
Am Fam Physician. 2023;107(5):474-485
Author disclosure: No relevant financial relationships.
A limp is a deviation from normal gait pattern, with pain as the presenting feature in about 80% of cases. The differential diagnosis is broad and includes congenital/developmental, infectious, inflammatory, traumatic (including nonaccidental), and, less commonly, neoplastic etiologies. Transient synovitis of the hip is the cause of a limp in the absence of trauma in 80% to 85% of children. It can be differentiated from septic arthritis of the hip by the absence of fever or ill-appearance and with laboratory testing that shows normal or only mildly elevated inflammatory markers and white blood cell count. If septic arthritis is suspected, joint aspiration should be performed urgently with ultrasound guidance and the aspirated fluid sent for Gram staining, culture, and cell count. Patient history, such as breech presentation at birth, and a leg-length discrepancy on physical examination may suggest developmental dysplasia of the hip. Pain reported primarily at night can occur with neoplasms. Hip pain in an adolescent who is overweight or has obesity may suggest slipped capital femoral epiphysis. Knee pain in an active adolescent may suggest Osgood-Schlatter disease. Radiography shows the degenerative femoral head changes in Legg-Calvé-Perthes disease. Abnormalities in bone marrow shown on magnetic resonance imaging indicate septic arthritis. A complete blood count with differential, erythrocyte sedimentation rate, and C-reactive protein should be obtained if infection or malignancy is suspected.
A limp is a deviation from normal gait pattern and is usually caused by pain, weakness, or deformity.1 The incidence of limping is 1.8 per 1,000 children presenting to an emergency department and 1.5 per 1,000 children presenting to primary care with nontraumatic hip pathology. Pain is the presenting feature in about 80% of cases.2,3 Table 1 lists common etiologies of a limp in children.

| Toddler (younger than 3 years) | Child (3 to 10 years of age) | Adolescent (11 to 19 years of age) | Any childhood age |
|---|---|---|---|
| Cerebral palsy Clubfoot Congenital Achilles contracture Hand-foot-and-mouth disease (enterovirus infection) Immunization reaction Leg-length discrepancy Nonaccidental trauma Toddler fracture Vertical talus | Baker cyst Dermatomyositis Köhler bone disease Legg-Calvé-Perthes disease Leukemia Myositis Tarsal coalition | Chondromalacia patellae Hypermobility syndrome Osgood-Schlatter disease Osteochondritis dissecans Overuse syndromes Slipped capital femoral epiphysis Sprain or strain Tendinopathy Tumor | Cellulitis Contusion Developmental dysplasia of hip Foreign body in foot Fracture Juvenile idiopathic arthritis Lyme disease arthritis Osteomyelitis Reactive arthritis Septic arthritis Transient synovitis |
Antalgic gait describes a gait pattern that reduces weight-bearing pain on one leg by shortening the stance phase of gait relative to the swing phase. Nonantalgic gait is also a deviation from the normal gait pattern but is distinguished by the absence of pain. Patterns of nonantalgic gait include toe walking, circumduction (semicircular leg movement at the hip), steppage (an inability to dorsiflex the ankle, resulting in dragging of the foot), or Trendelenburg gait (pelvic tilting). Familiarity with normal walking patterns in children at various ages helps recognize deviations. Toddlers normally have a wide-based walk with short steps and uncoordinated arm motion, preschoolers develop fluidity in stride and reciprocal arm motion, and children seven years and older walk as adults.4
History
Transient synovitis of the hip is the cause of limping in children in the absence of trauma in 80% to 85% of cases. It occurs in 3% of all children and may be related to a past viral infection.5,6 Sports and recreation injuries leading to a limp are common, with an annual rate of 77 per 1,000 children five to 19 years of age. One-half of these injuries result in treatment at an outpatient office or health clinic rather than the emergency department, and 42% of these injuries are to the lower extremities.7 If the explanation for the limp is vague or inconsistent with the patient's age or the severity and nature of the injury, nonaccidental trauma should be considered.8 The child and caregivers should be interviewed, preferably separately, using open-ended questions in a nonaccusatory manner. Social isolation, school closures, and stress from the COVID-19 pandemic have increased the incidence of nonaccidental trauma.9,10
Characteristics of pain and other key features elicited on patient history can narrow the broad differential diagnosis, which includes congenital, infectious, inflammatory, neo-plastic, and traumatic causes (Table 2).

| Etiology | Epidemiology | History | Physical examination findings |
|---|---|---|---|
| Congenital/developmental | |||
| Developmental dysplasia of the hip | 2% to 4% of population | Breech presentation at delivery, family history, firstborn, more common in girls, activity-related hip pain; often asymptomatic | Asymmetrical gluteal and thigh skinfolds, limited abduction of the hip, leg-length discrepancy, positive Trendelenburg test, positive Galeazzi test (Figure 1) |
| Duchenne muscular dystrophy | 3 to 6 per 100,000 boys | Limp may be a “waddle”; new weakness and limp in a child who was meeting developmental mile-stones in strength and motor skills | Calf hypertrophy; weakness in the trunk and proximal lower limbs; Gowers sign |
| Hypermobile Ehlers-Danlos syndrome or hypermobility spectrum disorders | 0.1% to 3.4% of population | Activity-related pain; progressive chronic pain and other symptoms such as fatigue, functional gastrointestinal disorders, paresthesias, and pelvic dysfunction | Hyperextension or hyperflexibility of joints; hyperextensible skin |
| Köhler bone disease (avascular necrosis of navicular bone) | Incidence < 2% | Midfoot pain; five times more likely in boys than girls | Tenderness at medial aspect of navicular bone in foot |
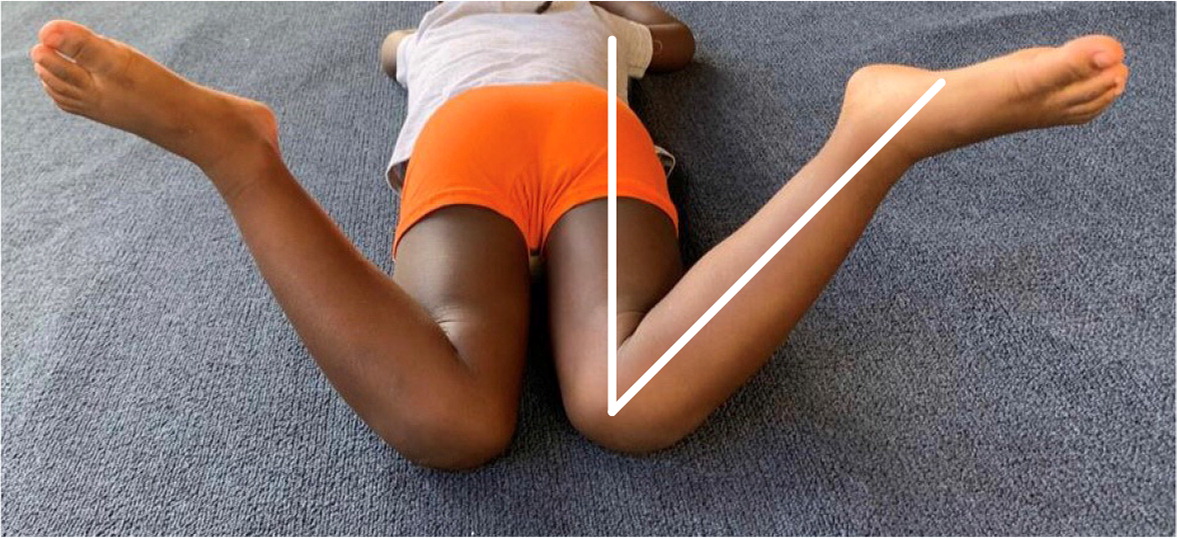
| Legg-Calvé-Perthes disease (avascular necrosis of the hip) | 1 to 11 per 100,000 children | Five times more common in boys than girls; afebrile, does not appear ill; onset of limp and pain over weeks to months; pain intensifies during and after physical activity | Pain with internal rotation, flexion, and abduction of hip; positive Galeazzi test; loss of internal rotation of the hip (Figure 2); bilateral in 10% to 24% of patients |
| Slipped capital femoral epiphysis | 4.8 cases per 100,000 children | Obesity; endocrine, metabolic, or renal disorders; more common in boys | Loss of internal rotation of the hip, obligate external rotation when the hip is flexed; painful range of motion in the knee |
| Infectious | |||
| Gonococcal arthritis | Genital infection rate of 350 to 600 per 100,000 adolescents (15 to 19 years of age); joint involvement is rare | Constant pain, sexually active; vaginal or urethral discharge; dysuria | Painless, nonpruritic maculopapular or vesicular skin rash; unilateral joint swelling, usually of the knees, ankles, or feet; tenosynovitis |
| Lyme disease arthritis | 4% to 12% per 100,000 children (likely underreported), with 50% of untreated cases developing arthritis | Tick bite, history of a bullseye rash, residency in or travel to endemic area three or more months earlier (joint involvement is a late manifestation of disseminated disease) | Swollen joint (typically the knee), usually able to bear weight |
| Osteomyelitis | 9 per 100,000 children | Fever, subacute presentation | Localized bony tenderness, overlying warmth, swelling, and redness |
| Septic arthritis | 4 to 5 cases per 100,000 children per year | Refusal to bear weight, fever, onset over three to five days; twice as common in boys than girls | Toxic appearance, overlying warmth, redness, and pain of affected joint through entire range of motion; joint is flexed with limited range of motion; if the involved joint is the hip, it is usually flexed, abducted, and externally rotated (Figure 4) |
| Transient synovitis | Average annual incidence for children is 0.2%; childhood risk of at least one episode is 3% | May have had recent upper respiratory tract or viral gastrointestinal infection | Groin or thigh pain; affected hip is usually flexed, abducted, and externally rotated; pain at the end of range-of-motion arc |
| Inflammatory | |||
| Juvenile idiopathic arthritis | 4 to 400 per 100,000 children | Joint stiffness in the morning or after protracted rest that improves with activity; blurry vision, dry eyes, fatigue, fever, weight loss | Red, swollen, tender, or warm joint; rash; temporomandibular joint involvement |
| Reactive (aseptic inflammatory) arthritis | 1% to 20% occurrence rate of arthritis after infection | Gastrointestinal or urogenital infection | Conjunctivitis, enthesitis, nasopharyngeal infection, oligoarthritis, urethritis; joint swelling, overlying warmth, or redness |
| Neoplasms, benign | |||
| Osteochondroma | Prevalence of 0.44% in people younger than 30 years, usually presents at 10 to 15 years of age | Pain or snapping sensation over bony mass | Hard, immovable bony mass on distal femur or proximal tibia |
| Osteoid osteoma | Rare, but third most common benign bone tumor (11% of cases) | Pain worse with activity and at night; more common in boys; pain relieved by nonsteroidal anti-inflammatory drugs | Palpable lump, usually in the femur, tibia, or fibula |
| Neoplasms, malignant | |||
| Leukemia | Most common childhood cancer, with 4,000 cases per year in the United States; about 3 out of 4 affected children and adolescents are diagnosed with acute lymphocytic leukemia and the remaining cases are mostly acute myeloid leukemia | Anorexia, constant pain even at rest, pain at night, weight loss | Abdominal mass, bony tenderness, hepatosplenomegaly, lymphadenopathy, palpable bony mass |
| Osteosarcoma | Usually affects children and young adults; overall incidence is 4 to 7 cases per 1 million individuals per year | Severe pain, especially at night | Palpable mass, usually on distal femur or proximal tibia |
| Trauma and overuse | |||
| Foreign body or puncture wounds in foot | Extremely common | Stepped on something with sharp pain | Focal redness on the sole of the foot, presence of skin disruption |
| Fracture, acute | Common; 1 in 3 healthy children will break a bone at some point during childhood, usually an upper extremity, but tibia and fibula fractures are also common | Trauma, focal pain, acute onset | Point tenderness in area of concern, focal swelling, ecchymosis; leg-length discrepancy if fracture in pelvis or femur |
| Fracture, avulsion | Exact incidence undetermined, but relatively uncommon | Adolescent athlete in a sport with kicking or running; sudden popping sensation at the site of injury, often the pelvis | Ecchymosis and tenderness with palpation of the anterosuperior or anteroinferior iliac spines |
| Fracture, stress | Common, occurs in up to 50% of runners and 22% to 45% of ballet dancers | Morning stiffness and pain that worsens with activity; insidious onset of pain over several weeks | Point tenderness in area of concern, usually tibia, fibula, or metatarsal bones |
| Iliotibial band syndrome | Up to 10% of runners | Pain over lateral knee, thigh, or hip; worse with running or walking and better with rest | Positive Ober test |
| Nonaccidental trauma | Centers for Disease Control and Prevention reports that at least 1 in 7 children experiences child abuse or neglect every year | Implausible or inconsistent story | Lower extremity fracture in a child who is not yet ambulatory |
| Osgood-Schlatter disease (apophysitis of the tibial tubercle) | Up to 10% to 20% of adolescent athletes | Recent growth spurt; participation in running or jumping sports; pain over tibial tubercle, worsens with activity | Tenderness over tibial tubercle, pain with resisted knee extension |
| Previous growth plate trauma | Undetermined incidence, not common | Recent growth spurt; history of trauma | Leg-length discrepancy |
| Sacroiliac joint pathology | Undetermined incidence, not common | Back pain; adolescent female athletes | Positive Patrick (FABER) test (Figure 5); positive pelvic compression test; pain with palpation at focal site inferomedial to the posterosuperior iliac spine |
| Sever disease (calcaneal apophysitis) | Incidence in general population not established; 2% to 16% of presentations at sports medicine clinics | Participation in sports on hardwood floors or wearing cleats; recent growth spurt; heel pain; toe walking; worse with activity | Tenderness and mild swelling at the calcaneal tendon insertion at the heel; pain with passive ankle dorsiflexion; pain with compression of the posterior calcaneus (squeeze test) and aggravated by standing on tiptoes (Sever sign) |
| Toddler fracture (spiral fracture of tibia) | 0.6 to 2.5 of every 1,000 patients in pediatric emergency departments | Twisting injury or fall | Point tenderness on tibial shaft |
Age. Age factors into the diagnostic process. Pain below the knee in the still-growing adolescent athlete suggests Osgood-Schlatter disease.
Duration of Limp. Insidious onset of pain in the lower leg or foot suggests a stress fracture.11 Chronic limps (i.e., lasting longer than six weeks) can arise from Legg-Calvé-Perthes disease, slipped capital femoral epiphysis (SCFE), or systemic illness (e.g., juvenile idiopathic arthritis [JIA], malignancy). Developmental dysplasia of the hip may be diagnosed after examination of an infant, but it may present with the insidious onset of a limp and groin pain in an adolescent.12
History of Trauma. There is often a clear inciting event, such as a sports injury or fall, although repetitive injuries leading to tendon or ligament disruption may not be as specific.
Nature of Pain. Morning stiffness that improves with activity is a feature of a rheumatologic disorder. Stress fractures can cause morning pain and worsen with activity. Pain at night may indicate a neoplasm.
Sex as Assigned at Birth. Developmental dysplasia of the hip is more common in girls, whereas Legg-Calvé-Perthes disease and SCFE are more common in boys.13
Systemic Signs. Fever accompanied by weight loss, night sweats, and anorexia suggests infection, inflammation (e.g., JIA), or, in rare cases, malignancy.
Physical Examination
OBSERVATION
Children should be assessed for a febrile or toxic appearance or rash, which suggests an infection or inflammatory process. An erythematous, swollen joint suggests an intra-articular cause, including septic arthritis.14 Obesity, especially in the setting of socioeconomic deprivation, may suggest SCFE.15 Leg-length discrepancy may be due to a chronic condition that is congenital, a past growth plate trauma that is unmasked by a growth spurt, or an acute condition such as a fracture of the pelvis or femur, causing a shift in how the child stands or walks. Leg lengths are measured bilaterally from the anterosuperior iliac spine to the ipsilateral medial malleolus or by measuring the distance between each medial malleolus and the sole of the foot.16 In the Galeazzi test, the examiner passively flexes the hips and knees of a supine child (Figure 117). Asymmetry in knee positions suggests leg-length discrepancy and is often used in the evaluation of hip malformation or dislocation. Feet should be examined for excess pronation or supination, foreign bodies, and callouses. Shoes should be inspected for uneven sole wear, which indicates a chronic kinetic imbalance leading to a limp.

PALPATION
Point tenderness, particularly with palpation of a bony step-off, or pain with pressure or manipulation of a joint or limb can occur when a bony mass or fracture is the cause of a limp. Tibial shaft point tenderness in an ambulating child younger than four years should prompt evaluation for a spiral fracture of the tibia known as a toddler fracture.18 Tenderness in the medial aspect of the navicular bone may suggest Köhler bone disease (i.e., osteonecrosis of the navicular bone).19 Pain on palpation of the tibial tubercle in an adolescent suggests Osgood-Schlatter disease.20 Pain with compression of the posterior calcaneus (i.e., squeeze test) may indicate Sever disease (i.e., apophysitis of the calcaneus).21 A hard, fixed mass in a long bone may indicate a benign bone tumor.22,23 Avulsion fractures of the proximal sartorius or rectus femoris can cause ecchymosis and tenderness with palpation of the anterosuperior and anteroinferior iliac spines, respectively.24 Warmth over the hip raises concern for septic arthritis. Fifteen percent of children with leukemia present with a limp, and concomitant diffuse abdominal tenderness raises concern for malignancy, especially when accompanied by organomegaly or lymphadenopathy.25
RANGE OF MOTION
Pain or range-of-motion deficits with internal rotation and abduction of the hip or flexion or extension of the knee can indicate intra-articular hip pathology such as Legg-Calvé-Perthes disease or SCFE26 (Figure 2). Limitations in hip abduction can be seen with developmental dysplasia of the hip (Figure 327). A child who is preferentially holding their hip in flexion and external rotation, which reduces intracapsular pressure, suggests septic arthritis or transient synovitis (Figure 428). Septic arthritis causes severe pain throughout the full hip range-of-motion arc, whereas pain from transient synovitis may be limited to the end of the hip's motion arc.6 Hyperextension or hyperflexibility of joints in a limping child may indicate hypermobile Ehlers-Danlos syndrome or hypermobility spectrum disorders.29


STRENGTH
The presentation of a child with a limp and loss of strength with resisted hip flexion and abduction suggests weakness in the quadriceps and hip abductors and can be seen in Legg-Calvé-Perthes disease.13 Muscular dystrophy may present with weakness in the trunk and proximal lower limbs, causing the child to use their hands and arms to rise from a sitting or supine position (i.e., Gowers sign).30 Resisted knee extension strength may be reduced in Osgood-Schlatter disease.31
TESTS
Many of the following tests can be viewed in a previous American Family Physician article available at https://www.aafp.org/pubs/afp/issues/2014/0101/p27.html.
Patrick (FABER) Test. The examiner passively flexes, abducts, and externally rotates the hip (Figure 528). Pain suggests sacroiliac joint pathology and can occur in adolescent girls due to laxity of the developing pelvic girdle. The condition may present as back pain and a limping gait and may respond to maneuvers to realign the joint.32

Pelvic Compression Test. The examiner pushes the alae (wings) of the pelvis toward each other. Pain suggests sacroiliac joint dysfunction.
Straight Leg Raise. The examiner passively flexes the hip while the patient is supine, keeping the knee extended. Reproduction of radicular pain in the leg is a positive test that suggests disk herniation and nerve compression and is not common in children. Pain in the posterior thigh correlates with hamstring tightness.
FADIR Test. The examiner passively flexes, adducts, and internally rotates the hip. Pain suggests hip impingement or other intraarticular pathology.
Ober Test. With the child lying on one side, assess the ability to lower the knee of the superior leg to the table. Movement that is difficult or reproduces lateral hip pain suggests iliotibial band syndrome. Focal pain to palpation 2 cm proximal to the lateral femoral epicondyle while the examiner passively flexes the knee also suggests iliotibial band syndrome.33
Trendelenburg Test and Gait. An inability to maintain a level pelvis when standing on one leg (pelvis drops toward the unsupported raised leg) is due to weakness of the contralateral hip abductors. This can be observed by gait or asking the child to stand on the affected limb while lifting the contralateral limb off the floor. A positive test may be indicative of developmental dysplasia of the hip, SCFE, Legg-Calvé-Perthes disease, acute or chronic hip dislocation, poliomyelitis, or damage to the superior gluteal nerve.
Laboratory Tests
A complete blood count with differential, erythrocyte sedimentation rate, and C-reactive protein level should be obtained if infection or malignancy is suspected. Antinuclear antibodies should be measured if inflammatory arthritis is suspected. If the child has a rash and history of a tick bite, a two-step serologic analysis with an enzyme immunoassay and reflexive immunoblotting has a sensitivity of 70% to 100% and a specificity greater than 95% for disseminated Lyme disease.34 However, an alternative strategy of using two different enzyme immunoassays without an immunoblot is a more rapid and economical testing strategy in children.35 If septic arthritis is suspected, joint aspiration should be performed urgently with ultrasound guidance and the aspirated fluid sent for Gram staining, culture, and cell count. A delay in the diagnosis and treatment of septic arthritis can lead to cartilage damage 12 hours after onset and may be irreversible within one to two days.36 A procalcitonin measurement may have greater diagnostic value than C-reactive protein levels in distinguishing septic from nonseptic arthritis.37 Blood cultures should be obtained if osteomyelitis is suspected because it is increasing in incidence and can be caused by contiguous spread of infection from adjacent soft tissues and joints, hematogenous seeding, or direct inoculation of bacteria into the bone as a result of trauma or surgery.38,39
Imaging
The American College of Radiology Appropriateness Criteria were established for initial imaging of children younger than five years with an acute limp. These recommendations are broken into five clinical presentation variants based on the localization of symptoms, presence of pain, and concern for infection. Various initial imaging modalities are classified under each variant as “usually appropriate,” “may be appropriate,” or “usually not appropriate” based on the likely yield of the study and the amount of radiation exposure.40
Nonlocalized symptoms and no concern for infection. Bilateral radiography of the tibia and fibula is usually appropriate, and radiography of the femurs may be appropriate for initial imaging.
Pain and localized symptoms and no concern for infection. Radiography of the lower extremity area of interest is usually appropriate for initial imaging.
Nonlocalized symptoms and concern for infection. Magnetic resonance imaging (MRI) of the lower extremity of interest, with and without intravenous contrast, or MRI of the lower extremity without contrast is usually appropriate. Whole-body MRI, ultrasonography of the hips, or technetium-99m bone scan of the pelvis and lower extremity (i.e., bone scintigraphy) may be appropriate for initial imaging.
Symptoms localized to the hip and concern for infection. Ultrasonography of the hip, pelvic MRI without intravenous contrast, or pelvic MRI with and without intravenous contrast is usually appropriate, whereas radiography of the pelvis or bone scintigraphy may be appropriate.
Symptoms localized to the lower extremity but not in the hips or pelvis and concern for infection. MRI of the lower extremity area of interest without intravenous contrast, or MRI of the lower extremity area with and without intravenous contrast is usually appropriate, whereas ultrasonography or radiography of the lower extremity area of interest may be appropriate.
RADIOGRAPHY
Radiography is the most common initial imaging modality in the evaluation of a limping child. In children younger than five years who do not show signs of infection, antero-posterior and lateral radiography of the bilateral tibia and fibula is recommended, because the most common etiology of a limp is minor trauma to the lower leg.40 If initial radiography is negative but suspicion persists, radiography should be repeated because a periosteal reaction may take up to two to three weeks to be seen and occurs in 45% of toddler (tibial shaft) fractures.18,41 In older children, imaging is ordered based on findings from history and examination.
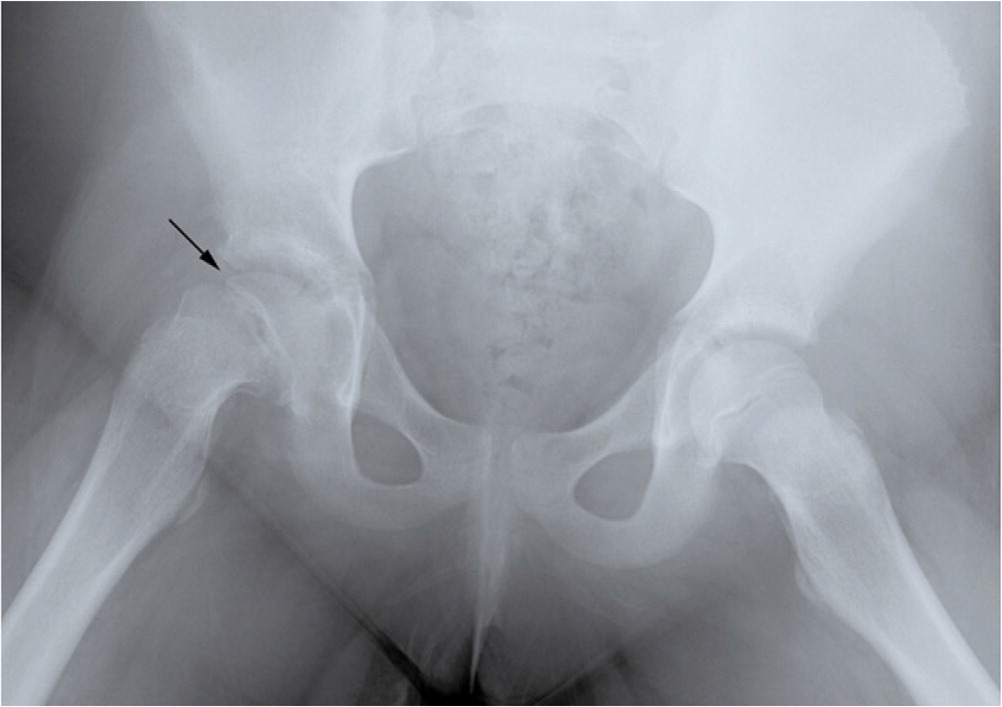
Anteroposterior and frog-leg lateral films of the hip will reveal the classic sclerosis, fragmentation, and flattening of the proximal femoral epiphysis in Legg-Calvé-Perthes disease (avascular necrosis of the femoral head), although these findings may not be present in early disease. Developmental dysplasia is seen as chronic hip dislocation on radiography and requires careful review because the radiographic anomalies may be symmetrical and therefore not immediately obvious. Hip radiography shows displacement of the femoral head with respect to the femoral neck in SCFE (Figure 617).
ULTRASONOGRAPHY
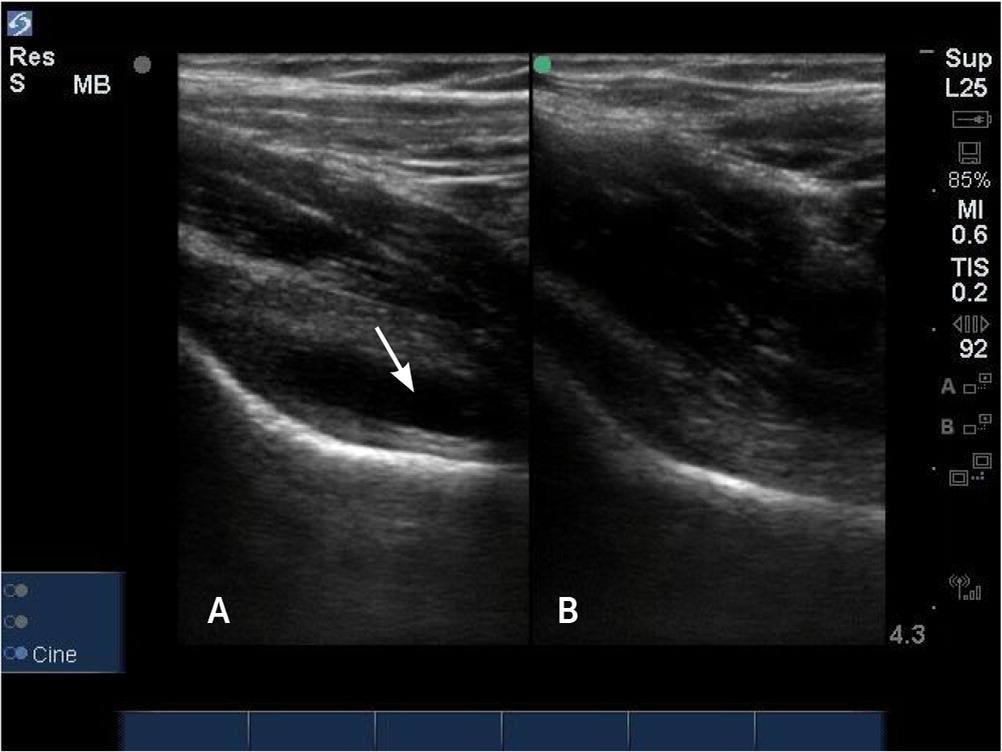
Although plain film radiography may detect osteomyelitis, fractures, or malignancy, its sensitivity for identifying effusions is low.42,43–46 A hip effusion appears as a hypoechoic area underneath the hip capsule (Figure 7). Clinicians can become proficient in POCUS with minimal training.44 False-negative findings on ultrasonography are higher when symptoms have been present for less than 24 hours or if the child is younger than one year.47 When effusions are present, POCUS can be used for ultrasound-guided fluid aspiration for analysis and culture, which is important for timely treatment of septic arthritis. Ultrasonography may reveal foreign bodies, abscesses, and ligament strains; the trained eye may also detect subtle cortical irregularities of a stress fracture and periosteal hematoma in the setting of a fracture.18,46
BONE SCINTIGRAPHY
Bone scintigraphy is highly sensitive and specific in detecting femoral head avascular necrosis and stress fractures.48,49 Legg-Calvé-Perthes radiographic changes may not be present in early disease but may be seen on a bone scan where minimal bone turnover can be detected.50 The use of bone scintigraphy is limited by cost and exposure to radiation, but it can demonstrate metastatic lesions, osteomyelitis, joint infections, and occult or stress fractures.
MAGNETIC RESONANCE IMAGING
Despite the high cost, MRI is a preferred alternative to bone scintigraphy because of its higher resolution and absence of ionizing radiation. MRI has high accuracy for detecting septic arthritis and osteomyelitis (Figure 817) and may be appropriate as an initial imaging study when there is concern for infection.51 The finding of joint effusions in the symptomatic and contralateral (i.e., asymptomatic) hip with the absence of signal intensity abnormalities in localized bone marrow is suggestive of transient synovitis. Signal intensity alteration and enhancement in soft tissue and bone marrow around the hip are suggestive of septic arthritis, myositis, abscess, or tumor.52

Diagnostic Dilemmas
DIFFERENTIATING INFECTION FROM INFLAMMATION
Transient synovitis of the hip is the most common nontraumatic cause of a limp in children and is a benign, self-limited condition, whereas septic arthritis of the hip can cause catastrophic damage to the hip cartilage and femoral head blood supply within hours of infection onset. Children with septic arthritis appear toxic with a flexed and externally rotated hip to relieve pain. The Kocher Criteria for Septic Arthritis (https://www.mdcalc.com/kocher-criteria-septic-arthritis) use clinical features to distinguish transient synovitis from septic arthritis. Fever, non–weight-bearing, an erythrocyte sedimentation rate of more than 40 mm per hour, and a white blood cell count of more than 12,000 per μL (12 × 109 per L) are suggestive of septic arthritis.53 A C-reactive protein level of more than 2 mg per dL (20 mg per L) further suggests the diagnosis of septic arthritis.54 Prediction tools are not externally validated and may not be reliable in low-risk populations.55
Up to 50% of patients with untreated cases of Lyme disease will develop arthritis, usually of the knees and less commonly the hip.56,57 There is clinical similarity between septic arthritis of the hip, Lyme arthritis, and transient synovitis. Lyme disease should be considered in children with a limp due to monoarticular arthritis, especially in endemic regions in the United States, such as New England, the upper Midwest, and the Pacific Northwest.58 Compared with septic arthritis, Lyme disease arthritis is less often accompanied by fever and local inflammation, has lower levels of inflammatory markers and peripheral blood count, and on examination the patient has less of an aversion to weight-bearing.59,60 Reactive arthritis refers to an infection-induced systemic illness and is characterized by aseptic inflammatory joint involvement occurring in a patient with a bacterial infection localized in a distant organ system.61
DIFFERENTIATING NEOPLASMS FROM JUVENILE IDIOPATHIC ARTHRITIS
A limp may be a presenting symptom of JIA or cancer, which can pose a diagnostic dilemma because systemic signs such as fever, fatigue, hepatosplenomegaly, and rash may be present in both conditions. Leukemia may present with joint pain and swelling similar to JIA in 15% to 30% of cases early in the disease when peripheral blood changes are subtle or absent.25,62,63 The presence of a low-normal platelet count, low white blood cell count (even if blasts are not yet present), and nighttime pain is suggestive of leukemia and indicates that an oncology referral should be considered.64 Although leukemia is the most common childhood and adolescent cancer, it is rare in primary care and emergency departments, with 4,000 cases per year in the United States.65 Most childhood leukemia (75%) is acute lymphocytic leukemia and is more common in boys than girls.66 Rarely, a limp can be a symptom of a bony tumor.62
The incidence of JIA is 4 to 400 per 100,000 children.67 Limping due to asymmetrical arthritis may be the predominant presentation in the oligoarticular subtype of JIA, which is the most common type. It is more common in girls with onset before six years of age.68 The knee joint is most affected, followed by the ankles. Laboratory tests for rheumatoid factor, antinuclear antibodies, and the HLA-B27 antigen can be useful in confirming JIA.69
This article updates previous articles on this topic by Naranje, et al.28; Sawyer and Kappor17; and Leet and Skaggs.70
Data Sources: A PubMed search was completed in Clinical Queries using the key terms limping child, arthritis in children, septic arthritis, child abuse, transient synovitis, Lyme arthritis, hip ultrasound, and imaging in limp. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. We also searched DynaMed, the Cochrane database, Google Scholar, Essential Evidence Plus, and Medline. Search dates: October 2021 through July 2022, and March 2023.
