
Am Fam Physician. 2022;106(2):195-196
Author disclosure: No relevant financial relationships.
A 16-year-old patient presented with right thigh pain that began three weeks earlier after he was injured in a lacrosse game. He was involved in a collision, with direct trauma to his right thigh, but was able to complete the game. The pain gradually increased over the next few weeks, and he noticed a new palpable mass within the anterolateral thigh.
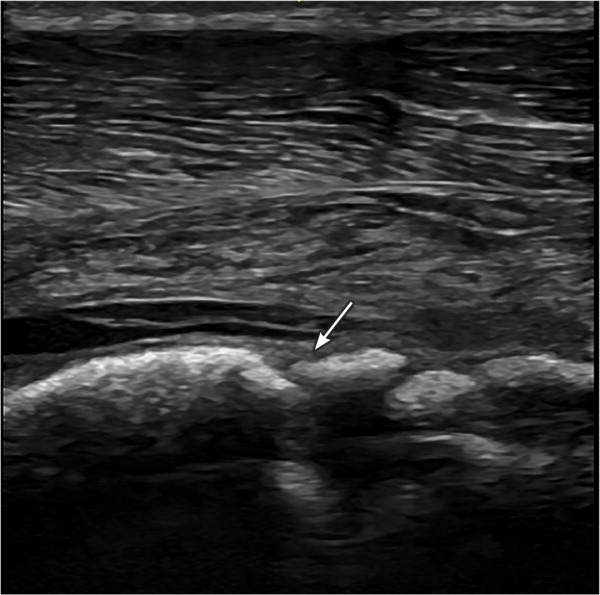
On examination, a firm, tender mass was palpated over the lateral quadriceps. The patient had pain on knee flexion, and range of motion was limited to 100 degrees. No overlying skin changes or gross deformities were present. Point-of-care ultrasonography was performed, followed by radiography (Figure 1 and Figure 2).


Question
Based on the patient's history, physical examination, and imaging findings, which one of the following is the most likely diagnosis?
A. Ewing sarcoma.
B. Femoral stress fracture.
C. Myositis ossificans.
D. Osteosarcoma.
Discussion
The answer is C: myositis ossificans. Myositis ossificans, also known as posttraumatic heterotopic ossification, is a nonmalignant ossification of soft tissue structures, usually the quadriceps, brachialis, and adductor muscles.1 The condition commonly occurs in athletes following an injury but may also occur after surgery. Myositis ossificans is believed to result from inflammation-induced differentiation of fibroblasts into osteoblasts.1
Myositis ossificans presents as localized muscle pain that lasts longer than would be expected with a contusion or muscle strain. The condition is associated with decreased range of motion in the adjacent joint and stiffness with motion in the affected joint. Presentation may be delayed because pain and range of motion worsen during osteoblastic transformation about two to four weeks after injury.1,2
Radiography can identify myositis ossificans at three to four weeks.1 Magnetic resonance imaging is considered the diagnostic standard, but ultrasonography is emerging as a preferred modality (Figure 3) because of low cost, ease of use, safety profile, and earlier diagnosis.3 Treatment of myositis ossificans includes cryotherapy and early activity restriction. Clinicians should encourage gentle, static stretching beginning no earlier than 48 hours postinjury.4 Acetaminophen is initially preferred over nonsteroidal anti-inflammatory drugs to avoid bleeding risk. Surgery may be considered if lesions persist beyond six to 12 months.2
| Condition | Radiograph findings | Ultrasound findings |
|---|---|---|
| Ewing sarcoma | Lytic lesions, aggressive periosteal reaction; lamellated or “onion skin” appearance, cortical disruption, soft tissue masses | Uneven disruption of osseous structures; heterogeneous, hypoechoic mass directly adjacent to bone |
| Stress fracture | Metaphyseal sunburst appearance, periosteal lifting | Early: hypoechoic, hypervascular cortical rim with surrounding edema; late: cortical disruption or callus formation |
| Myositis ossificans | Early: faintcalcification; late: progression to diffuse soft tissue calcification | Superficial, hyperechoic layer distinct from underlying bone (Figure 3; may be absent in acute phase) |
| Osteosarcoma | Metaphyseal sunburst appearance, periosteal lifting | Subperiosteal heterogeneous echogenicity with hyperechoic calcifications perpendicular to bone diaphysis; disorganized hypervascularization in lesion periphery |
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Uniformed Services University of the Health Sciences, the U.S. Army Medical Department, or the U.S. Army and U.S. Air Force at large.
