
Am Fam Physician. 2023;107(2):193-194
Author disclosure: No relevant financial relationships.
A 49-year-old man presented to the emergency department after waking up with a mild headache, lightheadedness, and loss of balance that resulted in two falls. He had chest discomfort but no chest pain, palpitations, or shortness of breath. He had no significant medical history and took no prescription or herbal medications.
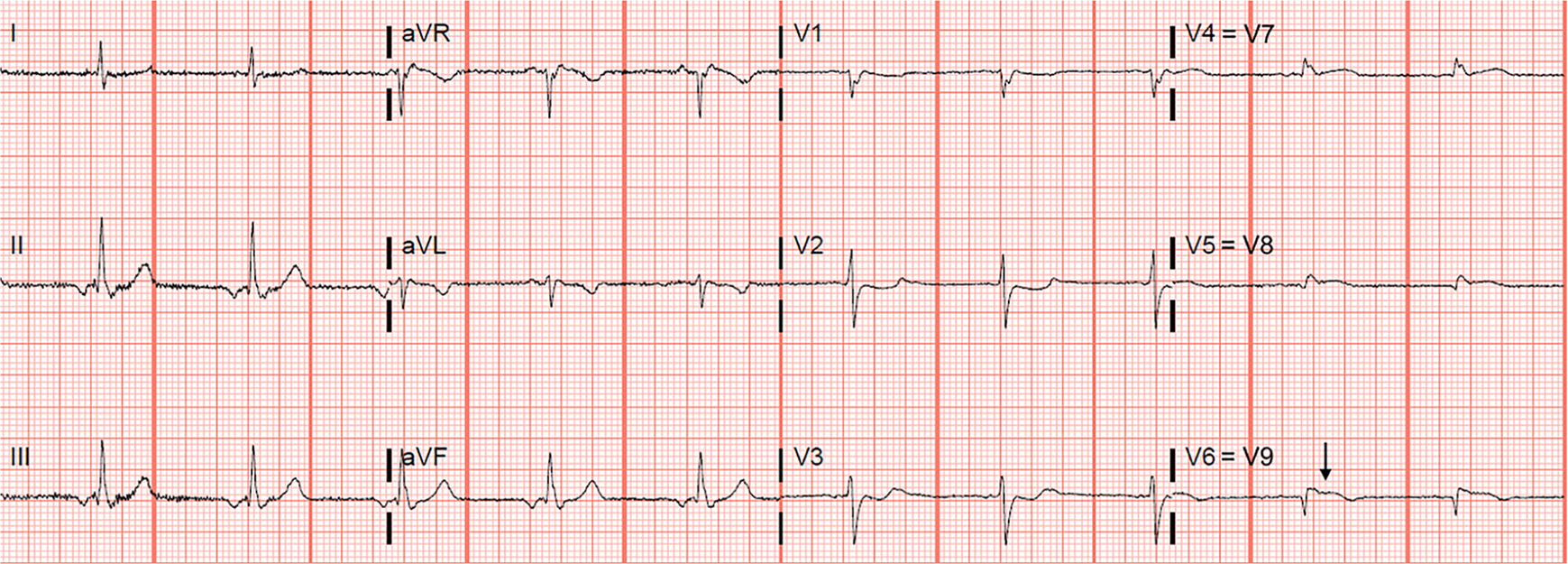
His initial vital signs were blood pressure of 70/30 mm Hg, pulse of 54 beats per minute, temperature of 97.3°F (36.3°C), respiratory rate of 18 breaths per minute, and oxygen saturation of 99% on room air. His physical examination was notable only for cool distal extremities and his cardiac examination was unremarkable. Electrocardiography (ECG) was performed (Figure 1).

Question
Based on the patient's history, physical examination, and initial ECG findings, which one of the following is the most likely diagnosis?
A. de Winter pattern.
B. Digitalis effect.
C. Hypokalemia.
D. Left ventricular hypertrophy with repolarization abnormality.
E. Posterior myocardial infarction.
Discussion
The answer is E: posterior myocardial infarction. This patient presented with bradycardia and hypotension. An emergent differential diagnosis for bradycardia and hypotension uses the DIE acronym: drugs (e.g., digoxin, calcium channel blockers, beta blockers), ischemia, and electrolyte changes (especially hyperkalemia and hypokalemia). In this patient, damage was to the posterior myocardial wall, which typically involves the area supplied by the right coronary artery but less commonly involves the left circumflex coronary artery. Emergent cardiac catheterization revealed that this patient's left circumflex coronary artery was 100% occluded. An isolated posterior myocardial infarction is uncommon, representing an estimated 3% of all myocardial infarctions. However, the posterior wall is involved in 15% to 21% of ischemic events affecting other myocardial areas.1
Patients with myocardial infarction may describe chest discomfort rather than pain.2 Additional symptoms such as shortness of breath, nausea, and epigastric pain may be present. The initial ECG in patients with isolated posterior myocardial infarction shows ST depressions in the anterior leads (V1 through V4) with reciprocal ST elevations in posterior leads V7 through V9, which are placed on the posterior chest wall (Figure 2). Due to the loss of voltage secondary to measuring the posterior aspect of the heart, an ST elevation as small as 0.5 mm in a single posterior lead should raise concern for posterior myocardial infarction.1,3 Greater ST depressions in leads V1 through V4 vs. lead V5 or V6 are highly concerning for posterior myocardial infarction.4
de Winter pattern is associated with occlusion of the left anterior descending artery and is considered an equivalent to ST elevation myocardial infarction, requiring immediate coronary reperfusion. The pattern has upsloping ST depressions with peaked T waves in leads V1 through V6 with reciprocal ST elevation of at least 0.5 mm in lead aVR. Although this patient's case was more consistent with posterior myocardial infarction, occlusion of the left anterior descending coronary artery would have been seen on catheterization.
Digitalis effect is typically a result of digoxin exposure. It presents as PR prolongation and scooped ST depressions, known as the Salvador Dali mustache, which is best seen in the lateral leads I, aVL, V5, and V6. Digitalis effect indicates drug presence, not toxicity.5 This patient had no history of ingesting digoxin or herbal supplements, and his ST depressions were best seen in the anterior leads.
Hypokalemia can cause a variety of ECG patterns due to potassium's critical role in cardiac conduction. ECG changes associated with potassium concentrations less than 2.7 mEq per L (2.7 mmol per L) include PR and QT prolongation, U waves, flattened and inverted T waves, and ST depressions. These changes are most often seen in the anterior leads.6 The patient did not have the widened intervals classically associated with hypokalemia.
Left ventricular hypertrophy is a common ECG finding resulting from increased pressure on the left ventricle, often caused by hypertension or valvular pathology. Left ventricular hypertrophy with repolarization abnormality (strain pattern) presents as ST elevations in the anterior leads and ST depressions primarily in the lateral leads. This patient's ECG findings did not meet the criteria for left ventricular hypertrophy, and the ST depressions were primarily in the anterior leads.7
| Condition | Echocardiograph findings |
|---|---|
| de Winter pattern | Upsloping ST depressions with peaked T waves in leads V1 through V6 with reciprocal ST elevation of at least 0.5 mm in lead aVR |
| Digitalis effect | PR prolongation and scooped ST depressions (known as Salvador Dali mustache), which is best seen in the lateral leads |
| Hypokalemia | PR and QT prolongation, U waves, flattened and inverted T waves, ST depressions |
| Left ventricular hypertrophy with repolarization abnormality | Left ventricular hypertrophy with ST elevations in the anterior leads and ST depressions in the lateral leads |
| Posterior myocardial infarction | ST depressions in the anterior leads (V1 through V4) with reciprocal ST elevations in posterior leads V7 through V9 |
