
Am Fam Physician. 2023;107(1):35-41
Related letter to the editor: Removal of Stones and Food for Relief of Pain and Recurrence of Tonsillitis
Patient information: See related handouts on tonsillitis (strep throat) and tonsil stones.
Author disclosure: No relevant financial relationships.
Tonsillitis, or inflammation of the tonsils, makes up approximately 0.4% of outpatient visits in the United States. Tonsillitis is caused by a viral infection in 70% to 95% of cases. However, bacterial infections caused by group A beta-hemolytic streptococcus (Streptococcus pyogenes) account for tonsillitis in 5% to 15% of adults and 15% to 30% of patients five to 15 years of age. It is important to differentiate group A beta-hemolytic streptococcus from other bacterial or viral causes of pharyngitis and tonsillitis because of the risk of progression to more systemic complications such as abscess, acute glomerulonephritis, rheumatic fever, and scarlet fever after infection with group A beta-hemolytic streptococcus. A variety of diagnostic tools are available, including symptom-based validated scoring systems (e.g., Centor score), and oropharyngeal and serum laboratory testing. Treatment is focused on supportive care, and if group A beta-hemolytic streptococcus is identified, penicillin should be used as the first-line antibiotic. In cases of recurrent tonsillitis, watchful waiting is strongly recommended if there have been less than seven episodes in the past year, less than five episodes per year for the past two years, or less than three episodes per year for the past three years. Tonsilloliths, or tonsil stones, are managed expectantly, and small tonsilloliths are common clinical findings. Rarely, surgical intervention is required if they become too large to pass on their own.
Tonsillitis, or inflammation of the tonsils, makes up approximately 0.4% of outpatient visits in the United States and is usually caused by a viral infection.1–3 Transmission occurs via droplets from patients with acute tonsillitis or rarely by asymptomatic carriers.3 Tonsilloliths, or tonsil stones, may be a result of recurrent tonsillitis, although the exact cause is unclear.
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| A clinical scoring scale, such as the Centor score, could be used in the initial evaluation of pharyngitis and tonsillitis symptoms; rapid antigen detection testing can be considered in patients with a score of 2 or more.8–12 | A | Meta-analysis and validated clinical decision rule |
| Antibiotics are recommended for group A beta-hemolytic streptococcus pharyngitis, and penicillin is the first-line agent.13,23–25 | A | Infectious Diseases Society of America clinical guidelines and meta-analysis |
| Watchful waiting is typically preferred over tonsillectomy for recurrent tonsillitis if there have been less than seven episodes in the past year, less than five episodes per year in the past two years, or less than three episodes per year in the past three years.30,32 | A | Systematic review and clinical practice guideline |
Tonsillitis
The tonsils are located in the lateral oropharynx between the anterior palatoglossal arch and the posterior palatopharyngeal arch. Tonsillitis is caused by a viral infection in 70% to 95% of cases.2,3 The most common viral causes include rhinovirus, respiratory syncytial virus, adenovirus, and coronavirus. Less common causes include Epstein-Barr virus, cytomegalovirus, hepatitis A, and rubella. Bacterial infections caused by group A beta-hemolytic streptococcus (GABHS) account for tonsillitis in 5% to 15% of adults and 15% to 30% of patients five to 15 years of age. Viral etiologies are more common in children younger than five years, and GABHS is rare in children younger than two years.2
Tonsillitis is less commonly caused by other bacteria such as groups C and G streptococci, Hemophilus influenzae, Nocardia, and Corynebacteriaceae.3 Syphilis, gonorrhea, chlamydia, and HIV should be considered in sexually active patients. Tuberculosis can cause recurrent tonsillitis.2 Only one-half to two-thirds of patients with tonsillitis have a detectable pathogen.3
CLINICAL MANIFESTATIONS
Acute tonsillitis is an inflammatory process of the tonsillar tissues. It may occur in isolation or as part of a generalized pharyngitis.4 The most common symptoms are fever, tonsillar exudate, sore throat, and tender anterior cervical lymphadenopathy5 (Figure 16). Other symptoms include odynophagia and dysphagia, particularly if tonsillar swelling is present. On physical examination, the tonsils may appear enlarged or erythematous, decreasing visualization of the posterior oropharynx. Tonsillar exudate can appear yellow or white.2 Data have shown that palatal petechiae are associated with GABHS pharyngitis and tonsillitis and are possibly more predictive than the presence of tonsillar exudate.7

DIAGNOSIS
The differential diagnosis of tonsillitis includes pharyngitis, retropharyngeal abscess, epiglottitis, peritonsillar abscess, and submandibular space infections (Ludwig angina).2 It is important to differentiate GABHS pharyngitis and tonsillitis from other bacterial and viral causes due to the risk of complications with GABHS.4 Physical examination of the oropharynx alone is not sufficient for this differentiation; therefore, a clinical scoring scale, such as the widely used Centor score (Table 18,9), is recommended to guide diagnosis and treatment of GABHS oropharyngeal infections.
| Symptoms | Points |
|---|---|
| Tonsillar exudate or swelling | 1 |
| Swollen, tender anterior cervical lymph nodes | 1 |
| Lack of cough | 1 |
| Fever | 1 |
| Total: | __________ |
The Centor score was developed in 1981 based on a study of 286 adults from a single emergency department.8,10 A second clinical scoring system, the McIsaac score/modified Centor score (https://www.mdcalc.com/centor-score-modified-mcisaac-strep-pharyngitis) was developed in 1998 based on 621 children and adults from 49 Ontario, Canada, communities.8 This score adds an adjustment for the patient's age because GABHS infections are more prevalent in younger patients. Because the initial sample sizes supporting these scores were small, both scoring systems underwent large-scale validation.8 A meta-analysis comparing the two scoring systems in a primary care setting found that they were similar in performance.9
The Centor score is helpful in ruling out streptococcal pharyngitis and has limited positive predictive value for determining when GABHS infection is present.9 In a guideline published in 2001, the American College of Physicians and Centers for Disease Control and Prevention recommended no further testing or treatment for a Centor score of 0 or 1.11 Based on these guidelines, rapid antigen detection testing may be considered for patients who have a score of 2, treating only individuals who test positive. Two possible strategies are recommended for scores of 3 and 4: perform rapid antigen detection testing and treat only patients who have positive results or initiate empiric antibiotics without further testing. The 2016 American College of Physicians and the Centers for Disease Control and Prevention guidelines for the treatment of acute respiratory infections do not recommend further testing for patients who meet fewer than 3 Centor criteria.12
The 2012 Infectious Diseases Society of America (IDSA) guidelines recommend antibiotic treatment only for patients with a positive rapid antigen detection test result.13 This echoes the concern from a recent meta-analysis that empiric treatment with antibiotics for patients with a Centor score of 3 or more may lead to overprescribing in a high percentage of patients.9
There are several laboratory tests that may be used in the evaluation of pharyngitis and tonsillitis to help differentiate GABHS infection from other causes. Rapid antigen detection testing has three features that make it the recommended first-line test for detecting GABHS infection. It is inexpensive (about $1 to $2 per test), easy to perform without specialized training, and rapid (results are typically available in less than 10 minutes).13,14 The test uses swab samples collected from the tonsils and posterior oropharynx. There are three types of rapid antigen detection tests: latex agglutination, enzyme immunoassay, and optical immunoassay.15 Latex agglutination tests were the first to be developed but are no longer used in clinical practice because of low sensitivity and poorly defined end points.13,15 Enzyme immunoassays are second-generation tests and the most widely used in clinical practice. Optical immunoassays are third-generation tests and more sensitive than enzyme immunoassays, but their use is limited because of cost.15 Rapid antigen detection tests are specific (88% to 100%), but sensitivities vary widely across studies (61% to 99%), and false-negative results are possible.4,15
A throat culture is considered the diagnostic standard for GABHS tonsillitis.16,17 This test is performed using a swab of the posterior oropharynx and tonsils. The swabbed specimen is then cultured, typically on a 5% sheep blood agar plate. A culture allows for identification of other pathogens and testing for antibiotic sensitivity if there is concern for organism resistance. Disadvantages of throat culture are the time frame to receive results (typically within 24 to 48 hours), which could lead to a delay in diagnosis and treatment, and the inability to differentiate between a new, active infection and a carrier state.16 Based on the most recent IDSA guidelines, a back-up culture after a negative rapid antigen detection test result should be performed in children and adolescents (i.e., five to 15 years of age) but is not required for adults because of the lower incidence of GABHS pharyngitis and exceptionally low risk of rheumatic fever in the adult population.13
Nucleic acid amplification tests can also be used to diagnose GABHS infections. They detect nucleic acid sequences that are specific to GABHS. Although nucleic acid amplification tests have higher sensitivity than rapid antigen detection testing, the high cost (approximately $70 per test) precludes widespread use as a replacement for throat culture.16
Antistreptococcal antibody titers, which are obtained from a peripheral blood sample, are another diagnostic approach. Antistreptolysin O and anti-deoxyribonuclease B (anti-DNase B) titers are most commonly used. Measurement of these titers is appropriate for diagnosis of a recent streptococcal infection in patients presenting with signs and symptoms that are concerning for poststreptococcal complications, such as rheumatic fever or poststreptococcal glomerulonephritis, but these complications are rare in the developed world.17 Antistreptolysin O and anti-DNase B titers do not begin to increase until at least one week after acute streptococcal infection and peak around three to six weeks and six to eight weeks, respectively. The World Health Organization and IDSA guidelines emphasize that antistreptococcal titers, including antistreptolysin O and anti-DNase B antibodies, are not recommended for the initial diagnosis of acute pharyngitis.13,17
In patients with more severe infection, including those with unstable vital signs, toxic appearance, difficulty swallowing, inability to tolerate oral intake, or trismus, imaging may be required.2 Contrast-enhanced computed tomography is the preferred imaging modality to evaluate for serious complications such as abscesses, epiglottitis, or Lemierre syndrome (a rare complication of tonsillitis with septic thrombophlebitis of the tonsillar and internal jugular veins).
TREATMENT
Acute tonsillitis is usually a self-limited disease and rarely results in hospitalization.18 Because acute tonsillitis is often caused by viruses, treatment is primarily supportive, including analgesia with medications such as nonsteroidal anti-inflammatory drugs and maintaining hydration.19 Corticosteroids have been shown to decrease pain scores and improve time to recovery and therefore can be considered as another therapeutic option. If corticosteroids are given, a single dose of dexamethasone administered intramuscularly or orally is the preferred regimen (10 mg for adults; 0.6 mg per kg, maximum 10 mg, for children).20 Studies of herbal remedies have not shown consistent benefit.21,22
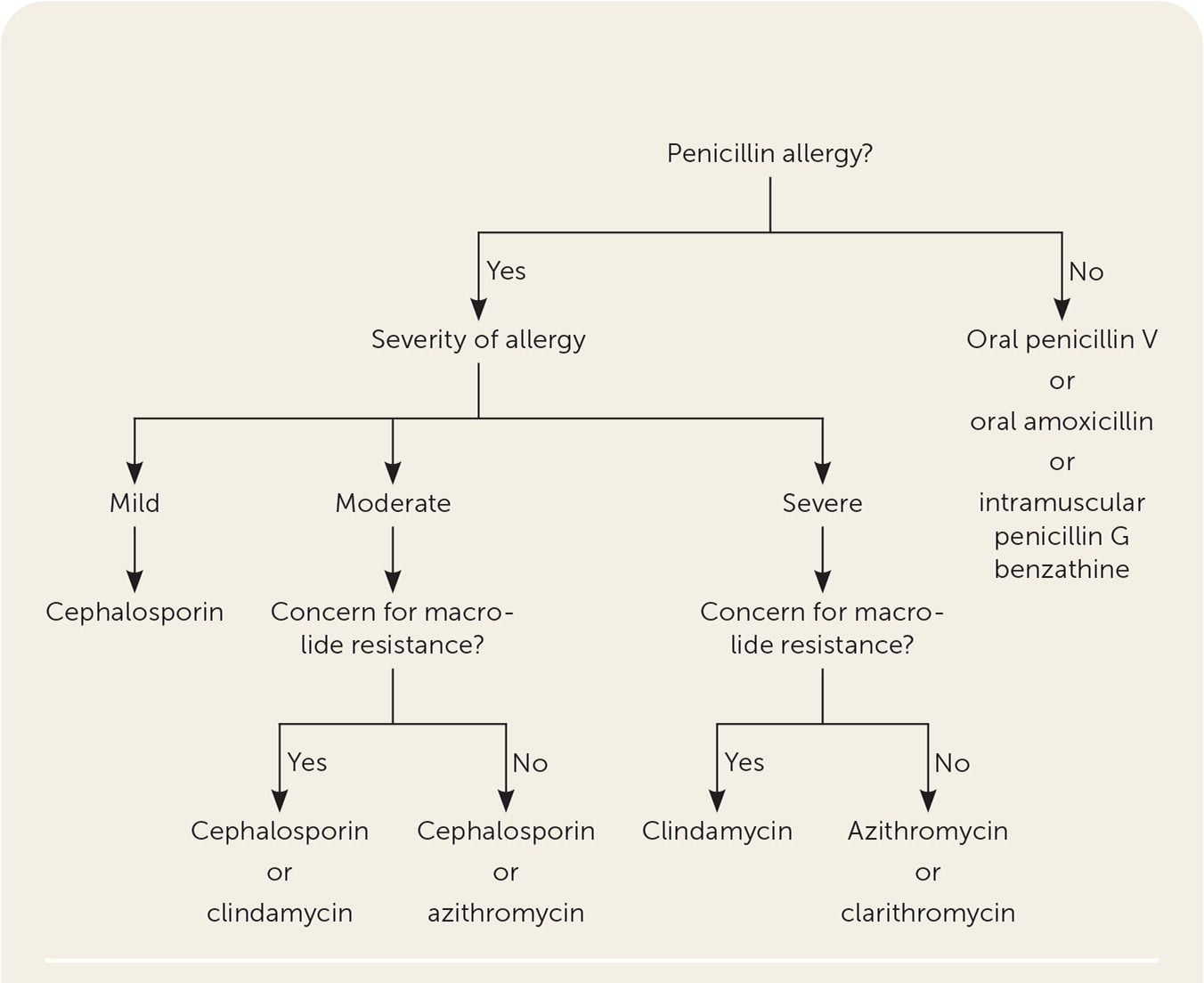
If a patient tests positive for GABHS infection, antibiotics are the recommended treatment, and penicillin is the first-line agent.13,23–25 Table 2 summarizes antibiotic therapy in adults and children.13,23,24,26 For patients who report a history of a penicillin reaction, physicians can use the PEN-FAST score (penicillin allergy, five or fewer years ago, anaphylaxis/angioedema, severe cutaneous adverse reaction, and treatment required for allergy episode) to identify patients at low-risk of penicillin allergies.27 In those with a true penicillin allergy, treatment with a macrolide or cephalosporin has been shown to be as effective as penicillin (Figure 213,28 ). Although a meta-analysis suggests that treating children with a cephalosporin instead of penicillin leads to significantly higher bacteriologic and clinical cure rates, a recent Cochrane review found uncertain evidence that there are clinically meaningful differences between antibiotic classes in adults and children.13,24,28
| Antibiotic | Adult dosage | Child dosage | Duration | Cost* |
|---|---|---|---|---|
| Penicillin (first line) | ||||
| Penicillin V | 500 mg two to three times daily | ≤ 27 kg: 250 mg two to three times daily > 27 kg: 500 mg two to three times daily | 10 days | $5 (—) for 30 500-mg tablets |
| Amoxicillin | 250 mg four times daily or 500 mg twice daily or 1,000 mg daily or 775 mg extended-release (Moxatag) once daily | 50 mg per kg once daily (1,000 mg maximum dose) Alternative: 25 mg per kg (500 mg maximum dose) twice daily | 10 days | $2 for 30 250-mg capsules ($163 for 10 Moxatag tablets) |
| Penicillin G benzathine (Bicillin L-A) | 1.2 million units administered intramuscularly | ≤ 27 kg: 600,000 units intramuscularly > 27 kg: 1.2 million units intramuscularly | One injection | — ($200) |
| Cephalosporins (alternatives for mild to moderate penicillin allergy) | ||||
| Cephalexin | 500 mg twice daily | 40 mg per kg per day divided into twice daily doses (500 mg maximum dose) | 10 days | $5 (—) for 20 500-mg capsules |
| Cefadroxil | 1,000 mg daily | 30 mg per kg once daily or divided into twice daily doses (1,000 mg maximum dose) | 10 days | $5 (—) for 20 500-mg capsules |
| Cefuroxime | 250 mg twice daily | 10 mg per kg per dose twice daily (250 mg maximum dose) | 10 days | $5 (—) for 20 250-mg tablets |
| Cefpodoxime | 100 mg twice daily | 5 mg per kg per dose twice daily (100 mg maximum dose) | 5 to 10 days | $30 (—) for 20 100-mg tablets |
| Cefdinir | 300 mg twice daily or 600 mg daily | 7 mg per kg per dose twice daily or 14 mg per kg once daily (600 mg maximum dose) | 5 to 10 days for 300 mg 10 days for 600 mg | $7 (—) for 20 300-mg capsules |
| Macrolides (alternatives for severe penicillin allergy) | ||||
| Azithromycin (Zithromax) | 12 mg per kg per day (500 mg maximum dose) | 12 mg per kg per day (500 mg maximum dose) | 5 days | $7 ($18) for 5 500-mg tablets |
| Clarithromycin | 250 mg twice daily | 7.5 mg per kg per dose twice daily (250 mg maximum dose) | 10 days | $6 (—) for 20 250-mg tablets |
| Lincosamide (alternative for severe penicillin allergy and concern for macrolide resistance) | ||||
| Clindamycin (Cleocin) | 300 mg three times daily | 7 mg per kg per dose three times daily (300 mg maximum dose) | 10 days | $8 ($12) for 30 300-mg capsules |
Treatment of recurrent tonsillitis (i.e., five or more episodes in one year) includes watchful waiting or surgical management with tonsillectomy.4 The American Academy of Otolaryngology–Head and Neck Surgery outlines criteria for surgical management decision-making, which are endorsed by the American Academy of Family Physicians.30,31 Watchful waiting is strongly recommended if there have been less than seven episodes in the past year, less than five episodes per year in the past two years, or less than three episodes per year in the past three years. Tonsillectomy has been shown to provide mostly short-term benefits such as a decrease in absence from school and number of days with sore throat, with those benefits diminishing after one year.30,32
COMPLICATIONS
Although rare in the developed world, suppurative and nonsuppurative complications of tonsillitis can include abscess, acute glomerulonephritis, rheumatic fever, and scarlet fever.2
Peritonsillar abscess is a collection of pus between the pharyngeal constrictor muscle and tonsillar capsule.33 Symptoms include fever, sore throat, dysphagia, trismus, and a “hot potato” voice.34 On examination, the physician may see a palatine bulge lateral to the tonsil. Peritonsillar abscess is most commonly a complication of streptococcal tonsillitis.33 Although the two are clinically distinct, antibiotic treatment for tonsillitis reduces abscess development.35 Treatment for peritonsillar abscess includes a combination of corticosteroids, antibiotics, and drainage.34
Poststreptococcal glomerulonephritis is an immune-mediated disease caused by nephritogenic strains of GABHS. Presentation can vary from asymptomatic microscopic hematuria to nephritic syndrome with edema, hypertension, acute kidney injury, elevated inflammatory markers, and low complement levels. Children are most often affected, whereas older adults tend to have a worse prognosis. Most patients will have spontaneous resolution of symptoms with return to baseline kidney function. Although antibiotics do not alter the disease course, they may decrease disease transmission.36
Rheumatic fever is an inflammatory, immunologic disease that occurs after infection with GABHS. The prevalence in developing nations is reported to be as high as 5.7 per 1,000 cases of tonsillitis.36 The disease affects multiple organ systems but most commonly causes migratory arthritis of large joints. Nearly 50% of patients have heart involvement manifesting as valvular pathology, with the mitral valve most commonly affected.36 Treatment involves antibiotic therapy to eradicate GABHS and specific therapy for the affected organ system.37
Scarlet fever is a diffuse, blanchable, erythematous eruption with associated papules described as a sandpaper-like rash. It typically starts in the flexural areas and spreads throughout the body, usually sparing the palms and soles, and ultimately desquamates. Scarlet fever results from a delayed-type skin reaction to pyogenic exotoxin produced by Streptococcus pyogenes. Treatment of scarlet fever is the same as standard tonsillitis treatment without specific treatment for the rash itself.38
Tonsilloliths
Tonsilloliths, or tonsillar stones, are products of calcified accumulates of food, cellular debris, and microorganisms in deep invaginations on the surface of the tonsils.39 Tonsilloliths smaller than 5 mm are common, and tonsilloliths larger than 5 mm are rare.40 The exact mechanism of tonsillolith development is not well understood but may be related to recurrent tonsillitis.39
CLINICAL MANIFESTATIONS

DIAGNOSIS
Tonsilloliths are usually diagnosed with physical examination alone. If diagnosis is uncertain, particularly if the stone has not extruded or is large, computed tomography of the oropharynx can be helpful; this would reveal a radiopaque, calcified, cylindrical or round lesion in the tonsillar tissue or fossa.42 Panoramic radiographs can also be used to identify tonsilloliths.43
TREATMENT
COMPLICATIONS
Complications from tonsilloliths are rare and described in literature as case reports. Large tonsilloliths can cause compression and displacement of nearby structures and necrosis of the compressed tissue.45
Data Sources: A PubMed search was completed using the key terms tonsillitis and tonsilloliths. It included books, clinical trials, meta-analyses, randomized controlled trials, and reviews. The National Institute for Health and Care Excellence guidelines, the Cochrane Database of Systematic Reviews, and Essential Evidence Plus were also searched. Search dates: December 23, 2021; January 7, 2022; January 28, 2022; and November 11, 2022.
