. With extrusive luxation, there is a partial avulsion from the alveolar bone. A dental evaluation within 24 hours is recommended. With lateral luxation, there is an alveolar bone fracture requiring immediate splinting. An intrusive luxation “jams” the tooth into the socket. These injuries are associated with an alveolar fracture and require immediate evaluation by an oral and maxillofacial surgeon.
Family physicians are often the first to encounter dental avulsion injuries. Immediate reimplantation is the preferred treatment for avulsed permanent teeth. After one hour, the periodontal ligament cells become nonviable, and reimplantation likely will not succeed.25 If the patient presents immediately after the injury, the tooth should be handled only by the crown, washed briefly in cold water, and promptly repositioned. Biting down gently on a washcloth can help hold the tooth in place after repositioning. If immediate reimplantation is not feasible, the tooth should be placed in pasteurized milk (a clinically recommended storage medium26) and immediate care should be sought from a dental professional.
Prevention: Brushing and Fluoride
Recognizing the importance of oral health in the context of holistic well-being, the Healthy People 2020 guidelines include 17 objectives for oral health27 (eTable A). Prevention is the area in which primary care physicians can have the greatest impact on oral health. Family physicians can incorporate oral health into routine practice through counseling about diet, oral hygiene, smoking cessation, and fluoride supplementation28; application of fluoride varnish; and screening for dental disease. Fluoride varnish should be applied when the first primary tooth erupts, then twice yearly in all infants and young children.28,29 Fluoride supplements should be prescribed for children beginning at six months of age if their primary water source is deficient in fluoride.28-30

| Increase the number of health agencies that have a dental public health program directed by a dental professional with public health training |
| Increase the number of states (including the District of Columbia) that have a system for recording and referring infants and children with cleft lips and cleft palates to craniofacial anomaly rehabilitative teams |
| Increase the number of states (including the District of Columbia) that have an oral and craniofacial health surveillance system |
| Increase the proportion of adults who receive preventive interventions in dental offices |
| Increase the proportion of children, adolescents, and adults who used the oral health care system in the past year |
| Increase the proportion of children and adolescents who have received dental sealants on their molar teeth |
| Increase the proportion of local health departments and FQHCs with an oral health program |
| Increase the proportion of low-income children and adolescents who received preventive dental services during the past year |
| Increase the proportion of oral and pharyngeal cancers detected at the earliest stage |
| Increase the proportion of patients who receive oral health services at FQHCs each year |
| Increase the proportion of school-based health centers with an oral health component |
| Increase the proportion of the U.S. population served by community water systems with optimally fluoridated water |
| Reduce the proportion of adults 45 to 74 years of age with moderate or severe periodontitis |
| Reduce the proportion of adults who have ever had a permanent tooth extracted because of dental caries or periodontal disease |
| Reduce the proportion of adults with untreated dental decay |
| Reduce the proportion of children and adolescents who have dental caries in their primary or permanent teeth |
| Reduce the proportion of children and adolescents with untreated dental decay |
As the first teeth erupt, young children require help from an adult to ensure adequate cleaning. Early use of fluoride toothpaste is an effective preventive measure at this stage.29 Children younger than two years should use a smear of low-fluoride toothpaste, and those two to five years of age should use a pea-sized amount of fluoride toothpaste. Tools are available to help non–dental professionals with caries risk assessment.30 Based on the patient's clinical risk and physical findings, recommended treatments include the use of fluoride toothpaste, professionally applied topical fluoride,31 and pit/fissure sealants.32
Family physicians are well positioned to include routine oral health evaluations as part of their well-child, prenatal, and well-adult examinations.27 Partnering with dental professionals in the context of a patient-centered medical home, as recommended by the American Academy of Family Physicians,33 can also improve care coordination and health outcomes. More information on oral health topics from American Family Physician is available at https://www.aafp.org/afp/oralhealth. The Society of Teachers of Family Medicine offers comprehensive training and an oral health app in its Smiles for Life curriculum at http://www.smilesforlifeoralhealth.org.
This article updates previous articles on this topic by Douglass and Douglass,9 and by Nguyen and Martin.8
Data Sources: A PubMed search was completed using the key terms dental, urgencies, emergencies, oral caries, prevention, oral infection, periodontal disease, and dental trauma. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. We also searched the Cochrane database, Essential Evidence Plus, and updated guidelines from the American Dental Association, the International Association of Dental Traumatology, and the American Academy of Pediatric Dentistry. Search dates: August 15, 2016, to July 17, 2018.
