
Am Fam Physician. 2020;101(1):19-23
Author disclosure: No relevant financial affiliations.
Adolescent idiopathic scoliosis affects 1% to 3% of U.S. adolescents. It is defined by a lateral curvature of the spine (Cobb angle) of at least 10 degrees in the absence of underlying congenital or neuromuscular abnormalities. Adolescent idiopathic scoliosis may be detected via the forward bend test and should be confirmed with scoliometer measurement. Mild scoliosis is usually asymptomatic; it may contribute to musculoskeletal back pain, but there is no evidence that it causes disability or functional impairment. Patients with severe scoliosis (Cobb angle of 40 degrees or more) may have physical pain, cosmetic deformity, psychosocial distress, or, rarely, pulmonary disorders. Several studies have shown modest benefit from bracing and scoliosis-specific physical therapy to limit progression in mild to moderate scoliosis, but there were no effects on quality of life. Because no high-quality studies have proven that surgery is superior to bracing or observation, it should be reserved for severe cases. There is little evidence that treatments improve patient-oriented outcomes. The U.S. Preventive Services Task Force and the American Academy of Family Physicians found insufficient evidence to assess the balance of benefits and harms of screening for adolescent idiopathic scoliosis in children and adolescents 10 to 18 years of age.
Adolescent idiopathic scoliosis is a lateral curvature of the spine (i.e., the Cobb angle) of 10 degrees or more that affects adolescents 10 to 18 years of age. It is the most common form of scoliosis and is distinguished from other types of scoliosis by the absence of underlying congenital or neuromuscular abnormalities. Approximately 1% to 3% of adolescents in the United States are affected.1 The incidence is similar between males and females. However, females are 10 times more likely to progress to Cobb angles of 30 degrees or more.1,2 Genetic factors are thought to contribute to the development of scoliosis, but inheritance patterns are variable, and no single mode of genetic transmission has been identified.2 There is no role for genetic testing in the screening and management of adolescent idiopathic scoliosis.
| Clinical recommendation | Evidence rating | Comment |
|---|---|---|
| The U.S. Preventive Services Task Force and the American Academy of Family Physicians concluded that evidence is insufficient to assess the balance of benefits and harms of screening for adolescent idiopathic scoliosis in adolescents 10 to 18 years of age.2,3 | C | Insufficient evidence that screening improves patient-oriented outcomes |
| A scoliometer measurement of 5 degrees or more requires radiologic evaluation for Cobb angle measurement, especially in overweight or obese patients.6,12–14 | C | Expert opinion and consensus guidelines in the absence of scoliosis screening clinical trials |
| Bracing and scoliosis-specific physical therapy may be effective for slowing progression of skeletal curvature.18,19,21 | C | Limited number of studies with disease-oriented outcomes |
What Is the Clinical Significance of Adolescent Idiopathic Scoliosis?
Although most patients with adolescent idiopathic scoliosis are asymptomatic, a small minority develop clinical symptoms such as physical discomfort and respiratory compromise with social and psychological consequences such as cosmetic deformity and psychological distress, all of which can reduce quality of life.
EVIDENCE SUMMARY
Most patients with adolescent idiopathic scoliosis will not develop clinical symptoms in their lifetime. Back pain is more common among those with scoliosis; however, it does not result in disability or functional impairment. Curve magnitude does not correlate with back pain severity. Mortality is similar between patients with adolescent idiopathic scoliosis and the general population.3
A minority of patients who have greater curve angles will develop substantial rib deformities, leading to more serious disease later in life. Clinically significant disease is more likely to occur at a Cobb angle of 40 degrees or more.3,4 The incidence of spinal curvature greater than 40 degrees is 0.4% among adolescents 10 to 16 years of age.1 Those with progressive scoliosis may have physical pain, cosmetic deformity, and respiratory difficulties ranging from subjective shortness of breath to pulmonary disorders with measurably impaired lung function. These diseases are accompanied by other adverse effects, including social and psychological distress, financial cost, and reduced quality of life.2,3
Should Children Be Screened?
EVIDENCE SUMMARY
The USPSTF found adequate evidence that adolescent idiopathic scoliosis can be accurately detected in asymptomatic adolescents using three screening techniques: the forward bend test, scoliometer measurement, and Moiré topography. Although bracing may slow curve progression in mild to moderate scoliosis, there is insufficient evidence that early detection and treatment improve health outcomes. No published studies have investigated the direct harms of screening or interventions.3
Because curve progression occurs primarily with skeletal growth during adolescence, proponents of screening have argued that early detection and treatment could slow curve progression before skeletal maturity and improve long-term health outcomes.3,4 This was the rationale for nationwide school-based scoliosis screening programs for decades. However, in 2004 the USPSTF and AAFP recommended against routine screenings, citing a lack of evidence that benefits exceed potential harms, including exposure of low-risk adolescents to unnecessary radiography, referrals, and bracing.5 Other professional organizations, including the American Academy of Orthopedic Surgeons, the Scoliosis Research Society, the Pediatric Orthopedic Society of North America, and the American Academy of Pediatrics, support routine screenings, arguing that early detection improves the chances of effective nonsurgical management and citing the relatively low cost and minimal radiation risk associated with screening. They suggest screening females twice, at 10 and 12 years of age, and males once at 13 to 14 years of age.6
How Useful Is Physical Examination in Detecting Clinically Significant Scoliosis?
Scoliosis is often brought to the attention of clinicians by the patient, caregivers, or school-based screening programs. Clinical examination including the forward bend test and use of a scoliometer can reliably determine which patients require further evaluation or referral.
EVIDENCE SUMMARY
Patients with adolescent idiopathic scoliosis are typically identified through school-based screening programs or when the patient, caregivers, or clinicians notice a curve or asymmetry (e.g., asymmetric breasts, chest wall, shoulders, or back). There are no reliable physical symptoms of scoliosis. Significant back pain is uncommon except in severe disease and should cause the examiner to suspect alternative diagnoses such as infection, inflammation, or neoplasm.2 Restrictive or obstructive pulmonary disease can result from severe scoliosis but will not likely be the cause for presentation. Clinical examination can identify patients who require imaging for calculation of the Cobb angle or for follow-up.
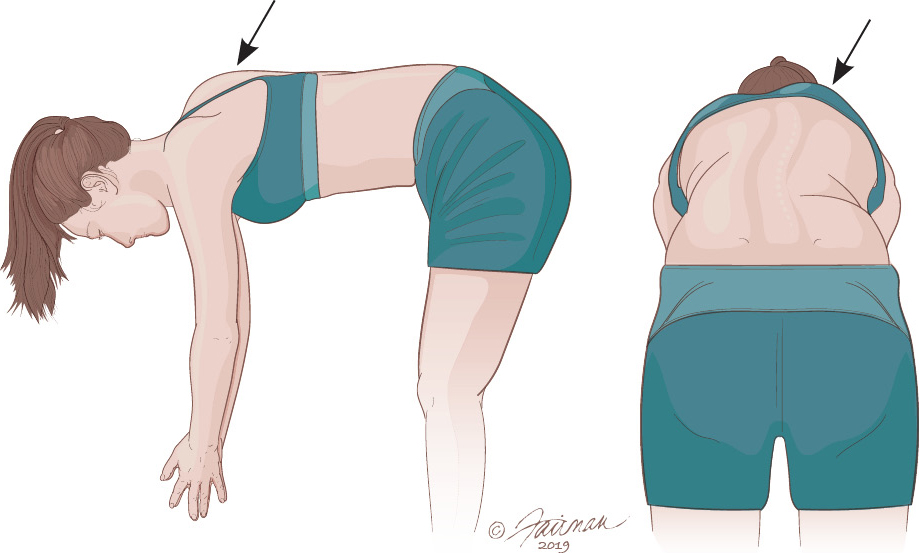
The most common method to screen for significant scoliosis is the forward bend test, which is often combined with the use of a scoliometer or Moiré topography. To perform the test, the patient stands upright while the examiner observes from behind for any obvious curvature (Figure 1).7 The patient is then asked to bend forward to bring the spine parallel with the floor, with the arms dangling, palms together, and knees forward, while the examiner inspects from behind for any thoracic or lumbar prominence that would signify scoliosis. The test has a sensitivity of 92% to 100% for thoracic scoliosis in patients with a Cobb angle of more than 20 degrees.8 It is less reliable for lumbar scoliosis. A scoliometer is typically used if curvature is suspected, and it can be useful to determine whether to order radiography for a definitive diagnosis. A scoliometer is used to measure the angle of trunk rotation. This measurement can then be used to estimate the more accurate Cobb angle, which is measured via radiography. A scoliometer is similar to a carpenter’s level and is available as a hand-held device or smartphone app9–11 (Figure 22).
The cutoffs at which radiography is ordered vary from 5 to 7 degrees of trunk rotation via scoliometer.6,12–14 The translation of scoliometer rotation to Cobb angle is not exact; in normal-weight patients a 7-degree angle of trunk rotation corresponds to a Cobb angle of approximately 20 degrees. The sensitivity and specificity of the scoliometer are about 83% and 87%, respectively, using a cutoff of 7 degrees of trunk rotation for a Cobb angle greater than 10 degrees; the sensitivity rises to 100% when a threshold of 5 degrees is used, but the specificity falls to 47%.15 The lower cutoff of 5 degrees of trunk rotation should be used in patients with body mass index in the 85th percentile or more.13 Radiography should be ordered for any adolescent with an obvious curve on physical examination or with readily apparent thoracic or lumbar asymmetry in those with a family history of scoliosis, and for monitoring of progression in patients who have been previously diagnosed.16

Moiré topography involves a specialized machine that projects a topographic image onto a person’s back to detect variation between the right and left sides.3 It is not commonly used for scoliosis screening in the United States.
What Examination and/or Radiologic Findings Warrant Referral?
Surgical referral is generally recommended for patients with a Cobb angle of at least 40 degrees. Those with lesser curvatures can be monitored unless there are signs or symptoms suggesting an alternative diagnosis.
EVIDENCE SUMMARY
No evidence-based guidelines exist to help determine which patients require orthopedic referral for adolescent idiopathic scoliosis. Referral should be considered for those with severe scoliosis or curvature and musculoskeletal symptoms suggestive of an alternative diagnosis. In general, few referrals are made because of a lack of evidence that treatment affects long-term outcomes, except in severe cases.
Referral for surgery and/or bracing is indicated when the initial Cobb angle is 40 degrees or more.2 Observation is generally recommended for patients with an initial Cobb angle less than 20 degrees, although referral for physical therapy may be appropriate.3 Patients with a smaller Cobb angle and risk factors for progression may also benefit from referral or close observation. Younger age at presentation (especially younger than 12 years), female sex, family history of clinically significant scoliosis, and relative skeletal immaturity are risk factors for progression.2,14,17 Skeletal maturity is generally estimated through radiography of the pelvis to obtain the Risser grade. Grading is based on the degree of iliac apophysis ossification, from grade 0 (no ossification) to grade 5 (complete bony fusion). Lower grades indicate more growth potential and greater risk of curve progression.2,3,14 At smaller degrees of curvature, radiographic monitoring for progression every six months is warranted, and referral is indicated if the angle increases2,14 (Table 17). Magnetic resonance imaging should be considered if alternative diagnoses such as malignancy are in the differential.
| Cobb angle (degrees) | Radiography | Treatment |
|---|---|---|
| 10 to 19 | Every six months | Observe |
| 20 to 29 | Every six months with Risser grading | Refer for consideration of bracing and physical therapy, especially at Risser grade 0 or 1* |
| 30 to 39 | — | Refer for bracing and/or physical therapy |
| ≥ 40 | — | Refer for surgery |
What Treatments Are Effective?
Several recent studies show that bracing and scoliosis-specific physical therapy provide modest benefit in limiting Cobb angle progression in patients with adolescent idiopathic scoliosis; spinal surgery remains poorly studied. It is unclear whether any treatment mitigates symptom progression into adulthood or improves long-term quality of life.
EVIDENCE SUMMARY
Treatment of adolescent idiopathic scoliosis aims to reverse, stop, or limit further spinal curvature, and thus, prevent or mitigate symptoms. Management options include observation, physical modalities (e.g., bracing, physical therapy), and surgery.18 The 2013 Bracing in Adolescent Idiopathic Scoliosis Trial included 242 participants across 25 U.S. centers; it was stopped early when interim results showed that bracing can significantly slow mild to moderate curvature progression.19 More than 70% of participants who wore braces experienced treatment success, defined as an end point Cobb angle less than 50 degrees, compared with only 48% of the observation group. This translates to a relative risk reduction of 56% and a number needed to treat of 3 to prevent one case of progression warranting surgery over approximately two years. There was no difference in quality of life among those treated with bracing vs. observation; of note, 8% of participants in the bracing group had adverse effects involving the skin, or a number needed to harm of 12 for an intervention that did not clearly improve patient-oriented outcomes. Other potential harms of bracing include body pain, physical limitations, anxiety, and depression.18
Although a Cochrane review of studies before 2012 showed no benefit for physical therapy in adolescent idiopathic scoliosis,20 a 2013 randomized controlled trial found modest benefits from scoliosis-specific therapy.21 An Italian study of 110 patients with mild adolescent idiopathic scoliosis (Cobb angle less than 25 degrees) showed that those in the scoliosis-specific and task-oriented exercise group (who were taught and encouraged to make active self-corrections in everyday life) maintained an average Cobb angle decrease of 4.9 degrees 12 months posttreatment, whereas the control group (who completed typical physiotherapy) had an average Cobb angle increase of 2.8 degrees.21 The treatment group also reported better function, mental health, pain, and self-perceived image at the conclusion of treatment (average: 42 months) and at the 12-month follow-up.
Surgery remains an option for severe adolescent idiopathic scoliosis, but it has been poorly studied and has not been proven superior to bracing, even for severe scoliosis.22 No prospective controlled studies have compared surgical intervention with observation.22 Surgery has significant risks, including bleeding, infection, nerve damage, and death.22
It is unclear whether aggressive surgical intervention or modest changes in Cobb angle with physical modalities provide long-term symptom relief and improved quality of life. In multiple studies of middle-aged adults who were treated with bracing vs. surgery during adolescence, there was no difference in quality of life in adulthood between the two groups.3,23
This article updates previous articles on this topic by Horne, et al.2 ; Reamy and Slakey7 ; and Greiner.24
Data Sources: We began with an initial evidence summary that included relevant POEMs, Cochrane reviews, evidence-based guidelines, and other items from Essential Evidence Plus. A PubMed search was then done using the key terms scoliosis, idiopathic scoliosis, adolescents, children, and pediatrics. Articles referenced in the 2018 U.S. Preventive Services Task Force recommendation statement on screening for adolescent idiopathic scoliosis were reviewed. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality evidence reports, the National Guideline Clearinghouse database, and UpToDate. Search dates: November 2018 to August 2019.
