Center for Diversity and Health Equity
You need to know how to identify and address social determinants of health to improve health outcomes for your patients and vulnerable populations in your community.
The results of an AAFP member survey indicate that while 85% of surveyed physicians believe social needs are directly related to poor health, 80% are not confident in their ability to address their patients' social needs. In response to this need and a AAFP Congress of Delegates resolution, the AAFP formed the Center for Diversity and Health Equity to address social determinants of health with The EveryONE Project.
The EveryONE Project aims to address social determinants of health by:
- Providing AAFP members with education and information about health equity.
- Identifying and developing clinical tools and resources to address patients’ social needs.
- Supporting research and policy development.
- Advocating for policies that encourage health equity.
- Encouraging workforce diversity.
- Serving as a resource center for AAFP members.
Striving for Health Equity
Due to their comprehensive training, family physicians are uniquely qualified to care for people of all ages—newborns to seniors. They provide the majority of health care for underserved rural and urban populations in the U.S., and treat a more diverse population of patients than any other medical specialty. This often places family physicians as leaders in their communities. As leaders, family physicians have an important role to raise awareness about health disparities and help patients address social and economic drivers of health inequities.
The AAFP has a long history of supporting health equity and reducing health disparities in patient care. One of the AAFP’s key strategic objectives is to “take a leadership role in addressing diversity and social determinants of health as they impact individuals, families, and communities across the lifespan and to strive for health equity.” The EveryONE Project is our vehicle to help achieve this objective.
In this presentation, Jason Glenn, PhD, Associate Professor of History and Philosophy of Medicine at the University of Kansas Medical Center discusses examples of medical experimentation on and exploitation of enslaved people and minoritized communities throughout history, and the impact this has had on the health inequities and disparities we see today.
Presented by Dr. Ada Stewart, former Board Chair of the American Academy of Family Physicians and Chair of the AAFP Commission on Diversity, Equity, and Inclusiveness in Family Medicine, this 19-minute video offers an overview of AAFP’s definitions and policies related to diversity, equity, inclusion, and anti-racism. At the time of this recording, Dr. Stewart was the Board Chair of the AAFP. Her term ended in September 2022.

AAFP has a long history of supporting health equity in patient care. But we can’t affect change without also recognizing racial equity as a root cause.
There's still work to do. During national observances, we honor our diverse family physicians, medical students and AAFP staff, and share resources that support health equity efforts.
“If we want to ensure all patients have access to optimal health, we need to make sure we are reaching everyone, and that sometimes means approaching conversations differently or even challenging our (possibly untrue) beliefs.”
- Margot Savoy, M.D.
Martin Luther King Day (Jan. 18)
The AAFP celebrates the important work of Dr. Martin Luther King, Jr., to advance civil rights and dismantle racism, a significant contributor to health inequities and poor patient outcomes. Healthy communities can only exist when there’s an awareness of the underlying issues and efforts to change systems that harm the health minority populations.
Black History Month (February)
Throughout this month, we'll celebrate the accomplishments of Black AAFP members working to improve health outcomes for all communities. We highlight AAFP.org and external resources for family physicians and patients regarding minority health, health equity and social determinants of health to equip members with practical tools and information.
National Minority Health Month (April)
This observance is an opportunity to elevate AAFP member voices and discuss issues that negatively impact patient health. Includes a focus on Black Maternal Health Week.
Asian American Pacific Islander Month (May)
During this observance, we highlight and celebrate the achievements and contributions of our Asian American, Native Hawaiian and Pacific Islander members. We’ll also feature tools and resources to help members promote health equity and provide culturally and linguistically appropriate services.
Pride Month (June)
During Pride Month, the AAFP celebrates the courage of the LGBTQ community, recognizes members who are creating practices that support LGBTQ patients, and advocates for LGBTQ persons to have equal health care rights.
Women in Medicine Month (September)
This month and throughout the year, we celebrate the contributions women have made to the field of medicine and we support them by providing leadership opportunities and advocating for equal pay and fair representation.
Hispanic and Latino Heritage Month (Sept. 15-Oct. 15)
During HLHM, the AAFP honors and celebrates the achievements and contributions of family physicians whose ancestors came from Mexico, the Caribbean, Central and South America, and Spain.
Native American Heritage Month (Nov.)
During NAH, the AAFP highlights health issues and disparities that American Indians/Alaska Natives experience, and links members to resources that can support care for this minority patient population.
.
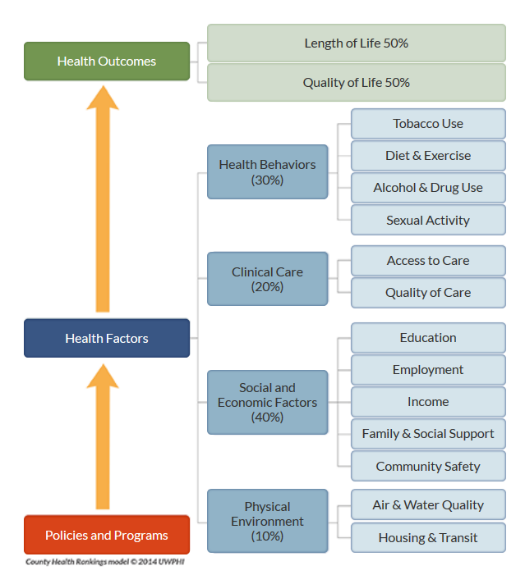
University of Wisconsin Population Health Institute. County Health Rankings & Roadmaps 2017.
The County Health Rankings & Roadmaps, a program of the Robert Wood Johnson Foundation, ranks the health of nearly every county in the U.S. They identify four classifications of health factors: health behaviors, clinical care, social and economic factors, and physical environment. Based on the group’s methodology, as well as previous research, each health factor is weighted1 and shown with activities and specific factors that contribute to social determinants of health.2 According to the County Health Rankings & Roadmaps, factors such as health behaviors (30%), clinical care (20%), social and economic factors (40%), and physical environment (10%) are attributed to SDOH.
Race, gender, and geography are not implicit in the County Health Rankings & Roadmaps model, but also impact health outcomes through discrimination and social stratification, and as a result, impact life expectancy rates. Gaps in life expectancy are evident among racial and ethnic groups, as well as between genders and by education level.3
Additionally, a nearly 20-year gap exists in life expectancy at birth between counties with the highest and lowest life expectancy rates.4
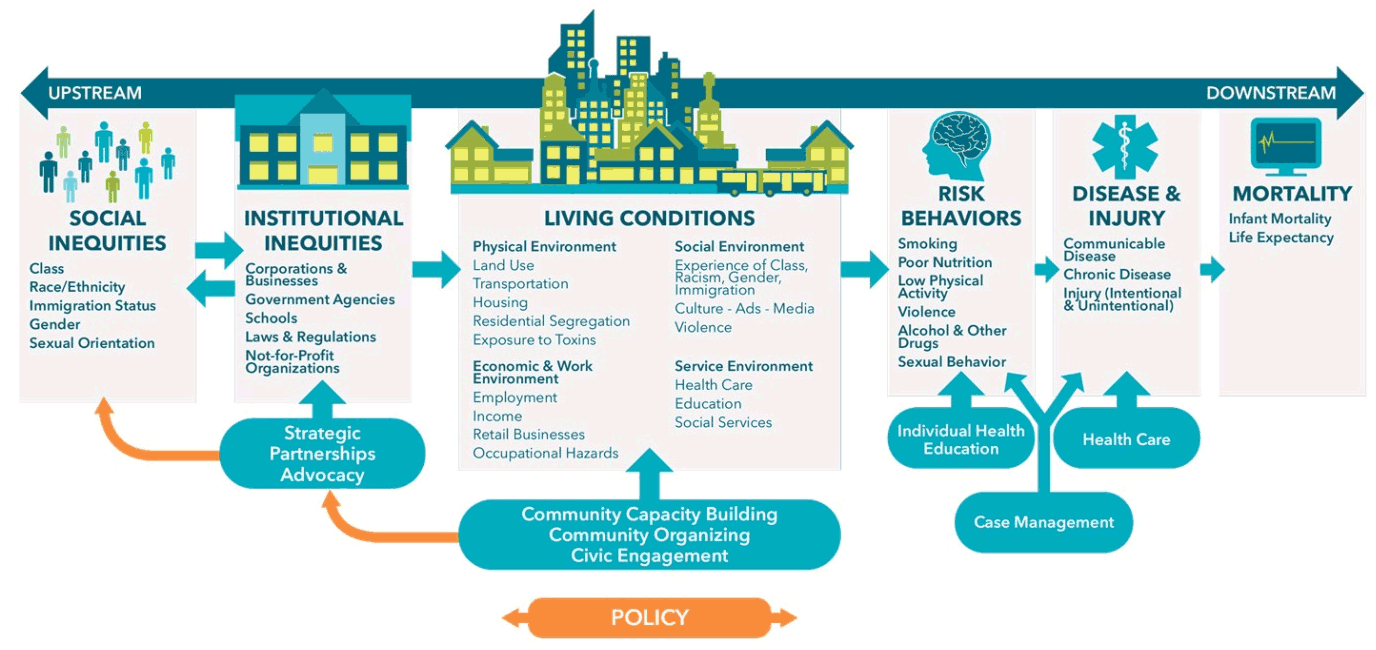
Public Health Framework for Reducing Health Inequities
Used with permission from the Bay Area Regional Health Inequities Initiative (BARHII)
A complex system of political, economic, social, behavioral, and medical factors influence health equity. Health equity scholars use an analogy of a stream of causation to describe this system. Upstream factors refer to underlying root causes of health inequities, such as the structural socioeconomic and political environments that leads to social stratification.5 Downstream factors refer to those factors that are nearer to where health outcomes are observed, such as behavior and disease.5 This upstream and downstream continuum reflects key factors that determine health outcomes.6
Achieving health equity requires actions to address both upstream and downstream factors. Upstream interventions are more population-based in nature and include actions such as advocacy, policy change, and community empowerment. Downstream interventions are more individual in nature and include actions such as education, healthy behaviors, and access to health care.6
The AAFP recognizes the complexity of these systems and the challenges our members face in helping their patients address their individual health factors. Additionally, the new Medicare payment model, the Quality Payment Program (QPP), focuses Medicare payments on measuring the quality of care you provide more than ever before. Understanding the SDOH of your patient population and helping them address factors that improve health outcomes is imperative to your patients’ overall health and potentially your bottom line.
Partner With Us
The AAFP has identified four strategic priorities that will guide our work for The EveryONE Project. We’d like to hear from you about what interests you. If you are interested in any of these issues, or learning more about health equity, please email The EveryONE Project at healthequity@aafp.org.
References
- Booske BC, Athens JK, Kindig DA, Park H, Remington PL. Different perspectives for assigning weights to determinants of health. 2010. University of Wisconsin Population Health Institute. Accessed February 27, 2018.
- County Health Rankings and Roadmaps. What and why we rank. Accessed February 27, 2018.
- Health Affairs. Health policy brief. Health gaps. Accessed February 27, 2018.
- Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Inequalities in life expectancy among US counties, 1980 to 2014. Temporal trends and key drivers. JAMA Intern Med. 2017;177(7): 1003-1011.
- Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl 2):19-31.
- Public Health Framework for Reducing Health Inequities. Used with permission from the Bay Area Regional Health Inequities Initiative (BARHII). Accessed October 13, 2020.
The Center for Diversity and Health Equity is supported in part by a grant from the AAFP Foundation.